What is xanthelasma?
Xanthelasma is a condition in which yellowish, cholesterol-rich plaques form on the eyelids, most commonly around the inner canthus. These deposits are frequently soft and flat, posing a significant cosmetic concern for many patients. While xanthelasma is harmless and causes no pain or discomfort, it can occasionally be a sign of underlying lipid metabolism disorders, such as hyperlipidemia, and other cardiovascular risks.
Xanthelasma is more common in middle-aged and older adults, with a slightly higher incidence in women. The condition is typically associated with high cholesterol levels, but it can also affect people with normal lipid profiles. Xanthelasma is usually easy to diagnose based on its clinical appearance. However, a lipid profile test is frequently recommended to detect any associated lipid abnormalities that may need to be addressed.
Understanding the nature of xanthelasma, its potential systemic implications, and the significance of treating underlying lipid disorders is critical for effective management. Treatment focuses primarily on cosmetic plaque removal, but it also includes managing any associated lipid abnormalities to prevent recurrence and reduce cardiovascular risk.
Standard Treatments for Xanthelasma
The goal of xanthelasma management and treatment is to remove the plaques for cosmetic reasons while also managing any underlying lipid disorders that may be contributing to the condition. There are several standard treatment methods in use, each with its own set of advantages and disadvantages.
Topical Treatments: Topical treatments, such as trichloroacetic acid (TCA), chemically peel the affected area, reducing the appearance of xanthelasma. A healthcare professional must apply TCA carefully to avoid causing damage to the surrounding skin. This method is effective, but it may require several sessions and may cause irritation or temporary discoloration.
Cryotherapy is the use of extreme cold to destroy xanthelasma plaques. This treatment employs liquid nitrogen to freeze the affected tissue, which then falls off as it heals. Cryotherapy is a quick and minimally invasive procedure, but it may not be appropriate for all patients, particularly those with darker skin tones, because it can cause pigment changes.
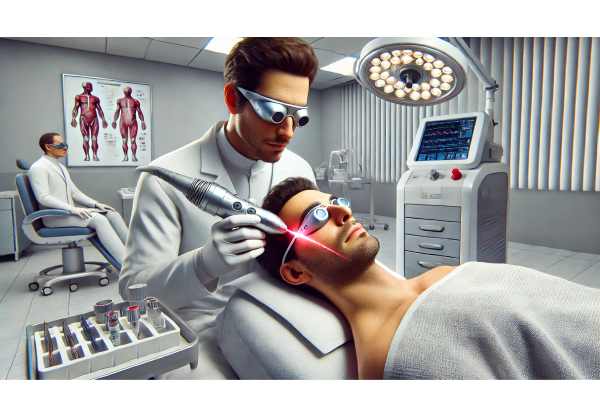
Laser Therapy: Laser therapy is a popular method for removing xanthelasma, which uses lasers like CO2 or Erbium:YAG to precisely target and vaporize the plaques. This technique provides high precision, minimal bleeding, and a reduced risk of scarring. However, it is more expensive than other methods due to the need for specialized equipment and trained personnel.
Surgical Excision: For larger or more stubborn plaques, surgical removal may be required. This involves physically removing the xanthelasma and suturing the skin. Surgical excision, while effective, is associated with a higher risk of scarring and infection than other treatments. It is typically reserved for situations in which other methods have failed or are ineffective.
Electrodesiccation: Electrodesiccation is the destruction of xanthelasma tissue using electrical current. This method is useful for small plaques and is frequently combined with curettage (scraping off the tissue). To reduce the risk of scarring and pigmentation changes, electrodesiccation must be performed by a skilled professional, as with all other methods.
Lipid-Lowering Therapy: Because xanthelasma is frequently associated with lipid metabolism disorders, treating the underlying conditions is critical. Statins, fibrates, and niacin are examples of lipid-lowering medications that can help lower cholesterol and potentially prevent xanthelasma recurrences. To manage lipid levels and overall cardiovascular health, dietary and lifestyle changes such as a low-fat diet, regular exercise, and quitting smoking are recommended.
Breakthrough Innovations in Xanthelasma Treatment
Recent advances in xanthelasma treatment have significantly improved the condition’s management, providing more effective and less invasive options. These advancements are altering the approach to treating xanthelasma and improving patient outcomes. Here are some of the most effective and innovative treatments currently available:
1. Advanced Laser Technology
Laser therapy is evolving, providing more precise and effective treatments for xanthelasma with less downtime and a lower risk of complications.
