Waardenburg syndrome is a rare genetic disorder that causes auditory, pigmentary, and structural abnormalities. This condition is named after Dutch ophthalmologist Petrus Johannes Waardenburg, who first described it in 1951. It is characterized by distinctive facial features, varying degrees of hearing loss, and pigmentation changes in the skin, hair, and eyes. Among these features, ocular manifestations are important in diagnosing and characterizing the syndrome.
The presence of additional features beyond the core symptoms distinguishes Waardenburg syndrome into several types. The most common types are Waardenburg syndrome types 1 (WS1), 2 (WS2), 3 (WS3, also known as Klein-Waardenburg syndrome), and 4 (WS4, also known as Waardenburg-Shah syndrome). Each type has unique genetic and phenotypic characteristics, as well as varying levels of ocular involvement.
Genetic Basis for Waardenburg Syndrome
Mutations in a variety of genes, including PAX3, MITF, SOX10, SNAI2, and EDNRB, are the most common causes of Waardenburg syndrome. These genes play a role in the development and function of neural crest cells, which are essential for the formation of various tissues and structures during embryonic development, including melanocytes, which produce pigment in the skin, hair and eyes. Mutations in these genes disrupt normal melanocyte development, causing the distinctive pigmentary changes seen in Waardenburg syndrome patients.
- PAX3 Gene: Mutations in the PAX3 gene are most often linked to WS1 and WS3. The PAX3 gene is essential for the early development of neural crest cells, which help form facial bones, inner ear structures, and melanocytes.
- MITF Gene: Mutations in the MITF gene are most commonly associated with WS2. MITF is a transcription factor that controls melanocyte development and function, making it an important gene in the pigmentation abnormalities associated with Waardenburg syndrome.
- SOX10 Gene: Mutations in the SOX10 gene are linked to WS4 and some cases of WS2. SOX10 is involved in the development of both neural crest cells and enteric ganglia, which explains the link between WS4 and Hirschsprung disease, a condition characterized by the absence of nerve cells in certain parts of the intestines.
Ocular Symptoms of Waardenburg Syndrome
The ocular manifestations of Waardenburg syndrome are among the most noticeable and easily identifiable aspects of the condition. These manifestations are primarily associated with pigmentation abnormalities, but structural anomalies may also exist. The extent and severity of ocular involvement can differ greatly between individuals, even within the same family.
Heterochromia Iridum
One of the most well-known ocular manifestations of Waardenburg syndrome is heterochromia iridum, which occurs when an individual’s two irises are different colors. Heterochromia can be complete, in which one eye is a different color than the other, or sectoral, in which a portion of one iris is a different color than the rest.
- Complete Heterochromia: One iris has a completely different color than the other. This striking difference is frequently the most noticeable ocular sign of Waardenburg syndrome and can occur in a variety of colors, with blue and brown being the most common.
- Sectoral Heterochromia: Sectoral heterochromia, also known as partial heterochromia, occurs when only a portion of the iris has a different color than the rest of the iris. This can make a single eye appear to have multiple colors, with a clear distinction between the different hues.
Waardenburg syndrome causes heterochromia iridum due to a disruption in melanocyte function during eye development. Melanocytes are responsible for iris pigmentation, and when their development is disrupted, uneven pigment distribution occurs, resulting in the distinctive differences in eye color.
Hypopigmented Irides
In addition to heterochromia, people with Waardenburg syndrome may have hypopigmented irides. This means that the iris of both eyes is lighter in color than usual. In many cases, the iris may appear pale blue or grey. The severity of hypopigmentation varies, and in some people, it may be difficult to distinguish from normal eye color variations.
Waardenburg syndrome causes hypopigmentation of the irides due to a decrease in the number or dysfunction of melanocytes in the iris, resulting in decreased melanin production. Melanin is the pigment responsible for the coloration of the eyes, and its absence or reduction causes lighter-colored irises.
Dystopia Canthorum
Dystopia canthorum, a condition in which the inner corners of the eyes (the canthi) are farther apart than normal, is another distinguishing feature of Waardenburg syndrome, especially in WS1. Telecanthus, or wide spacing of the eyes, is frequently associated with a flattened nasal bridge and contributes to the syndrome’s distinctive facial appearance.
