Infectious endophthalmitis is a severe, sight-threatening emergency characterized by inflammation of the internal structures of the eye due to microbial infection. Rapid diagnosis and decisive intervention are critical, as delays may lead to irreversible vision loss or even loss of the eye itself. This complex condition can arise after eye surgery, trauma, or systemic infection, and affects individuals of all ages. In this detailed treatment and management guide, we explore proven conventional therapies, surgical interventions, and emerging innovations that are redefining patient outcomes—equipping you with the latest, most practical knowledge for prevention, early detection, and successful recovery.
Table of Contents
- Comprehensive Overview, Epidemiology, and Pathogenesis
- Current Conventional and Pharmacological Treatment Approaches
- Operative Techniques and Interventional Procedures
- Recent Advances and Emerging Technologies in Management
- Clinical Trials and Future Directions for Infectious Endophthalmitis
- Frequently Asked Questions
- Disclaimer
Comprehensive Overview, Epidemiology, and Pathogenesis
Infectious endophthalmitis is a medical emergency defined by infection of the vitreous and/or aqueous humor. This intraocular inflammation can destroy vision within hours if not swiftly treated.
Definition and Classification
- Exogenous Endophthalmitis: Most cases occur due to external entry of pathogens following ocular surgery (especially cataract surgery), intravitreal injections, or trauma.
- Endogenous Endophthalmitis: Less common, results from hematogenous spread of infection from a distant site (often associated with immunocompromised patients, intravenous drug use, or sepsis).
Pathophysiology
- Infectious agents, primarily bacteria (gram-positive Staphylococcus and Streptococcus, gram-negative organisms, less commonly fungi), penetrate the ocular barriers.
- The immune response triggers intense inflammation, cellular infiltration, and cytokine release.
- Rapid destruction of ocular tissues can occur, leading to vision loss.
Prevalence and Risk Factors
- Incidence after cataract surgery: 0.03%–0.2%
- Post-injection endophthalmitis: ~0.02%–0.05% per injection
- Higher risk in eyes with diabetes, immunosuppression, complicated surgeries, wound leaks, or contaminated surgical fields.
- Traumatic cases occur after open globe injuries with retained foreign bodies or delayed repair.
Clinical Presentation
- Sudden onset pain, redness, and profound loss of vision
- Photophobia, eyelid swelling, hypopyon (layered pus in anterior chamber)
- Vitreous haze and loss of red reflex on ophthalmoscopy
Complications if Untreated
- Panophthalmitis (infection spreading to orbital tissues)
- Retinal detachment
- Phthisis bulbi (shrunken, nonfunctional eye)
Practical Advice:
If you have recently undergone eye surgery or suffered trauma and develop sudden pain, redness, or vision changes, seek urgent care from an ophthalmologist. Early diagnosis and rapid intervention can make the difference between saving vision and permanent blindness.
Current Conventional and Pharmacological Treatment Approaches
The management of infectious endophthalmitis must be prompt and aggressive, tailored to the cause, severity, and patient-specific factors.
Immediate Diagnostic Steps
- Ocular Examination: Slit-lamp and indirect ophthalmoscopy to assess anterior and posterior segments.
- Microbiological Sampling: Aqueous and vitreous taps (small fluid samples) sent for Gram stain, culture, and sometimes PCR to guide therapy.
- Imaging: B-scan ultrasonography if media opacity precludes visualization.
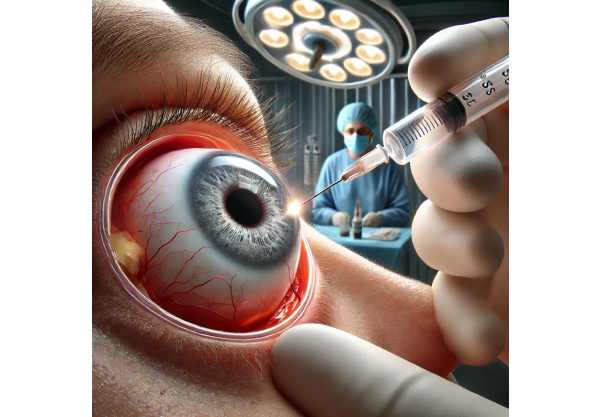
Empirical Intravitreal Antibiotics
- Empirical therapy is initiated before culture results due to the emergency nature.
- Vancomycin (gram-positive coverage) + Ceftazidime or Amikacin (gram-negative coverage) are injected directly into the vitreous cavity.
