What is Diabetic Papillopathy?
Diabetic papillopathy is a rare but significant ocular complication of diabetes mellitus. It primarily affects the optic disc, resulting in swelling and visual disturbances. Diabetic papillopathy, while often self-limiting, can be an early warning sign of diabetes-related systemic microvascular complications. The condition is most commonly seen in young people with Type 1 diabetes, but it can also affect those with Type 2 diabetes. Understanding the underlying mechanisms, clinical presentation, and potential consequences of diabetic papillopathy is critical for early detection and treatment, which can help prevent additional ocular and systemic complications.
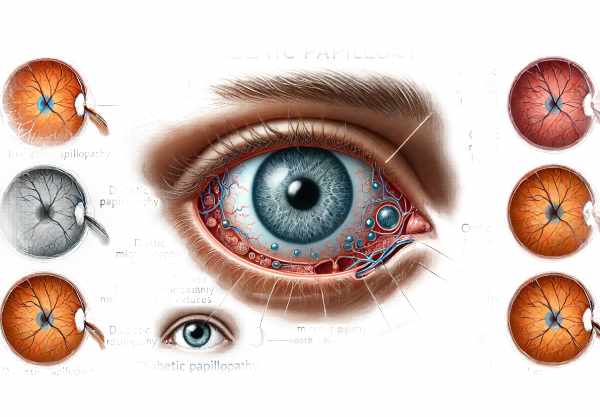
Diabetic Papillopathy Comprehensive Insights
Diabetic papillopathy is a distinct form of diabetic microangiopathy that only affects the optic nerve head. Unlike other more common diabetic ocular complications, such as diabetic retinopathy, diabetic papillopathy is poorly understood and frequently misdiagnosed due to its subtle and variable presentation.
Pathophysiology
Diabetic papillopathy develops as a result of a complex interaction of metabolic, vascular, and possibly inflammatory factors. Chronic hyperglycemia causes endothelial dysfunction, which impairs the microvascular supply to the optic nerve head. The resulting ischemia and disruption of the blood-retinal barrier cause optic disc edema. Furthermore, the role of diabetic neuropathy and its effect on optic nerve fibers must be considered. These factors all contribute to the development of diabetic papillopathy.
Clinical Presentation
Diabetic papillopathy can present with a variety of symptoms, making diagnosis difficult. Patients may report blurred vision, visual field defects, or even a mild reduction in visual acuity. However, a large number of cases are asymptomatic, with the condition discovered during routine ophthalmic examinations.
Diabetic papillopathy usually causes bilateral optic disc swelling, but it can also be unilateral. This swelling is usually mild to moderate, and unlike papilledema, it does not cause significant vision loss. A fundoscopic examination reveals hyperemic optic discs with blurred margins, as well as flame-shaped hemorrhages or cotton wool spots on or near the disc.
Risk Factors
Several risk factors for diabetic papillopathy exist, which are similar to those for other diabetic microvascular complications. The main risk factor is chronic and poorly controlled hyperglycemia, which worsens endothelial dysfunction and microvascular damage. Another common comorbidity in diabetic patients is hypertension, which causes vascular stress and contributes to optic nerve head ischemia.
Additionally, the duration of diabetes is an important consideration. Patients with a longer diabetes history are more likely to develop microvascular damage over time. Other systemic factors, such as dyslipidemia, smoking, and obesity, increase the risk by adding to the overall vascular burden.
Differential Diagnosis
The differential diagnosis of diabetic papillopathy includes a number of conditions characterized by optic disc edema. These include papilledema caused by elevated intracranial pressure, non-arteritic anterior ischemic optic neuropathy (NAION), and hypertensive retinopathy. Differentiating between these conditions is critical for effective management.
Papilledema is characterized by bilateral optic disc swelling caused by increased intracranial pressure, and it is frequently accompanied by symptoms like headache, nausea, and vomiting. Diabetic papillopathy, on the other hand, is rarely accompanied by these systemic symptoms.
NAION causes sudden, painless vision loss and is characterized by a pale, swollen optic disc rather than the hyperemic appearance seen in diabetic papillopathy. It primarily affects older people and is linked to systemic vascular risk factors.
