Conjunctival melanoma is a rare yet potentially aggressive malignancy that arises from melanocytes within the conjunctiva—the thin membrane covering the white part of the eye and the inside of the eyelids. This tumor can pose significant threats to both vision and life due to its potential for local recurrence and distant metastasis. Early recognition, comprehensive evaluation, and tailored treatment are vital for optimal outcomes. In this guide, we will explore up-to-date therapies, innovative surgical approaches, and the latest research, all presented in a clear, accessible, and patient-focused manner to empower you or your loved ones facing this diagnosis.
Table of Contents
- Condition Overview and Epidemiology
- Conventional and Pharmacological Therapies
- Surgical and Interventional Procedures
- Emerging Innovations and Advanced Technologies
- Clinical Trials and Future Directions
- Frequently Asked Questions
- Disclaimer
Condition Overview and Epidemiology
Conjunctival melanoma is an uncommon but serious cancer originating from pigment-producing cells (melanocytes) in the conjunctiva. This malignancy presents most frequently in middle-aged and older adults, although it can occur at any age. Understanding its unique features, risk factors, and epidemiological patterns is essential for prompt recognition and intervention.
Key Features:
- Definition: A malignant neoplasm derived from melanocytes of the conjunctival epithelium.
- Common Sites: Most often arises on the bulbar conjunctiva (overlying the eyeball), but can also involve the palpebral conjunctiva (lining the eyelids), fornices, and caruncle.
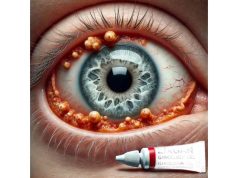
- Appearance: Typically appears as a raised, pigmented lesion with irregular borders and variable color (from dark brown/black to pink or amelanotic). It may be associated with feeder blood vessels.
Epidemiology:
- Incidence: Estimated at 0.2 to 0.8 cases per million per year—much rarer than cutaneous melanoma.
- Demographics: More common in fair-skinned individuals; no strong sex predilection.
- Risk Factors:
- Pre-existing conjunctival melanocytic lesions (primary acquired melanosis with atypia, nevus)
- UV light exposure
- Older age
- Genetic predisposition
- History of cutaneous melanoma or dysplastic nevus syndrome
Pathophysiology:
- Conjunctival melanoma can arise de novo, from a nevus, or more commonly from primary acquired melanosis (PAM) with atypia.
- The tumor exhibits variable growth patterns—may remain localized or invade local tissues, with potential for lymphatic or hematogenous spread, especially to lymph nodes, lungs, liver, or brain.
Clinical Presentation:
- Asymptomatic pigmented or non-pigmented mass on the conjunctiva
- Possible bleeding, irritation, foreign body sensation, or changes in appearance of pre-existing lesion
- Rarely, vision changes if the lesion invades the cornea or globe
Diagnosis:
- Comprehensive slit-lamp examination and high-resolution imaging (anterior segment OCT, ultrasound biomicroscopy)
- Incisional or excisional biopsy for histopathological confirmation
- Sentinel lymph node evaluation or imaging (ultrasound, MRI, PET/CT) to assess regional and systemic spread
Practical Advice:
If you notice a new, growing, or changing spot on the surface of your eye, especially with pigmentation or irregularity, consult an eye care specialist promptly. Early detection significantly improves prognosis.
Conventional and Pharmacological Therapies
Non-surgical management plays a vital role in both adjunctive and, in select cases, primary treatment of conjunctival melanoma. Medical therapy is often combined with surgical approaches to improve outcomes and minimize recurrence.
Primary Medical Management:
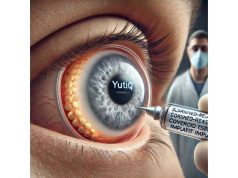
- Topical Chemotherapy:
- Mitomycin C (MMC): Most widely used agent, effective for residual microscopic disease, diffuse lesions, or in-situ components. Applied as eye drops in cycles, typically 0.02–0.04% for 1–2 weeks with drug-free intervals.
