Vitreoretinal lymphoma (VRL) is a rare and aggressive cancer that begins in the retina and vitreous, which is a gel-like substance that fills the eye. It is considered a subtype of primary central nervous system lymphoma (PCNSL) due to its close association with central nervous system involvement. VRL primarily affects older adults and can pose significant diagnostic and therapeutic challenges due to its enigmatic nature and overlapping symptoms with other ocular conditions.
VRL is characterized by a variety of symptoms, including blurred vision, floaters, and, less frequently, eye pain and redness. These symptoms are frequently mistaken for more common inflammatory eye diseases, delaying an accurate diagnosis. VRL can also cause vitreous opacities, retinal infiltrates, and subretinal lesions, which are visible during an eye exam.
VRL is a complex diagnosis that typically includes a combination of clinical evaluation, imaging studies, and laboratory tests. Optical coherence tomography (OCT) and fundus photography are essential for imaging the retina and vitreous. A vitreous biopsy, which examines a sample of vitreous fluid for malignant cells and specific biomarkers such as interleukin-10 (IL-10), is frequently required for a definitive diagnosis. Advanced imaging techniques and molecular diagnostics have significantly improved the detection and characterization of VRL, allowing for earlier and more accurate diagnosis.
Standard Management for Vitreoretinal Lymphoma
Vitreoretinal lymphoma requires a multidisciplinary approach that includes ophthalmologists, oncologists, and radiologists. The primary goals are to eradicate cancer, preserve vision, and prevent systemic spread. Treatment plans are tailored to each patient’s specific needs, taking into account factors such as the degree of ocular involvement, the presence of systemic disease, and overall health.
Intravitreal Chemotherapy: One of the most important aspects of VRL treatment is the direct injection of chemotherapy agents into the vitreous cavity. Methotrexate and rituximab are widely used medications. Methotrexate, a folate antagonist, inhibits DNA synthesis in rapidly dividing cells, specifically targeting lymphoma cells in the vitreous. Rituximab, a monoclonal antibody that targets the CD20 antigen on B lymphocytes, aids in the elimination of malignant cells. These injections are given on a regular basis, usually weekly or biweekly, to achieve the best therapeutic concentrations within the eye.
Systemic Chemotherapy: Because VRL frequently causes CNS involvement, systemic chemotherapy is often required. The standard regimen is high-dose methotrexate, sometimes combined with other agents such as cytarabine and temozolomide. Systemic chemotherapy aids in the treatment of any undetected CNS disease and lowers the risk of systemic spread. Regular monitoring with imaging and lumbar punctures is required to assess treatment efficacy and adjust the regimen as necessary.
Radiation Therapy: Radiation therapy can be used as a standalone treatment or in combination with chemotherapy. External beam radiation therapy (EBRT) treats the entire eye or both eyes if bilateral involvement is suspected. EBRT is useful for controlling local disease and providing symptom relief. However, it raises the possibility of radiation-induced side effects such as cataract formation, dry eye syndrome, and radiation retinopathy.
Systemic Immunotherapy: Immunotherapy uses the body’s immune system to combat cancer. Immune checkpoint inhibitors such as pembrolizumab and nivolumab have shown promise in the treatment of VRL, especially in cases resistant to conventional chemotherapy. These drugs work by inhibiting immune cells’ inhibitory pathways, allowing the body to recognize and destroy cancer cells. Immunotherapy is frequently combined with other treatment modalities to achieve synergistic results.
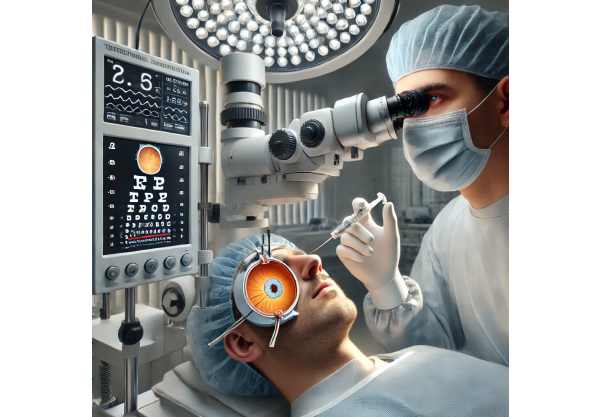
Surgical Interventions: In some cases, surgical procedures may be required to treat complications or obtain diagnostic samples. Vitrectomy, a surgical procedure that removes the vitreous gel, can be used to reduce tumor burden and improve visual clarity. Vitrectomy also enables direct examination and biopsy of the vitreous material, which aids in diagnosis and treatment planning.
Regular Monitoring and Follow-up Patients with VRL require continuous monitoring to assess treatment response, detect recurrences, and manage side effects. Regular eye exams, imaging studies, and laboratory tests are all necessary components of follow-up care. Multidisciplinary collaboration ensures comprehensive management and timely changes to the treatment plan.
