Distichiasis is a complex eyelid condition in which an extra row of eyelashes grows from the meibomian gland openings, sometimes causing significant discomfort and corneal complications. Whether inherited or acquired, distichiasis can present as mild irritation or progress to persistent pain, tearing, and even vision loss. Early recognition and timely management are crucial to prevent long-term damage. In this comprehensive guide, you’ll discover a full spectrum of current and emerging approaches—from home care and medical therapies to the latest surgical solutions and groundbreaking innovations—ensuring you’re informed and empowered at every step of the journey.
Table of Contents
- Distichiasis Fundamentals and Prevalence Patterns
- Nonsurgical Care and Medication Strategies
- Operative Approaches and Procedural Interventions
- Advancements in Technology and Innovative Treatments
- Clinical Trials and Anticipated Advancements
- Frequently Asked Questions
Distichiasis Fundamentals and Prevalence Patterns
Defining Distichiasis:
Distichiasis is characterized by the presence of a supplementary row of eyelashes originating abnormally from the meibomian gland orifices along the eyelid margin. Unlike normal eyelashes, these aberrant lashes may grow in directions that irritate the eye surface, leading to a variety of symptoms.
Pathophysiology and Types:
- Congenital distichiasis: Often inherited as an autosomal dominant trait, frequently associated with lymphedema-distichiasis syndrome. Lashes are typically soft and less likely to cause injury in childhood, but may stiffen with age.
- Acquired distichiasis: Usually develops after chronic inflammation, trauma, or following certain eye surgeries. The lashes can be more coarse and symptomatic.
Prevalence and Demographics:
- Congenital forms are rare and may be underdiagnosed, often detected in childhood or adolescence.
- Acquired forms are more common in adults with chronic blepharitis, ocular cicatricial pemphigoid, Stevens-Johnson syndrome, or those with repeated eyelid trauma.
Risk Factors:
- Family history of distichiasis or related syndromes
- Chronic eyelid inflammation
- Repeated eyelid procedures or injuries
- Certain autoimmune disorders
Symptoms and Clinical Signs:
- Foreign body sensation and irritation
- Red, watery eyes (epiphora)
- Light sensitivity and frequent blinking
- Chronic conjunctivitis or recurrent corneal abrasions
- Vision disturbances if corneal scarring develops
Diagnosis:
- Slit-lamp examination: Reveals abnormal lash row at meibomian gland orifices
- Eyelid eversion: Helps visualize and assess aberrant lashes
- Corneal and conjunctival assessment: Checks for surface damage
Practical Advice:
If you experience persistent eye irritation or notice abnormal lash growth, consult an ophthalmologist early—prompt action can prevent corneal complications and improve comfort.
Nonsurgical Care and Medication Strategies
Conservative Symptom Relief:
- Lubricating eye drops/ointments: Help shield the cornea from friction and reduce irritation.
- Artificial tears: Useful for mild cases, especially when lash contact with the cornea is minimal.
- Cool compresses: Provide short-term relief from inflammation and discomfort.
- Antibiotic or steroid ointments: Can reduce secondary infection risk and decrease swelling from chronic irritation.
Mechanical Management:
- Epilation (lash plucking):
- Temporarily removes aberrant lashes using forceps.
- Simple and quick, but lashes usually regrow in 2–6 weeks.
- Can be done at home with proper training, but professional care reduces risk of infection and incomplete removal.
- Bandage Contact Lenses:
- Protect the cornea in severe cases or while awaiting surgery.
- Best used short-term, as long-term wear increases risk of infection.
Pharmacologic Options:
- Topical anti-inflammatories: May be prescribed for patients with chronic blepharitis or coexisting inflammation.
- Immunomodulatory agents: In select cases with autoimmune components (e.g., ocular cicatricial pemphigoid), systemic therapies may be needed under specialist care.
Patient Education and Self-Care Tips:
- Practice excellent eyelid hygiene—use gentle lid scrubs and avoid harsh chemicals.
- If lashes are frequently irritating, avoid rubbing your eyes, which can worsen symptoms.
- Consider keeping a “lash diary” to monitor symptoms, triggers, and effectiveness of different management strategies.
Long-tail Keywords Used:
- distichiasis home treatment
- non-surgical eyelash removal
- artificial tears for eyelid irritation
- bandage contact lens for corneal protection
Operative Approaches and Procedural Interventions
Indications for Surgical Management:
When symptoms are severe, persistent, or when there is a risk of vision loss due to corneal damage, surgical or minimally invasive interventions become necessary.
Key Surgical and Office-Based Techniques:
- Electrolysis:
- Uses a fine needle with electrical current to destroy the hair follicle.
- Effective for isolated lashes; several sessions may be needed for complete eradication.
- May cause minor discomfort or swelling post-procedure.
- Cryotherapy (Cryoepilation):
- Freezes and destroys aberrant follicles using controlled cold.
- Often used for larger lash groups; risk of skin depigmentation or lid notching.
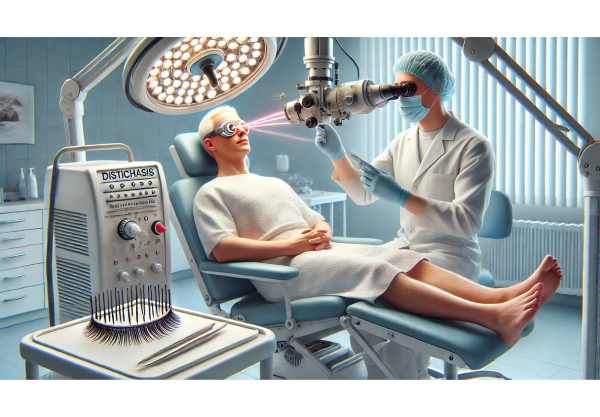
- Laser Ablation:
- Argon or diode lasers target lash follicles, offering precise and often permanent removal.
