Introduction to Endothelial Dystrophy
Endothelial dystrophy is a collection of progressive eye disorders that primarily affect the cornea’s inner layer, known as the endothelium. This layer is essential for preserving corneal transparency by regulating fluid balance within the cornea. When endothelial cells deteriorate, it causes corneal swelling, cloudiness, and vision impairment. The most common type is Fuchs’ endothelial dystrophy, which usually appears in middle age or later. Understanding this condition is critical for early detection and effective treatment to avoid serious vision loss.
Endothelial Dystrophy: Clinical Insights
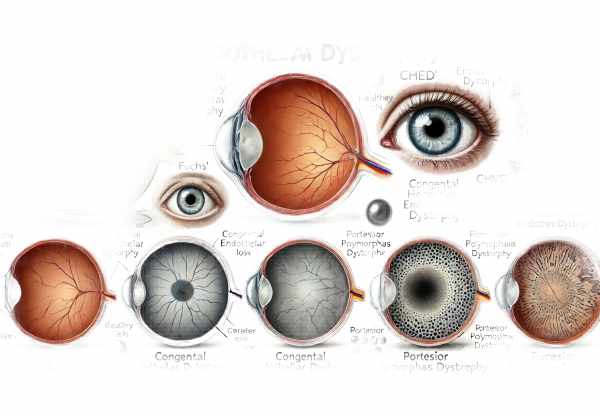
Endothelial dystrophy is a broad term that refers to a number of distinct disorders, the most common of which is Fuchs’. This condition causes a gradual loss of endothelial cells, resulting in corneal edema and vision problems. Other types of endothelial dystrophy include congenital hereditary endothelial dystrophy (CHED) and posterior polymorphous dystrophy (PPMD). Each type has distinct characteristics, but they all share the feature of endothelial cell dysfunction.
Pathophysiology
The corneal endothelium helps keep the cornea clear by pumping excess fluid out. Endothelial dystrophy occurs when endothelial cells degenerate or fail to function properly, resulting in fluid accumulation within the corneal stroma. This fluid buildup causes corneal swelling (edema), making vision blurry and hazy. As the endothelial cell count declines, the cornea’s ability to maintain a dehydrated state deteriorates, exacerbating swelling and cloudiness.
Fuchs Endothelial Dystrophy
Fuchs’ endothelial dystrophy is the most prevalent type of endothelial dystrophy. It usually affects both eyes and develops gradually over many years. Guttae, or tiny bumps on the back surface of the cornea, are present in the early stages of FED. As the condition progresses, the number of guttae increases, and the corneal endothelium becomes less efficient at removing fluid, resulting in corneal edema and vision problems. Patients frequently have blurred vision in the morning due to fluid accumulation overnight, which partially clears during the day as the eyes remain open.
Congenital Hereditary Endothelial Dystrophy(CHED)
CHED is a rare inherited form of endothelial dystrophy that manifests at birth or early childhood. It is caused by genetic mutations that alter the development and function of endothelial cells. CHED is classified into two types: CHED1 (inherited autosomally dominantly) and CHED2 (inherited autosomally recessively). Children with CHED typically have diffuse corneal clouding, which leads to significant vision impairment from a young age. Unlike Fuchs’ dystrophy, CHED does not progress with age, but the severity of the condition varies by individual.
Posterior Polymorphous Dystrophy(PPMD)
PPMD is another uncommon form of endothelial dystrophy that is typically inherited in an autosomal dominant manner. It can occur at any age and is frequently detected during routine eye examinations. PPMD is defined by abnormalities in endothelial cells, which can behave more like epithelial cells, resulting in the formation of abnormal cell layers on the back of the cornea. This condition can cause corneal edema and irregular corneal shape, resulting in visual disturbances. In some cases, PPMD may be linked to other eye conditions, such as glaucoma.
Symptoms and Signs
The symptoms of endothelial dystrophy differ according to the type and severity of the condition. Blurred vision, glare, halos around lights, and reduced visual acuity are all common symptoms, especially in low-light conditions. Patients with Fuchs’ endothelial dystrophy may notice that their vision is worse in the morning but improves throughout the day. As the disease progresses, persistent corneal edema can cause severe vision impairment and discomfort due to epithelial bullae (blisters) on the cornea.
Risk Factors
Several factors can increase the likelihood of developing endothelial dystrophy. Age is significant.
Risk factor, particularly for Fuchs’ endothelial dystrophy, which primarily affects people in their 50s and 60s. Endothelial dystrophy can run in families, so genetics plays a role. Another risk factor is a history of eye surgery or trauma, which can jeopardize the integrity and function of endothelial cells. In addition, women have a higher risk of developing Fuchs’ endothelial dystrophy than men.