Fractional CO2 Lasers: Fractional CO2 lasers are a targeted approach to xanthelasma removal, delivering laser energy in a grid pattern while leaving surrounding tissue intact. This method promotes faster healing while lowering the risk of scarring and pigmentation changes. Fractional CO2 lasers effectively remove xanthelasma plaques while causing minimal damage to the surrounding skin.
Pulsed Dye Lasers: Pulsed dye lasers (PDL) aim at the blood vessels within xanthelasma plaques, causing them to collapse and be reabsorbed by the body. PDL is less invasive than traditional laser therapies and carries a lower risk of post-treatment hyperpigmentation. This method is especially useful for patients who have sensitive skin or are prone to pigmentation issues.
2. Minimal Invasive Procedures
Minimally invasive procedures are gaining popularity due to their ability to effectively treat xanthelasma while posing fewer risks and requiring shorter recovery times.
Radiofrequency Ablation: Radiofrequency ablation (RFA) is the process of heating and destroying xanthelasma plaques using radiofrequency energy. This method is extremely precise, allowing for controlled tissue removal with little impact on the surrounding area. RFA has a short recovery period and minimal discomfort, making it an appealing option for patients looking for effective treatment with little downtime.
Microdermabrasion with Chemical Peels: Combining microdermabrasion and chemical peels improves the efficacy of topical treatments. Microdermabrasion exfoliates the skin gently, allowing chemical agents such as TCA to penetrate more deeply. This combination approach can help remove xanthelasma plaques and promote smoother, more even skin texture.
3. Novel Pharmacological Approaches
New pharmacologic treatments are opening up new options for managing xanthelasma, particularly in terms of lowering the risk of recurrence and treating underlying lipid disorders.
Topical Statins: Researchers are investigating the use of topical statins, such as atorvastatin and simvastatin, to reduce cholesterol deposits in the skin. These topical formulations aim to provide localized treatment while minimizing systemic absorption, lowering the risk of side effects associated with oral statins. Early research indicates that topical statins can effectively reduce xanthelasma plaques and prevent recurrence.
Anti-inflammatory Agents: Inflammation plays a role in the development of xanthelasma, and anti-inflammatory drugs are being studied for their ability to reduce plaque formation. Topical formulations containing anti-inflammatory compounds, such as corticosteroids or nonsteroidal anti-inflammatory drugs (NSAIDs), may help manage xanthelasma by addressing the underlying inflammatory processes.
- Integrative and Holistic Approaches.
Integrative medicine combines conventional and alternative therapies to provide comprehensive care for xanthelasma patients.
Nutritional Interventions: A diet high in nutrients that promote lipid metabolism and skin health can help manage xanthelasma. Foods high in omega-3 fatty acids, antioxidants, and fiber can help lower cholesterol and improve skin quality. Nutritional counseling can assist patients in developing dietary habits that promote overall health and reduce the likelihood of xanthelasma recurrence.
Mind-Body Practices: Yoga, meditation, and mindfulness can help manage stress, which can lead to lipid metabolism disorders and xanthelasma formation. These mind-body techniques can be combined with an integrative treatment plan to improve both mental and physical health.
Herbal and Complementary Therapies: Acupuncture and homeopathy, for example, may offer additional benefits in the treatment of xanthelasma. While the scientific evidence for some of these therapies is still evolving, they can provide patients with supportive care and improve their quality of life.
5) Genetic and Molecular Research
Advances in genetic and molecular research are shedding light on xanthelasma’s underlying mechanisms, paving the way for targeted therapies.
Genetic Screening: Genetic testing can help identify people who are at risk for developing xanthelasma due to inherited lipid metabolism disorders. Early detection enables proactive management and lifestyle changes to reduce the risk of xanthelasma development and associated cardiovascular diseases.
Molecular Targeting: Studies on the molecular pathways involved in cholesterol metabolism and plaque formation are leading to the development of targeted therapies. These therapies aim to specifically inhibit the processes that cause xanthelasma, resulting in more effective and precise treatment options.
6. AI & Machine Learning
AI and machine learning are revolutionizing xanthelasma diagnosis and management by providing cutting-edge analytical tools and predictive models.
AI-Powered Diagnostics: AI algorithms can use clinical images to detect and quantify xanthelasma plaques with great accuracy. These tools improve diagnostic accuracy and allow for more personalized treatment plans. AI-powered diagnostics can also track treatment progression and predict the likelihood of recurrence.
Predictive Analytics: Machine learning models can forecast patient responses to various treatments based on a variety of clinical and genetic data. This information enables clinicians to choose the most effective therapies and adjust treatment plans as needed. Predictive analytics can also detect potential side effects and complications, which improves patient safety and treatment.