Hypertensive retinopathy can cause optic disc edema, but it is usually accompanied by other retinal signs such as arteriolar narrowing, flame hemorrhages, and cotton wool spots, which reflect the long-term effects of high blood pressure on the retinal vasculature.
Impact on Vision
Diabetic papillopathy has a milder impact on vision than other optic neuropathies. Most patients experience only a slight decrease in visual acuity or minor visual field defects. However, significant visual impairment can occur in rare cases, especially if there is concurrent diabetic macular edema or other retinal pathology.
The swelling of the optic disc usually goes away on its own after a few weeks or months, and the visual symptoms improve as well. Despite the generally favorable prognosis, these patients must be closely monitored due to the risk of recurring episodes and the possibility of progressive diabetic retinopathy.
Long-Term Complications
While diabetic papillopathy frequently resolves without causing long-term complications, it is critical to recognize it as a sign of systemic microvascular disease. Diabetic papillopathy increases the risk of other diabetic complications such as nephropathy, neuropathy, and severe forms of diabetic retinopathy.
As a result, the discovery of diabetic papillopathy should prompt a thorough review of the patient’s overall diabetic control and management of associated comorbidities. Improved glycemic control, blood pressure management, and lipid optimization are critical strategies for lowering overall vascular risk.
Diabetic Papillopathy Prevention Strategies
- Maintain Optimal Glycemic Control: Maintaining blood glucose levels in the target range is critical for lowering the risk of diabetic papillopathy and other microvascular complications.
- Regular Eye Examinations: Have a comprehensive eye exam at least once a year to detect diabetic papillopathy and other ocular complications.
- Control Blood Pressure: Managing hypertension with lifestyle changes and medications reduces vascular stress and protects the optic nerve head.
- Healthy Diet: Eat a well-balanced diet rich in fruits, vegetables, whole grains, and lean proteins to improve overall vascular health and lower oxidative stress.
- Quit Smoking: Smoking cessation is critical for reducing oxidative stress and vascular damage, lowering the risk of diabetic complications.
- Manage Lipid Levels: To reduce vascular risk, regularly monitor and control cholesterol and triglyceride levels with diet, exercise, and medications.
- Stay Physically Active: Regular physical activity can help improve insulin sensitivity, lower blood pressure, and improve overall cardiovascular health.
- Monitor Weight: Maintaining a healthy weight lowers the risk of insulin resistance and related metabolic issues.
- Educate Yourself: Stay informed about diabetes management and potential complications so you can take proactive steps to maintain your health.
- Follow Medical Advice: Follow your healthcare provider’s diabetes management recommendations, which include medication adherence and lifestyle changes.
Diagnostic Tools for Diabetic Papillopathy
Diabetic papillopathy is diagnosed after a thorough clinical evaluation and the use of advanced imaging techniques to distinguish it from other causes of optic disc swelling. An ophthalmologist or optometrist usually performs a comprehensive eye examination to begin the diagnostic process.
The Visual Acuity Test:
A visual acuity test determines the clarity of vision. Patients with diabetic papillopathy may have slightly reduced visual acuity, but significant vision loss is rare.
Fundoscopy:
Fundoscopy, also known as ophthalmoscopy, is required for direct visualization of the optic disc. Diabetic papillopathy causes the optic disc to appear swollen and hyperemic, with blurred margins. Flame-shaped hemorrhages and cotton wool spots may also be seen around the disc.
Optical Coherence Tomography(OCT):
OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina and optic nerve head. It aids in determining the severity of optic disc edema and detecting any associated macular edema. OCT is especially useful for tracking changes over time and evaluating treatment outcomes.
fluorescein angiography (FA):
FA involves injecting a fluorescent dye into the bloodstream and taking sequential images of the retinal vasculature. It aids in assessing retinal circulation and detecting leakage from microaneurysms or neovascularization. FA can confirm the diagnosis of diabetic papillopathy by revealing optic disc leakage.
Visual Field Test:
Visual field testing assesses both central and peripheral vision. Patients with diabetic papillopathy may have visual field defects, but these are usually minor. This test is useful for establishing a baseline visual function and tracking changes over time.
Color Vision Test:
Color vision testing can help detect subtle changes in color perception that may be present in diabetic papillopathy. This is frequently done using pseudoisochromatic plates or other standardized color vision tests.