- Best suited for focal, stubborn lashes.
- Surgical Resection:
- Involves excising a portion of the eyelid margin containing abnormal follicles.
- Reserved for extensive or recurrent cases.
- More invasive, requires anesthesia, and carries risk of scarring or eyelid malposition.
- Radiofrequency Ablation:
- Delivers high-frequency electrical energy to ablate follicles.
- Growing in popularity due to precision and lower recurrence rates.
Post-Procedure Care:
- Use cold compresses to reduce swelling.
- Apply antibiotic ointment as prescribed.
- Avoid touching or rubbing the treated area.
- Follow up closely with your eye care provider to monitor for recurrence or complications.
Practical Advice:
Discuss all available procedural options, including their risks, benefits, and recovery times, with your ophthalmologist to select the approach best suited to your lifestyle and preferences.
Long-tail Keywords Used:
- permanent eyelash removal for distichiasis
- cryotherapy for abnormal eyelash growth
- radiofrequency ablation eyelid
- laser distichiasis surgery outcomes
Advancements in Technology and Innovative Treatments
Modern Innovations Transforming Care:
- High-Precision Imaging:
- Newer slit-lamp cameras and imaging software allow detailed mapping of lash origins and corneal health.
- Supports personalized surgical planning and better outcome tracking.
- Robotic and AI-Guided Surgery:
- Early-phase trials of robotic micro-surgical tools for ultra-precise lash ablation.
- AI helps analyze recurrence patterns and optimize procedural strategies for individual patients.
- Gene and Cell Therapy Approaches:
- Research into genetic modulation to address congenital forms, especially in lymphedema-distichiasis syndrome.
- Future therapies may target underlying molecular pathways, aiming for long-term correction rather than repeated procedures.
- Innovative Follicle-Targeting Agents:
- Investigational pharmacologic compounds being tested to selectively suppress abnormal lash growth while sparing normal follicles.
- Teleophthalmology and Digital Monitoring:
- Remote follow-up tools help patients track symptoms, submit photos, and receive early intervention for regrowth or complications.
Practical Applications and Patient Engagement:
- Use mobile health apps to record symptoms, send photos to your doctor, and receive reminders for eyelid hygiene or scheduled treatments.
- Ask your provider about clinical trials or innovative therapies available in your area.
Long-tail Keywords Used:
- AI in eyelash disorder diagnosis
- gene therapy for congenital distichiasis
- robotic eyelid surgery
- future treatments for abnormal eyelashes
Clinical Trials and Anticipated Advancements
Current Research Directions:
- Novel Surgical Devices: Studies underway to evaluate next-gen cryoprobes, laser delivery systems, and radiofrequency instruments that minimize side effects and enhance lash removal accuracy.
- Pharmacologic Solutions: Trials for new topical agents aiming to inhibit lash regrowth without harming normal eyelid tissues.
- Gene Editing Techniques: Exploring CRISPR/Cas9-based correction for inherited distichiasis with lymphedema.
- Telemedicine-Facilitated Follow-Up: Research into digital platforms for home-based monitoring and early detection of complications.
Getting Involved in Clinical Trials:
- Participation offers access to new therapies and helps advance medical knowledge.
- Look for reputable research centers or discuss clinical trial opportunities with your specialist.
Looking Ahead:
- Personalized care models that integrate AI, genetic data, and digital monitoring promise to transform management.
- Ongoing innovations aim to make treatments more effective, less invasive, and widely accessible for all ages.
Long-tail Keywords Used:
- clinical trials for distichiasis
- new drugs for abnormal eyelashes
- gene editing eyelid disorders
- telemedicine for eyelid care
Frequently Asked Questions
What is distichiasis and how is it different from trichiasis?
Distichiasis is an extra row of lashes emerging from the meibomian glands, while trichiasis is misdirected normal lashes. Both can cause irritation, but their causes and treatments differ.
How can I treat distichiasis at home?
Mild cases may be managed with lubricating drops, lid hygiene, and careful epilation. If symptoms persist or vision is threatened, professional evaluation and procedural intervention are recommended.
What are the permanent solutions for abnormal eyelash growth?
Permanent options include electrolysis, cryotherapy, laser ablation, and surgical excision. The best method depends on lash location, number, and your individual medical history.
Are there any risks to repeated lash removal procedures?
Yes, repeated procedures may cause lid scarring, pigment changes, or notching. Discuss the risks and benefits with your ophthalmologist to minimize complications.
Can distichiasis be prevented?
Congenital forms cannot be prevented, but early recognition and management can prevent complications. For acquired cases, addressing chronic eyelid inflammation promptly may reduce risk.
Is distichiasis associated with any genetic syndromes?
Yes, congenital distichiasis often occurs with lymphedema-distichiasis syndrome and may be inherited. Genetic counseling can help affected families.
Disclaimer:
This article is intended for informational and educational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider with questions about your condition.
If you found this guide useful, please share it on Facebook, X (formerly Twitter), or your favorite social media platform—and don’t forget to follow us for more in-depth, practical health insights. Your support helps us continue to deliver trusted, high-quality medical content for everyone.