- Interferon alpha-2b: Used in cases resistant to MMC or with contraindications; may reduce tumor burden and recurrence risk.
- 5-Fluorouracil (5-FU): Less commonly used but may be considered for non-responsive or recurrent disease.
- Systemic Therapies:
- Targeted Therapy: BRAF and MEK inhibitors may be considered if mutations are present (especially in advanced or metastatic cases).
- Immunotherapy: Immune checkpoint inhibitors (e.g., pembrolizumab, nivolumab) are under investigation and may be offered for advanced or metastatic disease.
Adjunctive Treatments:
- Cryotherapy:
- Liquid nitrogen applied to lesion base or margins post-excision to destroy residual tumor cells and reduce recurrence risk.
- Radiation Therapy:
- Plaque brachytherapy (custom radioactive plaque placement) for local control in cases with positive margins or recurrent lesions.
- Proton beam or external beam radiotherapy may be considered when surgery is not feasible.
Symptom Management:
- Artificial tears and lubricating gels reduce irritation from topical drugs.
- Topical steroids may be prescribed briefly to control drug-induced inflammation (always under specialist care).
Practical Advice:
Adhere strictly to the prescribed dosing schedule for topical therapies. Wash hands before each application, and immediately report any increased pain, redness, or vision changes to your care team.
Surgical and Interventional Procedures
Surgery is the cornerstone of conjunctival melanoma treatment, aiming for complete tumor removal with maximal preservation of vision and cosmesis. Procedural strategies are personalized based on tumor size, location, and extent.
Surgical Techniques:
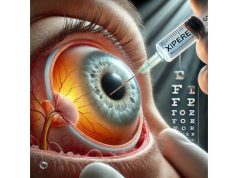
- Excisional Biopsy with “No Touch” Technique:
- Wide local excision of the tumor, minimizing direct manipulation to prevent seeding.
- Margins of 2–4 mm of healthy tissue are included; underlying Tenon’s capsule and sclera may be removed if involved.
- Alcohol Epitheliectomy:
- Application of absolute alcohol to the involved area to facilitate removal of atypical epithelial cells.
- Adjuvant Cryotherapy:
- Applied to surgical margins and bed to destroy microscopic residual tumor cells.
Advanced Interventions:
- Amniotic Membrane Transplantation:
- Used to reconstruct large defects post-excision and promote rapid healing with reduced scarring.
- Conjunctival Grafts or Flaps:
- Autografts or allografts help restore ocular surface integrity, improve cosmesis, and protect the globe.
- Sentinel Lymph Node Biopsy:
- Performed in select patients to assess regional lymphatic spread and guide further therapy.
Orbital Exenteration:
Reserved for extensive tumors invading the orbit or globe, where globe preservation is not possible. While vision is lost, it may be life-saving.
Postoperative Care:
- Topical antibiotics, steroids, and lubricants as prescribed
- Regular surveillance for recurrence with slit-lamp exams and imaging as needed
- Sun protection and vigilant self-monitoring
Potential Complications:
- Recurrence at the same or new site
- Scarring, symblepharon (adhesion of conjunctiva to eyelid), or dry eye
- Infection or, rarely, severe ocular surface disorders
Practical Advice:
Follow all postoperative instructions closely, attend all follow-up appointments, and alert your provider promptly if you notice new growths, redness, or discomfort.
Emerging Innovations and Advanced Technologies
Advances in oncology and ocular surgery have led to new and promising approaches for conjunctival melanoma management.
Targeted Molecular Therapy:
- Gene Profiling:
- Comprehensive genetic analysis of tumors identifies actionable mutations (BRAF, NRAS, KIT), guiding targeted drug selection.
- Immune Checkpoint Inhibitors:
- Drugs such as pembrolizumab or nivolumab have demonstrated effectiveness against metastatic conjunctival melanoma in selected cases.
Minimally Invasive Surgical Technologies:
- Micro-incision and Sutureless Techniques:
- Reducing tissue trauma, speeding recovery, and minimizing scarring.