- Telecanthus vs. Hypertelorism: It is critical to distinguish telecanthus from hypertelorism. While both conditions involve wide spacing between the eyes, hypertelorism refers to an increased distance between the orbits (eye sockets), whereas telecanthus refers to an increased distance between the inner canthi that does not necessarily affect orbital spacing.
Dystopia canthorum is not usually associated with visual impairment, but it is an important diagnostic feature of Waardenburg syndrome and can help distinguish between the different types of the syndrome.
Additional Ocular Features
Other ocular abnormalities may be present in people with Waardenburg syndrome, though they are less common. This may include:
- Congenital Ptosis: Some people with Waardenburg syndrome may have congenital ptosis, which is when one or both eyelids droop. This can partially cover the eye and impair vision if severe.
- Strabismus: Eye misalignment, also known as strabismus, may occur. This condition can cause difficulties with binocular vision and depth perception.
- Aniridia: In rare cases, Waardenburg syndrome may be associated with aniridia, which is characterized by the absence of the iris. This can cause severe visual impairment and increased sensitivity to light (photophobia).
- Coloboma: Coloboma, a structural defect of the eye caused by incomplete closure of the optic fissure during development, is occasionally seen in Waardenburg syndrome. Colobomas can affect any part of the eye, including the iris, retina, choroid, or optic nerve, and can cause visual impairment depending on the size and location of the defect.
- Microphthalmia: Rarely, people with Waardenburg syndrome develop microphthalmia, a condition in which one or both eyes are abnormally small. This can cause significant visual impairment or blindness in the affected eye.
Impact on Vision
The effect of Waardenburg syndrome on vision varies according to the specific ocular manifestations and their severity. In many cases, Waardenburg syndrome’s ocular features, such as heterochromia iridum and dystopia canthorum, have no direct effect on visual acuity or eye function. However, when structural abnormalities such as coloboma, aniridia, or microphthalmia are present, significant visual impairment can occur.
- Normal Vision: Many people with Waardenburg syndrome have normal vision despite the presence of heterochromia or dystopia canthorum. These characteristics are primarily cosmetic in nature and do not interfere with the visual pathway or the eye’s ability to focus light.
- Visual Impairment: When structural abnormalities such as coloboma or aniridia are present, visual impairment can be mild to severe. Colobomas can create visual field gaps, whereas aniridia can cause light sensitivity and reduced visual acuity. Microphthalmia can cause blindness in the affected eye if the condition is severe.
- Impact of Strabismus: Strabismus, if present, can progress to amblyopia (lazy eye) if not treated, especially in children. This condition occurs when the brain favors one eye over the other, resulting in reduced vision in the affected eye. Amblyopia can cause permanent vision loss, so early intervention and treatment are critical.
Diagnostic methods
Waardenburg syndrome, particularly its ocular manifestations, requires a combination of clinical examination, family history analysis, and genetic testing. The diagnosis is primarily clinical, based on the recognition of characteristic features; however, genetic testing can confirm the diagnosis and aid in the differentiation of the various types of the syndrome.
Clinical Examination
A thorough clinical examination by an ophthalmologist is required to diagnose the ocular manifestations of Waardenburg syndrome. This exam typically includes:
- Visual Acuity Testing: A visual acuity test is used to assess how any ocular abnormalities affect vision. This test assesses vision clarity and can aid in the detection of visual impairments associated with the syndrome.
- Slit-Lamp Examination: A slit-lamp examination allows the ophthalmologist to thoroughly examine the eye’s anterior structures, such as the iris, cornea, and lens. This examination is especially effective in detecting heterochromia iridum, hypopigmented irides, and other anterior segment abnormalities.
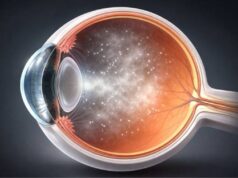
- Fundus Examination: A fundus examination consists of examining the back of the eye, including Retina, optic disc, and blood vessels. This examination is critical for detecting any retinal abnormalities, such as coloboma or pigmentation changes, that may be present in people with Waardenburg syndrome. The use of an ophthalmoscope or fundus photography allows the ophthalmologist to document any structural abnormalities that may impair vision.