- Voriconazole or Amphotericin B may be added if fungal infection is suspected (e.g., immunosuppressed or trauma with organic material).
Systemic and Topical Medications
- Systemic antibiotics may be given in severe exogenous cases or all endogenous cases (e.g., IV vancomycin, ceftazidime).
- Topical antibiotics and corticosteroids reduce anterior segment inflammation and secondary infection risk.
- Cycloplegics (e.g., atropine drops) provide pain relief and prevent synechiae (adhesions).
Steroid Use
- Corticosteroids (topical, periocular, or intravitreal) are controversial. They help reduce inflammation but may suppress immune clearance; use is tailored to organism, severity, and immune status.
Monitoring and Follow-Up
- Frequent exams (daily or every few hours in acute cases)
- Repeat intravitreal injections based on clinical response and organism sensitivities
Special Considerations for Fungal Endophthalmitis
- Fungi (especially Candida, Aspergillus) require systemic antifungals (oral or IV voriconazole, amphotericin B), plus repeated intravitreal antifungal injections.
- Prognosis is generally worse than bacterial cases, and longer therapy is needed.
Home Care and Patient Education
- Strict adherence to drop and medication regimens
- Monitoring for worsening symptoms (increased pain, vision loss, new floaters)
- Infection prevention: avoid eye rubbing, maintain hygiene, and report any new symptoms after eye procedures
Patient Tip:
Keep an updated list of all eye medications and dosages, and don’t hesitate to reach out to your care team with any concerns about side effects or missed doses. Recovery often requires patience and strict medical follow-up.
Operative Techniques and Interventional Procedures
Surgical intervention is a mainstay in severe, sight-threatening endophthalmitis or when response to initial medical therapy is insufficient.
Pars Plana Vitrectomy (PPV)
- What It Is: Surgical removal of infected vitreous gel using specialized instruments through tiny incisions in the sclera (white of the eye).
- Why It’s Done: Clears infection, removes inflammatory debris, improves access for antibiotics, and helps prevent retinal detachment.
- Modern Advances: Microincision vitrectomy (MIVS) enables safer, faster recovery with less trauma to surrounding tissues.
Timing and Indications
- Acute, severe vision loss (e.g., light perception only) calls for immediate PPV.
- Milder cases may be managed with repeated taps and injections, but PPV is increasingly considered earlier based on evolving evidence.
Intraoperative Procedures
- Removal of Foreign Bodies: Especially in post-traumatic cases to reduce microbial load.
- Silicone Oil or Gas Tamponade: Used in select cases to stabilize the retina and promote healing.
- Retinal Repair: If concurrent detachment or tears are detected.
Adjunctive Intraocular Drug Delivery
- Intraoperative intravitreal antibiotics, antifungals, or antivirals may be given during vitrectomy.
- Sustained-release implants (e.g., dexamethasone) are being studied to provide ongoing anti-inflammatory effects post-surgery.
Other Procedures
- Anterior Chamber Washout: For heavy hypopyon or fibrin, to reduce inflammatory burden and improve visualization.
- Enucleation (Eye Removal): Reserved for severe, unresponsive panophthalmitis to prevent life-threatening spread.
Postoperative Care and Monitoring
- Intensive topical, systemic, and sometimes repeat intravitreal therapy.
- Monitoring for complications: elevated intraocular pressure, retinal detachment, or recurrent infection.
Practical Guidance:
If you are scheduled for eye surgery or trauma repair, ask your surgeon about infection prevention strategies and postoperative warning signs. Prompt recognition and treatment of complications is vital for vision preservation.
Recent Advances and Emerging Technologies in Management
Innovations in diagnostics, therapeutics, and care delivery are changing the landscape of endophthalmitis management.
Rapid Diagnostics
- PCR-Based Pathogen Detection: Polymerase chain reaction can identify organisms within hours, even if cultures are negative—speeding targeted therapy.
- Next-Generation Sequencing (NGS): Simultaneously detects multiple pathogens and antibiotic resistance genes, informing tailored regimens.
- Point-of-Care Testing: New handheld devices are in development for bedside or remote diagnosis.
Sustained-Release Drug Delivery
- Intraocular Implants: Ongoing trials explore antibiotic or antifungal implants that release drugs over days to weeks, minimizing repeat injections.
- Drug-Eluting Sutures and Hydrogels: Provide localized delivery at surgical sites, reducing recurrence risk.
Minimally Invasive Surgical Platforms
- 25- and 27-Gauge Vitrectomy Systems: Allow safer, faster surgery with less post-op discomfort and quicker return to vision.