Groundbreaking Therapies for Vitreoretinal Lymphoma
Recent advances in vitreoretinal lymphoma treatment are transforming the management of this complex condition. These innovations enhance diagnostic accuracy, treatment efficacy, and patient outcomes. Here are some of the most effective and innovative treatments currently transforming VRL care:
1. Targeted Therapy
Targeted therapies, which focus on specific molecular targets associated with VRL, represent a significant advancement in the treatment of this disease.
Bruton’s Tyrosine Kinase (BTK) inhibitors: BTK inhibitors, such as ibrutinib, have shown promise in treating VRL. BTK is an enzyme in the B-cell receptor signaling pathway that is required for the survival and proliferation of B-cell lymphomas. Ibrutinib inhibits BTK, which disrupts these pathways and causes cancer cell death. Clinical trials have shown that ibrutinib is effective in patients with relapsed or refractory VRL, offering a new treatment option for those who have not responded to conventional therapies.
Lenalidomide: Lenalidomide, an immunomodulatory drug, has been tested for anti-tumor activity in VRL. It works by improving immune function, preventing angiogenesis, and directly killing cancer cells. Studies have shown that lenalidomide, when combined with rituximab, can induce remission in VRL patients, providing a novel therapeutic approach.
2. Advanced Diagnostic Techniques.
Diagnostic technology advancements improve VRL detection and characterization, resulting in faster and more accurate diagnoses.
Next-Generation Sequencing (NGS): NGS enables comprehensive genetic profiling of VRL, revealing mutations and molecular changes that can help guide treatment decisions. By analyzing lymphoma cells’ genetic makeup, clinicians can tailor therapies to target specific mutations, improving treatment outcomes.
Liquid Biopsies: To detect VRL, liquid biopsies analyze circulating tumor DNA (ctDNA) in blood or vitreous fluid. This non-invasive method has several benefits, including early detection of relapse and real-time monitoring of treatment effectiveness. Liquid biopsies can provide valuable information about VRL’s genetic landscape, allowing for more personalized treatment strategies.
3. Novel Drug Delivery Systems.
Drug delivery innovations improve the administration and efficacy of VRL chemotherapeutic agents.
Nanoparticle-Based Delivery: Nanoparticles can encapsulate chemotherapeutic agents and deliver them directly to the vitreous and retina, thereby increasing drug penetration and retention. This technology enables the controlled and sustained release of drugs, potentially improving therapeutic outcomes and lowering systemic side effects.
Sustained-Release Implants: Intravitreal implants that release chemotherapy drugs over time are being developed to maintain therapeutic levels in the eye. These implants reduce the need for frequent injections while increasing patient compliance. There is ongoing research to optimize sustained-release formulations for VRL treatment.
4. Immunotherapy Advancements
Immunotherapy is constantly evolving, with new strategies emerging to harness the immune system against VRL.
CAR-T Cell Therapy: Chimeric antigen receptor (CAR) T-cell therapy involves modifying a patient’s T cells to express receptors that specifically target lymphoma cells. These engineered T cells are then reinfused into the patient, where they search for and destroy cancer cells. CAR T-cell therapy has demonstrated remarkable efficacy in treating other types of lymphoma and is being studied for VRL. Early research suggests that CAR T-cell therapy could be an effective and long-lasting treatment option for this difficult disease.
Checkpoint Inhibitors: Immune checkpoint inhibitors such as pembrolizumab and nivolumab are still being tested for their efficacy in VRL. By inhibiting immune cell inhibitory pathways, these drugs improve the body’s ability to mount an effective anti-tumor response. Combination therapies involving checkpoint inhibitors and other modalities are being investigated to maximize their potential.
5) Gene Therapy
Gene therapy is a cutting-edge treatment for VRL that targets the disease’s underlying genetic and molecular drivers.
CRISPR/Cas9 Gene Editing: CRISPR-Cas9 technology allows for precise genome editing to correct genetic mutations associated with VRL. This approach has the potential to provide long-term control or even cure by directly targeting the genetic abnormalities that cause lymphoma. Although research is still in its early stages, gene editing represents a promising new frontier in VRL therapy.
6. Integrated and Holistic Approaches
Integrative medicine combines conventional and alternative therapies to provide VRL patients with comprehensive care.
Nutritional Interventions: Consuming anti-inflammatory foods and antioxidants can improve overall health and reduce inflammation. Supplements like omega-3 fatty acids, vitamins C and E, and lutein may help manage VRL and improve treatment outcomes. Nutritional counseling is an essential component of comprehensive cancer care, as it addresses each patient’s unique needs.
Mind-Body Practices: Yoga, meditation, and Tai Chi can help manage stress and improve overall well-being, which may benefit VRL outcomes. These mind-body techniques can be combined with an integrative treatment plan to improve both mental and physical health.
Herbal and Complementary Therapies: Herbal remedies and complementary therapies, such as acupuncture and homeopathy, may have additional benefits for VRL management. While the scientific evidence for some of these therapies is still evolving, they can provide patients with supportive care and improve their quality of life.






