Introduction to Endophthalmitis
Endophthalmitis is a serious and potentially vision-threatening condition that causes inflammation within the eye, primarily affecting the vitreous and/or aqueous humor. This condition is usually caused by an infection, but non-infectious causes, such as autoimmune responses or foreign bodies in the eye, can also cause inflammation. Endophthalmitis can develop after eye surgery, trauma, or even infections in other parts of the body, making it a serious concern for eye health. Recognizing and treating it early is critical to preserving vision and avoiding further complications.
Detailed Overview of Endophthalmitis
Endophthalmitis is divided into two types: exogenous and endogenous, based on how the infection enters the eye. Exogenous endophthalmitis occurs when infectious agents enter the eye directly, usually following surgery, trauma, or intraocular injections. Endogenous endophthalmitis occurs when pathogens infect other parts of the body and spread to the eye via the bloodstream.
Causes and Development
Endophthalmitis can be caused by a variety of bacteria, fungi, and, less frequently, viruses. Bacterial infections are the most common, with Gram-positive cocci, such as Staphylococcus and Streptococcus species, being the primary causes. Gram-negative bacteria, like Pseudomonas aeruginosa, are less common but can cause more serious infections. Fungal endophthalmitis is frequently caused by Candida species, particularly in people with weakened immune systems or who have undergone invasive medical procedures.
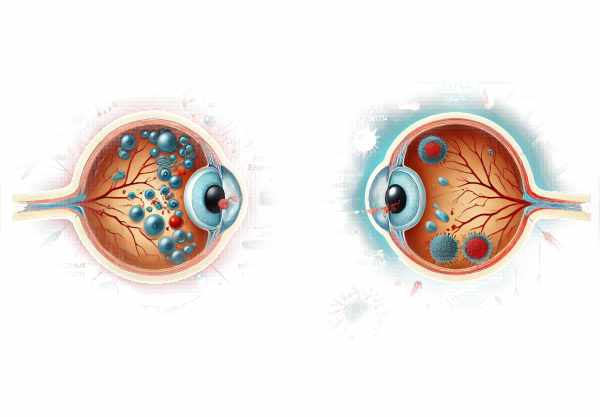
Endophthalmitis develops when pathogens enter the eye and cause inflammation. The vitreous humor, a gel-like substance in the eye, has no blood vessels, making it an ideal environment for microbes to thrive. The body’s inflammatory response includes immune cells and the release of various chemicals, which causes tissue damage and vision problems.
Symptoms and Signs
Endophthalmitis can cause a variety of symptoms, which typically appear suddenly. Severe eye pain, decreased vision, light sensitivity, and a red eye are among the most common symptoms. During an eye examination, redness, swelling, corneal cloudiness, pus in the front of the eye (hypopyon), and cloudy vitreous may be detected. Chronic endophthalmitis may produce milder symptoms, such as gradual vision loss and less noticeable inflammation.
Risk Factors
Several factors can raise the risk of getting endophthalmitis. Eye surgeries, particularly cataract surgery, are a significant risk factor because they are the most common procedures that cause this condition. Other risk factors include eye injuries, intravitreal injections (e.g., for age-related macular degeneration), weakened immune systems (as seen in diabetes or HIV/AIDS), and systemic infections that can spread to the eyes.
How it affects the eye
Understanding how endophthalmitis affects the eye entails investigating the interaction between microbes and the body’s immune response. When pathogens enter the eye, they are met with a blood supply that is limited, preventing immune cells and medications from reaching their destination. During the initial immune response, macrophages and microglial cells release chemicals such as IL-1 and TNF-α, which increase blood vessel permeability and attract neutrophils. This response, while intended to control the infection, can also harm the eye’s delicate structures, resulting in vision loss.
