What is traumatic glaucoma?
Traumatic glaucoma is a type of secondary glaucoma that develops after an eye injury. This condition can result from blunt trauma, penetrating injuries, or chemical burns that damage the ocular structures, causing elevated intraocular pressure (IOP). If not treated promptly and effectively, the increase in IOP can lead to optic nerve damage and vision loss.
Traumatic glaucoma’s pathophysiology is complex. Angle recession, or damage to the eye’s drainage angle, can result in impaired aqueous humor outflow and elevated IOP. Penetrating injuries may introduce foreign bodies or cause structural damage, which also affects drainage pathways. Inflammation and bleeding inside the eye can also cause secondary glaucoma by obstructing the trabecular meshwork, the eye’s drainage system. Over time, persistently elevated IOP can cause irreversible optic nerve damage and vision impairment.
The symptoms of traumatic glaucoma vary depending on the cause and severity of the injury, but they frequently include eye pain, redness, blurred vision, halos around lights, and, in some cases, nausea or vomiting. Early detection and intervention are critical to avoiding long-term consequences. A comprehensive eye examination, including IOP measurement, gonioscopy to examine the drainage angle, and imaging studies to assess the extent of the damage, is usually required to make a diagnosis. Understanding the underlying causes and mechanisms of traumatic glaucoma is critical for devising effective treatment plans.
Traditional Approaches to Traumatic Glaucoma Treatment
The management and treatment of traumatic glaucoma necessitates a comprehensive approach that addresses the underlying cause, lowers IOP, and protects the optic nerve from further damage. Medical and surgical interventions are standard treatments for traumatic glaucoma.
Medical Management
Medical management is frequently the first option for controlling elevated IOP in traumatic glaucoma. This entails the use of several types of medications, including:
- Beta-blockers: These drugs, such as timolol, reduce aqueous humor production, lowering IOP. They are frequently used as initial therapy due to their efficacy and low side effects.
- Prostaglandin Analogs: Drugs such as latanoprost and bimatoprost increase the outflow of aqueous humor via the uveoscleral pathway, lowering IOP. They are extremely effective and widely used in glaucoma treatment.
- Alpha Agonists: Brimonidine and other drugs reduce aqueous humor production while increasing uveoscleral outflow. They can be used along with other medications to improve IOP control.
- Carbonic Anhydrase Inhibitors: These drugs, which include dorzolamide and acetazolamide, reduce aqueous humor production. They are available in both topical and oral formulations.
- Miotics: Pilocarpine, a miotic agent, stimulates aqueous humor outflow by contracting the ciliary muscle and opening the trabecular meshwork. However, it is less commonly used due to its side effects and the availability of more effective medications.
Surgical Treatment
When medical treatment fails to control IOP or there is significant structural damage, surgical intervention may be required. Common surgical procedures for traumatic glaucoma are:
- Trabeculectomy: This surgery opens up a new drainage pathway for aqueous humor to exit the eye, bypassing the damaged trabecular meshwork. It is highly effective in lowering IOP, but there are risks of infection and scarring.
- Drainage Implants: Devices such as the Ahmed or Baerveldt implants are inserted into the eye to improve aqueous humor drainage. These implants are useful when traditional surgery fails or is not an option.
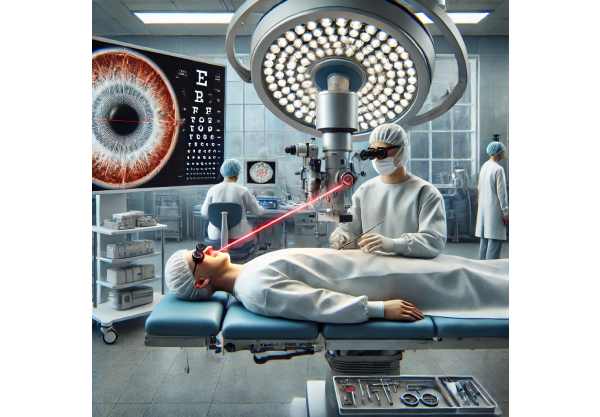
- Laser Trabeculoplasty: Laser procedures like argon laser trabeculoplasty (ALT) and selective laser trabeculoplasty (SLT) improve aqueous outflow by targeting the trabecular meshwork. They are minimally invasive and can be completed as an outpatient procedure.
- Cyclophotocoagulation: This laser treatment reduces aqueous humor production by focusing on the ciliary body. It is frequently used in refractory cases where other treatments have been ineffective.
Supportive Care and Monitoring
Ongoing monitoring and supportive care are essential for treating traumatic glaucoma. Regular follow-up visits to measure IOP, assess optic nerve health, and evaluate visual function are critical for detecting changes early and adapting treatment as needed. Patients should also avoid activities that may raise IOP, such as heavy lifting or straining.