- Robotic-Assisted Vitrectomy: Early-stage research for greater precision, especially in complex or pediatric cases.
Biological and Immunomodulatory Strategies
- Monoclonal Antibodies: New drugs that neutralize bacterial toxins or modulate the immune response.
- Gene Therapy: Experimental approaches to enhance local immune defenses and reduce infection risk.
Artificial Intelligence in Imaging and Monitoring
- AI-powered tools for automated detection of subtle signs on OCT or B-scan imaging, alerting clinicians to early relapse or complications.
- Teleophthalmology: Remote assessment, digital triage, and telemonitoring for follow-up, especially in rural or underserved areas.
Best Practices for Patients and Providers
- Adoption of “bundled” prevention protocols in operating rooms (antisepsis, perioperative antibiotics, wound closure checks).
- Real-time feedback systems for early symptom reporting via mobile health apps.
Practical Advice:
Stay informed about new options and ask your provider whether you might benefit from advanced diagnostic or therapeutic techniques. Participation in clinical trials may offer access to cutting-edge care.
Clinical Trials and Future Directions for Infectious Endophthalmitis
The landscape of endophthalmitis care is shaped by ongoing research and a robust clinical trial pipeline.
Major Areas of Research
- Optimizing Drug Delivery: Studies on sustained-release antibiotics, antifungals, and anti-inflammatory agents for long-term intraocular effect with fewer interventions.
- Next-Generation Surgical Techniques: Evaluating microincision and robotic-assisted vitrectomy for speed, safety, and visual recovery.
- Molecular and Genetic Diagnostics: Integrating NGS and PCR into routine workflows to guide therapy more rapidly and accurately.
- Host Immune Response Modulation: Understanding genetic and immunological factors influencing susceptibility and recovery, paving the way for precision medicine.
- Biofilm and Resistance Research: New approaches to combat biofilm-producing bacteria and multidrug-resistant organisms.
Ongoing and Recent Clinical Trials
- Intravitreal moxifloxacin for multidrug-resistant endophthalmitis
- Drug-eluting intraocular devices for postoperative prophylaxis
- Real-world outcomes comparing early versus delayed vitrectomy
Future Directions
- Personalized Medicine: Use of patient-specific risk factors and microbiological profiles to guide therapy.
- Remote Monitoring: Integration of wearable or smartphone-based tools for early detection of relapse.
- Collaborative Care Models: Multidisciplinary teams—including infectious disease, surgery, and vision rehab—optimizing outcomes for high-risk or recurrent cases.
How to Find and Join Trials
- Ask your ophthalmologist about local or national registries.
- Visit official clinical trial websites or academic hospital platforms.
Empowering Patients and Families
- Stay proactive: Early detection and reporting symptoms is key.
- Engage in support groups and educational forums for updates on advances.
Frequently Asked Questions
What is infectious endophthalmitis and what causes it?
Infectious endophthalmitis is an inflammation inside the eye caused by bacteria or fungi. It often follows eye surgery, injections, trauma, or spreads from infection elsewhere in the body.
What are the symptoms of infectious endophthalmitis?
Symptoms include sudden eye pain, redness, blurry or decreased vision, light sensitivity, and sometimes pus inside the eye (hypopyon). These symptoms require emergency eye care.
How is infectious endophthalmitis diagnosed?
Diagnosis involves an eye examination, sampling of eye fluids for culture or PCR, and often ultrasound imaging to assess the extent of infection.
What are the main treatments for infectious endophthalmitis?
Treatment includes intravitreal antibiotics or antifungals, possible systemic medications, and often urgent surgery (vitrectomy) to clear infection and preserve vision.
Can vision be saved after infectious endophthalmitis?
Vision outcomes vary—rapid diagnosis and treatment increase the chances of recovery. Some patients regain functional vision, while others may experience permanent loss if care is delayed.
How can infectious endophthalmitis be prevented?
Prevention involves sterile surgical techniques, antibiotic prophylaxis, and prompt treatment of eye injuries. Patients should monitor for symptoms after any eye procedure or trauma.
Are there new treatments for infectious endophthalmitis?
Yes, research is advancing rapid diagnostics, sustained-release drugs, and minimally invasive surgery. Participation in clinical trials may provide access to these innovations.
Disclaimer
This content is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult an eye care professional with questions regarding your condition.
If you found this article helpful, please share it on Facebook, X (formerly Twitter), or your preferred social platforms. Your support enables us to continue producing reliable, in-depth health content for readers like you—thank you!