Microbes Involved
The microbes that cause endophthalmitis vary depending on the source of infection. Gram-positive cocci are frequently involved in postoperative endophthalmitis, with Staphylococcus epidermidis being the most common cause. Traumatic endophthalmitis is frequently associated with mixed infections containing both Gram-positive and Gram-negative bacteria. Endogenous endophthalmitis, caused by systemic infections, frequently involves pathogens such as Candida species, Aspergillus, and, less commonly, bacteria such as Streptococcus pneumoniae and Klebsiella pneumoniae.
Disease Progress and Outlook
Endophthalmitis progresses quickly and severely, necessitating immediate medical attention. Acute postoperative endophthalmitis usually appears within days to weeks of surgery, with sudden onset of symptoms. Chronic postoperative endophthalmitis, which is commonly caused by less aggressive organisms such as Propionibacterium acnes, can appear months or years later, with a slower onset and milder symptoms.
The prognosis for endophthalmitis is dependent on how quickly and effectively it is treated. The type of infecting organism, the severity of inflammation, and the timing of treatment all have an impact on the outcome. Early diagnosis and aggressive treatment can significantly improve visual outcomes, but severe cases may still result in significant vision loss or even eye removal.
Potential Complications
Endophthalmitis can cause a variety of complications, both short and long term. Immediate complications include retinal detachment, corneal damage, and elevated eye pressure (glaucoma). Long-term effects may include permanent vision impairment, cataract formation, and chronic inflammation. In severe cases, the infection can spread outside the eye, resulting in orbital cellulitis or systemic infection, especially in people with weakened immune systems.
Prevention Strategies
Endophthalmitis prevention is critical, especially during eye surgeries and other invasive procedures. Preoperative antisepsis, which includes using povidone-iodine to clean the skin and conjunctiva, has been shown to reduce infection risk. Maintaining a sterile environment during surgery and administering preventive antibiotics are also critical. Postoperative care includes keeping an eye out for signs of infection and acting quickly if symptoms appear.
Preventing endogenous endophthalmitis requires managing underlying health conditions and promptly treating systemic infections. People with risk factors, such as intravenous drug use or prolonged hospitalization, should be closely monitored for any signs of endophthalmitis.
Endophthalmitis: Diagnostic Techniques
Endophthalmitis is diagnosed using a combination of clinical assessments, laboratory tests, and imaging studies to confirm the infection and guide treatment.
Clinical Assessment
The first step in diagnosing endophthalmitis is to conduct a thorough clinical evaluation, which includes a detailed patient history to identify potential risk factors such as recent eye surgery, trauma, or systemic infections. Symptoms such as severe eye pain, vision loss, and light sensitivity should raise concerns. An eye examination may reveal redness, corneal swelling, pus in the front of the eye (hypopyon), and vitreous cloudiness. A comprehensive eye exam, including pupil dilation, is required to determine the extent of vitreous involvement and any complications.
Lab Tests
Laboratory tests are required to identify the causative organism and determine the best treatment option. Diagnostic vitrectomy and anterior chamber paracentesis are two procedures used to obtain samples of vitreous and/or aqueous humor. These samples are then subjected to Gram staining, culture, and sensitivity tests. Polymerase chain reaction (PCR) can be used to rapidly detect specific pathogens, particularly when cultures are negative. Blood cultures should be performed if endogenous endophthalmitis is suspected in order to identify any systemic infection sources.
Imaging Studies
Imaging tests aid in the diagnosis of endophthalmitis. B-scan ultrasonography is useful when direct visualization of the posterior eye is difficult due to media opacity. It can detect vitreous inflammation, retinal detachment, and other intraocular problems. Optical coherence tomography (OCT) generates detailed cross-sectional images of the retina and choroid, allowing for the assessment of structural damage and treatment response.
Additional Tests
Additional tests, such as anterior chamber paracentesis for cytology and flow cytometry, may be considered in exceptional cases or when cancer is suspected. These tests help distinguish infectious endophthalmitis from conditions that look like it, such as intraocular lymphoma.