- Custom Ocular Surface Reconstruction:
- Bioengineered conjunctival tissues and advanced graft materials help optimize healing in large defects.
Artificial Intelligence and Digital Surveillance:
- AI-Driven Image Analysis:
- Early studies show promise in AI tools for distinguishing benign from malignant conjunctival lesions, improving diagnostic accuracy.
- Teleophthalmology:
- Remote digital follow-up and triage platforms are expanding access to subspecialty care and postoperative monitoring.
Personalized Medicine:
- Liquid Biopsies:
- Investigational blood tests for circulating tumor DNA (ctDNA) offer hope for earlier detection of recurrence or metastasis.
Immunovirotherapy:
- Research is ongoing into engineered viruses that selectively target and kill tumor cells, potentially boosting anti-tumor immune responses.
Patient Engagement:
Ask your provider about clinical trial options or advanced molecular testing that may guide personalized therapy.
Clinical Trials and Future Directions
Clinical research in conjunctival melanoma is evolving rapidly, with new therapies and diagnostics under active investigation.
Active Areas of Research:
- Novel Immunotherapies:
- Ongoing trials of checkpoint inhibitors, adoptive cell transfer, and personalized cancer vaccines.
- Targeted Agents:
- Next-generation kinase inhibitors and combination therapies for tumors with specific mutations.
- Minimally Invasive Surgery:
- Research on refined surgical approaches and tissue-sparing technologies for improved outcomes.
- Digital Health and AI:
- Integration of artificial intelligence and digital platforms for early detection, monitoring, and remote patient engagement.
- Biomarkers and Prognostics:
- Identification of blood- or tissue-based biomarkers for better risk stratification and treatment planning.
Patient Opportunities:
- Many leading eye cancer centers and academic hospitals recruit for studies on new therapies, imaging, and genetic testing.
- Clinical trial participation may offer access to the latest interventions, often with intensive monitoring and support.
Future Outlook:
- Increasing use of precision medicine, less toxic systemic agents, and technology-driven diagnostics is expected to continue improving survival and quality of life.
Practical Advice:
Stay proactive and informed. If diagnosed with conjunctival melanoma, ask your specialist about clinical trial options and discuss all available treatments before making decisions.
Frequently Asked Questions
What is conjunctival melanoma and how is it diagnosed?
Conjunctival melanoma is a rare eye cancer from pigment cells on the eye’s surface. Diagnosis relies on detailed eye examination, imaging, and biopsy to confirm malignancy and determine the extent.
What are the treatment options for conjunctival melanoma?
Treatments include surgical excision, topical chemotherapy, cryotherapy, radiation, and, for advanced disease, targeted therapy or immunotherapy. Treatment plans are individualized based on tumor features.
Can conjunctival melanoma recur after treatment?
Yes, this tumor has a significant risk of recurrence. Regular follow-up visits and self-monitoring are essential to detect new or returning lesions early.
Is conjunctival melanoma life-threatening?
While some cases are localized, conjunctival melanoma can metastasize to lymph nodes or distant organs, making early diagnosis and comprehensive treatment critical for best outcomes.
Are there new treatments available for advanced conjunctival melanoma?
Yes, newer therapies include targeted drugs for specific mutations and immunotherapies such as checkpoint inhibitors, available through some specialists or clinical trials.
Should I consider joining a clinical trial for conjunctival melanoma?
Clinical trials may provide access to cutting-edge therapies and are especially valuable for advanced or recurrent disease. Discuss eligibility and options with your care team.
Disclaimer
The information in this guide is for educational purposes only and does not replace individualized medical advice. Always consult a qualified healthcare professional for diagnosis, treatment decisions, and follow-up related to conjunctival melanoma.
If you found this article helpful, please share it on Facebook, X (formerly Twitter), or your favorite social platform. Follow us for more expert insights and help us continue providing trusted, accessible eye health information by sharing with your network!