Genetic influences
Genetic mutations play an important role in the development of different types of endothelial dystrophy. For example, mutations in the COL8A2 gene have been linked to early-onset Fuchs’ endothelial dystrophy. Similarly, mutations in the SLC4A11 gene are linked to CHED. These genetic insights have improved our understanding of disease mechanisms, paving the way for future genetic therapies.
Effects on Quality of Life
Endothelial dystrophy has a significant impact on a person’s quality of life. The gradual loss of vision has an impact on daily activities like reading, driving, and recognizing faces. Patients may experience emotional distress as a result of the disease’s progression and uncertainty about the future of their vision. Managing these effects through appropriate treatment and support is critical to maintaining overall well-being.
Pathological changes in the cornea
Endothelial dystrophy causes pathological changes primarily at the microscopic level. Endothelial cells, which form a single layer on the cornea’s inner surface, regulate fluid levels. In conditions such as Fuchs’ dystrophy, these cells form guttae and gradually lose their ability to maintain corneal dehydration. Histological examinations show cell loss, abnormal cell morphology, and thickening of Descemet’s membrane, which lies just beneath the endothelium.
Epidemiology
The prevalence of endothelial dystrophy varies by population. Fuchs’ endothelial dystrophy is more common in Europeans than in Asians and Africans. The condition is also slightly more common in women. Understanding these epidemiological patterns aids in the early detection and targeted treatment of at-risk populations.
Complications
As endothelial dystrophy progresses, complications may develop, resulting in further vision impairment. Chronic corneal edema can result in ongoing discomfort and pain. In severe cases, bullous keratopathy, which is distinguished by blister formation on the corneal surface, may develop. These complications frequently require surgical intervention to restore vision and relieve symptoms.
Patient Education and Support
Educating patients about endothelial dystrophy is critical for managing expectations and improving treatment adherence. Providing patients with information about the nature of the disease, its progression, and available treatment options allows them to make more informed decisions about their care. Support groups and counseling can also help patients deal with the emotional aspects of the disease.
Endothelial Dystrophy: Diagnostic Techniques
Endothelial dystrophy is diagnosed using a combination of clinical examination, imaging techniques, and genetic testing to confirm and assess the condition’s severity.
Clinical Examination
A thorough eye examination is the first step in diagnosing endothelial dystrophy. This includes a thorough patient history to identify symptoms and any family history of the condition. The slit-lamp examination is essential for determining the cornea’s clarity, the presence of guttae, and any signs of corneal edema. The slit lamp allows the ophthalmologist to examine the corneal layers and detect early signs of endothelial dystrophy.
Corneal Imaging
Advanced imaging techniques provide detailed views of the cornea, which aids in the diagnosis and management of endothelial dystrophy.
- Specular Microscopy: This non-invasive imaging technique produces high-resolution images of the corneal endothelium, allowing for the measurement of cell density, size, and shape. Specular microscopy is critical for identifying early endothelial changes and tracking disease progression.
- Anterior Segment Optical Coherence Tomography (AS-OCT): AS-OCT produces cross-sectional images of the cornea that show structural changes, corneal thickness, and the extent of edema. This imaging modality aids in quantifying corneal swelling and monitoring response to treatment.
- Confocal Microscopy: Confocal microscopy provides detailed images of the corneal layers at the cell level. It is especially useful for examining guttae, assessing endothelial cell health, and detecting inflammatory or fibrotic changes in the cornea.
Pachymetry
Pachymetry measures corneal thickness and is a useful diagnostic tool for determining the severity of corneal edema in endothelial dystrophy. The condition is characterized by increased corneal thickness, which indicates fluid accumulation caused by endothelial cell dysfunction. Pachymetry can be performed with ultrasound or optical devices, resulting in precise measurements that help guide treatment decisions.
Genetic Testing
When a hereditary form of endothelial dystrophy is suspected, genetic testing can reveal specific mutations associated with the condition. Identifying these genetic markers confirms the diagnosis while also providing useful information for genetic counseling and family planning. Genetic testing is especially important for congenital hereditary endothelial dystrophy (CHED) and early-onset Fuchs’ dystrophy.
Ancillary tests
Additional tests may be required to rule out other conditions that cause symptoms similar to endothelial dystrophy. These tests include:
- Keratometry: Measures the curvature of the cornea to detect irregularities or changes in its shape.
- Endothelial Cell Count: Using specular microscopy, the density of endothelial cells is measured, allowing for the quantification of cell loss and assessment of disease severity.
- Visual Acuity Testing: Determines the effect of corneal edema on vision clarity and aids in tracking changes over time.