Breakthrough Innovations in Traumatic Glaucoma Treatment
Recent advances in the treatment of traumatic glaucoma have resulted in novel approaches that improve the effectiveness, safety, and convenience of this condition. These cutting-edge innovations include novel surgical techniques, advanced drug delivery systems, and emerging technologies that have the potential to transform traumatic glaucoma treatment.
Minimal Invasive Glaucoma Surgery (MIGS)
Minimally invasive glaucoma surgery (MIGS) has changed the surgical landscape for glaucoma treatment, providing safer and less invasive alternatives to traditional procedures. MIGS procedures aim to reduce IOP while causing minimal tissue disruption and allowing for faster recovery times. The key MIGS techniques are as follows:
- iStent and iStent Inject: These small devices are placed in the trabecular meshwork to improve aqueous humor outflow. The iStent Inject, a second-generation device, enables the placement of multiple stents, increasing efficacy. To achieve the best results, these procedures are often combined with cataract surgery.
- Xen Gel Stent: This soft, gelatin-based implant forms a permanent drainage channel between the anterior chamber and the subconjunctival space, thereby lowering IOP. The Xen Gel Stent is a minimally invasive alternative to traditional trabeculectomy.
- Hydrus Microstent: This flexible device is placed in Schlemm’s canal to improve outflow via natural drainage pathways. Its purpose is to provide a long-term reduction in IOP with a low risk of complications.
- Cycloablation Techniques: Procedures like MP-TSCPC and HIFU target the ciliary body to reduce aqueous humor production. These methods are less invasive and provide accurate, controlled treatment.
Sustained-release drug delivery systems.
Advances in drug delivery technology have resulted in the creation of sustained-release systems that provide long-term IOP control with fewer side effects and higher patient compliance. Notable innovations are:
- Durysta (Bimatoprost Implant): This biodegradable implant is inserted into the anterior chamber and gradually releases bimatoprost over several months. Durysta provides a convenient and long-lasting alternative to daily eye drops.
- Travoprost Punctal Plug Delivery System: This novel system injects travoprost into the tear duct via a punctal plug. The drug slowly releases over time, resulting in consistent IOP reduction without the need for daily administration.
- Mati Therapeutics’ Evolute: This scleral plug delivery system is intended to provide sustained latanoprost release for up to six months. It represents a promising solution for patients who struggle to adhere to topical therapies.
Gene Therapy and Neuroprotection
Emerging fields, such as gene therapy and neuroprotection, hold significant promise for treating traumatic glaucoma.
- Gene Therapy: Researchers are investigating gene-editing technologies such as CRISPR-Cas9 to identify and correct genetic defects that contribute to glaucoma. This method could potentially prevent or reverse optic nerve damage by restoring normal gene function.
- Neuroprotective Agents: Neuroprotection aims to protect the optic nerve from damage while also promoting regeneration. Brimonidine tartrate, memantine, and citicoline are three drugs under investigation for their ability to protect retinal ganglion cells and improve optic nerve health.
Artificial Intelligence, Machine Learning
AI and machine learning are transforming the diagnosis and treatment of traumatic glaucoma:
- AI-Driven Diagnostics: AI algorithms can analyze large datasets of imaging and clinical data to identify patterns and detect glaucoma early on. These tools can help clinicians make accurate diagnoses and track disease progression.
- Predictive Analytics: Machine learning models can predict the risk of glaucoma development and progression based on patient-specific information, allowing for personalized treatment plans and proactive management.
Telemedicine & Remote Monitoring
The integration of telemedicine and remote monitoring technologies is increasing access to glaucoma care and improving patient outcomes.
- Remote IOP Monitoring: Devices like the iCare HOME tonometer enable patients to measure their IOP at home and send the results to their healthcare providers. This allows for continuous monitoring and timely interventions.
- Telehealth Platforms: Telehealth services enable remote consultations with glaucoma specialists, ensuring timely access to expert care, particularly for patients in underserved communities. These platforms enable ongoing management and follow-up without requiring frequent in-person visits.
Stem Cell Therapy and Regenerative Medicine
Advances in stem cell therapy and regenerative medicine provide potential new treatments for traumatic glaucoma.
- Stem Cell-Based Treatments: Scientists are exploring the use of stem cells to regenerate damaged ocular tissues such as the trabecular meshwork and optic nerve. Stem cell therapies could potentially restore normal aqueous humor outflow and protect against future damage.
- Regenerative Medicine: Bioengineered scaffolds and tissue engineering are being used to repair and replace damaged ocular structures. These approaches seek to restore the eye’s natural function while preventing glaucoma progression.