Overall, diagnosing endophthalmitis necessitates a multifaceted approach that includes clinical evaluations, laboratory tests, and imaging studies. Early and accurate diagnosis is essential for initiating appropriate treatment, improving visual outcomes, and maintaining eye health.
Endophthalmitis: Standard and Emerging Treatments
Endophthalmitis treatment is multifaceted and often urgent, with the goal of eliminating the infection and controlling inflammation so that vision can be preserved. The standard treatment options are:
Intravitreal Antibiotics
Antibiotics are administered directly into the vitreous cavity as the primary treatment for bacterial endophthalmitis. Vancomycin is a common antibiotic used against Gram-positive bacteria, while ceftazidime or amikacin is used against Gram-negative bacteria. Antibiotics are chosen based on suspected or confirmed causative organisms.
Systemic Antibiotics
In addition to intravitreal antibiotics, systemic antibiotics are frequently used to treat potential systemic involvement and provide additional coverage. This approach is especially important for endogenous endophthalmitis.
Vitrectomy
Vitrectomy, a surgical procedure that removes the vitreous gel, is used in severe cases or when antibiotic therapy alone fails to provide significant improvement. This procedure reduces the load of infectious agents and inflammatory mediators, allowing for easier access to antibiotics and better visual results.
Corticosteroids
Corticosteroids can be used in conjunction with other treatments to reduce inflammation and protect tissues. They can be given intravenously, systemically, or topically. Corticosteroids should be used with caution, as they have the potential to suppress the immune response to infection.
Antifungal Treatment
Fungal endophthalmitis is treated with intravitreal and systemic antifungal agents such as amphotericin B or voriconazole. The treatment regimen is tailored to the specific fungal species and patient response.
Emerging Therapies
Endophthalmitis therapies that are innovative and emerging include the use of newer antimicrobial agents with broader spectrums and improved penetration into ocular tissues. Nanoparticles and drug delivery systems are being investigated for their ability to provide sustained release of antibiotics directly into the eye.
Adjunctive Treatment
Supportive care, such as pain management and monitoring for complications like high intraocular pressure, is critical. Advances in imaging and diagnostic techniques help to detect and treat endophthalmitis earlier.
Early intervention and a combination of these treatment strategies are critical for improving outcomes and maintaining vision in endophthalmitis patients.
Best Practices for Avoiding Endophthalmitis
- Preoperative Antisepsis: Prior to any intraocular procedure, thoroughly antiseptically prepare the periocular area using agents such as povidone-iodine.
- Sterile Techniques: Use strict sterile techniques during eye surgeries and procedures to reduce the risk of transmitting infectious agents.
- Prophylactic Antibiotics: To reduce infection risk, use appropriate prophylactic antibiotics prior to and following intraocular surgeries or injections.
- Postoperative Care: Closely monitor patients following surgery for early signs of infection and educate them on symptoms that require immediate medical attention.
- Proper Wound Management: To avoid infection, ensure that any ocular trauma is treated immediately and appropriately.
- Immunization: Stay up to date on vaccinations, especially for conditions such as influenza and pneumococcal disease, which can cause systemic infections that spread to the eye.
- Health Management: Effectively manage chronic conditions like diabetes to reduce your risk of developing endogenous endophthalmitis.
- Personal Hygiene: Encourage good personal hygiene practices, such as proper handwashing, particularly for those who handle contact lenses or administer eye medications themselves.
- Avoid Contaminants: Make sure that all eye medications and solutions are free of contaminants and properly stored.
- Regular Check-Ups: Regular eye exams, particularly for those at higher risk, can aid in the early detection and prevention of complications that may lead to endophthalmitis.
Trusted Resources
Books
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski and Brad Bowling
- “Ocular Infection: Investigation and Treatment in Practice” by Geoffrey Tabin and Matthew Oliva
- “Infectious Diseases of the Eye” by P. K. Mukherjee