Endothelial dystrophy is accurately diagnosed using a combination of these diagnostic methods, which provide a comprehensive understanding of the condition’s scope and progression. Early and accurate diagnosis is critical for initiating appropriate treatment and maintaining vision.
Endothelial Dystrophy Treatment Options
Endothelial dystrophy treatment varies according to its severity and type. Standard treatment options are intended to alleviate symptoms, reduce corneal edema, and improve visual acuity.
Standard Treatment Options
- Hypertonic Saline Drops and Ointment
- Hypertonic saline (5% sodium chloride) drops and ointments are commonly used to reduce corneal swelling by removing excess fluid from the cornea. These treatments can offer symptomatic relief, especially in the early stages of the disease.
- Hair dryers
- A hairdryer set to low heat and held at arm’s length can help evaporate excess moisture from the cornea, reducing morning corneal edema. Patients frequently use this method upon waking to improve their vision for the day.
- Contact lenses
- Specialized contact lenses, such as scleral lenses, can help manage corneal edema by providing a smooth refractive surface and a reservoir of saline solution to moisturize the cornea. These lenses can improve patients’ vision and comfort with advanced disease.
- Descemet Stripping Endothelial Keratoplasty (DSEK).
- DSEK is a surgical procedure that removes the diseased endothelial layer of the cornea and replaces it with a donor graft. This procedure is highly successful and less invasive than full-thickness corneal transplants.
- Descemet Membrane Endothelial Keratoplasty (DMEK)
- DMEK transplants only the thin Descemet membrane and endothelial cells, which leads to faster recovery and better visual outcomes than DSEK. This technique is gaining popularity because it is minimally invasive and produces excellent results.
Innovative and Emerging Therapies
- Genetic Therapy
- Gene therapy research aims to correct endothelial dystrophy-causing genetic mutations. These therapies, which target the underlying genetic causes, have the potential to halt or reverse disease progression.
- stem cell therapy
- Stem cell therapy is being investigated as a method for regenerating damaged endothelial cells. This approach, which involves transplanting stem cells that can differentiate into healthy endothelial cells, has the potential to restore cornea function and clarity.
- Rho Kinase inhibitors
- Rho kinase inhibitors are a class of drugs that have shown promise in increasing endothelial cell proliferation and migration. These drugs may improve the healing and regeneration of the corneal endothelium, providing a non-surgical treatment option.
- Artificial corneas
- Advances in biomaterials and tissue engineering are driving the development of artificial corneas. These synthetic implants have the potential to replace damaged corneal tissue, making them a viable option for patients who are not candidates for donor grafts.
- Nanotechnology for Drug Delivery
- Nanotechnology is being used to develop sophisticated drug delivery systems that can deliver medications directly to the corneal endothelium. These targeted therapies have the potential to improve treatment effectiveness while also reducing side effects.
Ongoing research and clinical trials continue to investigate these novel therapies, providing hope for more effective and less invasive endothelial dystrophy treatments in the future.
Best Practices to Prevent Endothelial Dystrophy
- Regular Eye Exam
- Have regular eye exams to detect early signs of endothelial dystrophy and monitor the health of your corneas.
- Managing Systemic Health Conditions
- Manage systemic conditions such as diabetes and hypertension, which can affect overall eye health and contribute to endothelial cell dysfunction.
- Protect your eyes
- Wear protective eyewear when participating in activities that may result in eye injury to avoid trauma that can cause endothelial cell damage.
- Avoid eye rubbing
- Avoid vigorously rubbing your eyes, as this can damage the corneal endothelium and worsen pre-existing conditions.
- Practice Proper Contact Lens Hygiene
- Maintain proper contact lens hygiene to avoid infections that can damage the corneal endothelium.
- Stay hydrated
- Stay hydrated to support overall eye health and avoid dry eye conditions, which can stress the corneal endothelium.
- Protect from UV light
- Protect your eyes from harmful ultraviolet rays that can damage the cornea by wearing UV-protective sunglasses.
- Avoid smoking
- Smoking can harm eye health, particularly the corneal endothelium. Quitting smoking lowers the risk of developing endothelial dystrophy.
- Monitor Medication Side Effects
- Be aware of medications that can have an impact on eye health, and discuss any potential side effects with your doctor.
- Genetic counseling
- If you have a family history of endothelial dystrophy, seek genetic counseling to better understand your risk and take proactive steps toward early detection and management.
Trusted Resources
Books
- “Corneal Dystrophies and Degenerations: A Molecular Genetics Approach” by David T. Azar
- “Cornea: Fundamentals, Diagnosis and Management” by Jay H. Krachmer
- “Corneal Endothelial Transplantation: DSEK, DMEK and Beyond” by Soosan Jacob