Magnetic Resonance Imaging(MRI):
When the diagnosis is uncertain or there is a possibility of other neurological conditions, an MRI of the brain and orbits may be performed. MRI can help rule out other causes of optic disc swelling, including optic neuritis, compressive optic neuropathy, and intracranial masses.
Optical Coherence Tomography Angiogram (OCTA):
OCTA is a sophisticated imaging technique that produces detailed images of the retinal and optic nerve head vasculature without the need for dye injection. It allows for the evaluation of microvascular changes and blood flow in the optic nerve head, providing valuable information about the vascular component of diabetic papillopathy.
** Electroretinography (ERG)**:
ERG measures the retina’s electrical responses to light stimulation. While not commonly used in the diagnosis of diabetic papillopathy, it can provide additional information about retinal function and help rule out other retinal disorders.
Combining these diagnostic methods ensures a thorough evaluation of diabetic papillopathy, allowing for accurate diagnosis and differentiation from other optic neuropathies. Early and accurate diagnosis is critical for determining appropriate treatment and tracking the condition’s progression.
Standard Treatments for Diabetic Papillopathy
Diabetic papillopathy is treated primarily by managing the underlying diabetes and any associated ocular or systemic conditions. The condition is frequently self-limiting, but certain treatments can help relieve symptoms and prevent complications.
Glycemic control:
Maintaining optimal blood glucose levels is critical for treating diabetic papillopathy. Tight glycemic control lowers the risk of additional microvascular damage and promotes the resolution of optic disc edema. Patients are advised to follow their diabetes management plan, which includes regular blood glucose monitoring, medication adherence, and lifestyle changes.
blood pressure management:
Controlling hypertension is critical for lowering vascular stress and protecting the optic nerve head. Patients with diabetic papillopathy are encouraged to regularly monitor their blood pressure and take antihypertensive medications as directed by their healthcare provider.
Observation:
Diabetic papillopathy often resolves spontaneously over a few weeks or months. Regular follow-up visits with an ophthalmologist are required to monitor the condition and ensure that it improves. During these visits, visual acuity, optic disc appearance, and OCT measurements are taken to monitor progress.
Steroid Therapy*:
Corticosteroids may be used if the optic disc edema is severe and causes significant visual impairment. Steroids help to reduce inflammation and edema, but their use must be balanced against potential side effects, particularly in diabetic patients. Depending on the severity of the condition, either intravitreal steroid injections or oral corticosteroids may be used.
Anti-VEGF Treatment:
Anti-vascular endothelial growth factor (anti-VEGF) therapy is widely used in the treatment of diabetic macular edema and proliferative diabetic retinopathy. While anti-VEGF injections are not a standard treatment for diabetic papillopathy, they may be considered if visual symptoms are exacerbated by concurrent macular edema or neovascularization.
Neuroprotective Agents*:
Emerging research is looking into the use of neuroprotective agents to preserve optic nerve function and prevent further damage. These agents are intended to protect retinal ganglion cells and optic nerve fibers from oxidative stress and ischemia. Although neuroprotective therapies are still experimental, they show promise for the future management of diabetic papillopathy.
Laser therapy:
Laser photocoagulation is an established treatment for diabetic retinopathy. If diabetic papillopathy coexists with proliferative diabetic retinopathy, focal or pan-retinal laser photocoagulation may be used to reduce the risk of vision-threatening complications.
Lifestyle Modifications:
Patients are encouraged to lead a healthy lifestyle to improve their overall vascular health. This includes consuming an antioxidant-rich diet, engaging in regular physical activity, quitting smoking, and managing weight. These lifestyle changes improve insulin sensitivity, lower oxidative stress, and promote vascular function.
Patient education and support:
It is critical to educate patients about diabetic papillopathy and how it affects systemic diabetes management. Providing support and resources for effective diabetes management, such as access to diabetes educators and support groups, can help patients adhere to treatment plans and achieve better outcomes.
The goal of diabetic papillopathy management is to preserve vision, prevent complications, and improve patients’ overall quality of life by combining standard and emerging treatment approaches.
Trusted Resources
Books
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski
- “Diabetes and Ocular Disease: Past, Present, and Future Therapies” by Ingrid U. Scott
- “Optic Nerve Disorders: Diagnosis and Management” by Jane W. Chan