To evaluate dystopia canthorum, the ophthalmologist measures the distance between the inner canthi (telecanthus) and compares it to normal standards for the patient’s age and ethnic background. This measurement helps determine whether the spacing between the eyes is normal or indicative of Waardenburg syndrome.
- Assessment for Strabismus and Ptosis: The clinical examination will also include an assessment for strabismus (eye misalignment) and ptosis (eyelid drooping). If any of these conditions exist, they may necessitate additional evaluation and management in order to avoid visual complications like amblyopia.
Genetic Testing
Genetic testing is critical for confirming the diagnosis of Waardenburg syndrome and distinguishing between its various types. Genetic testing can provide definitive evidence of the condition by detecting mutations in the syndrome-associated genes (such as PAX3, MITF, SOX10, SNAI2, and EDNRB).
- Targeted Gene Sequencing: Targeted gene sequencing examines specific genes known to be associated with Waardenburg syndrome. This method is especially useful when clinical features strongly indicate a specific type of Waardenburg syndrome, such as WS1 or WS2.
- Next-Generation Sequencing (NGS): If the diagnosis is unclear or multiple genetic conditions are suspected, next-generation sequencing (NGS) may be used. NGS can analyze multiple genes at the same time and detect mutations that targeted sequencing cannot.
- Prenatal Testing: In families with a history of Waardenburg syndrome, prenatal genetic testing can be used to detect the syndrome in a developing fetus. This information can help families prepare for the potential difficulties associated with the condition.
Family History Analysis
A detailed family history is required for diagnosis because Waardenburg syndrome is inherited in an autosomal dominant manner, which means that a single copy of the mutated gene is enough to cause the condition. Affected individuals have a 50% chance of passing the condition down to their children. Clinicians can identify inheritance patterns and assess the risk of the syndrome reoccurring in future generations by analyzing family histories.
- Pedigree Analysis: Pedigree analysis is the process of mapping out the family tree in order to identify other affected relatives and trace the condition’s inheritance pattern. This analysis can help determine whether the syndrome is inherited or the result of a new mutation in the affected individual.
- Counseling for Genetic Risk: Genetic counseling is frequently recommended for families with a history of Waardenburg syndrome. Counseling teaches about the risk of inheritance, the implications of genetic testing, and the various options for family planning and management.
Imaging Studies
When structural ocular abnormalities are suspected, imaging studies can provide more information about the eye’s anatomy. The studies include:
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina and optic nerve. OCT is useful in determining the extent of retinal colobomas and other structural abnormalities that may impair vision.
- Ultrasound Biomicroscopy (UBM): UBM uses high-frequency ultrasound to visualize the eye’s anterior segment, which includes the iris, lens, and ciliary body. This imaging modality can help detect abnormalities in these structures that may not be visible with a standard slit-lamp examination.
- Magnetic Resonance Imaging (MRI) or Computed Tomography (CT): In rare cases where craniofacial abnormalities exist, MRI or CT scans may be used to assess the orbital bones and surrounding tissues. These imaging studies can help identify any structural issues that may be causing ocular manifestations in Waardenburg syndrome.
Waardenburg Syndrome Ocular Manifestations Management
The management of ocular manifestations in Waardenburg syndrome is tailored to each individual’s specific symptoms and complications. Waardenburg syndrome is a genetic condition with a variety of ocular manifestations, so treatment is frequently multidisciplinary, involving ophthalmologists, geneticists, and other specialists as needed. The primary goals of management are to preserve vision, address any cosmetic concerns, and provide supportive care for related conditions.
Regular Ophthalmic Monitoring
Regular ophthalmic monitoring is critical in the management of Waardenburg syndrome. Individuals with Waardenburg syndrome should have routine eye exams throughout their lives because there is a risk of progressive ocular changes or complications developing.
- Early Detection of Complications: Regular eye exams can help detect problems like strabismus, cataracts, and retinal abnormalities early on, allowing for timely treatment. Early detection and treatment of strabismus or amblyopia (lazy eye) is critical for children with Waardenburg syndrome in order to avoid long-term vision problems.
- Visual Acuity Monitoring: Periodic visual acuity assessments are critical, especially for people who have structural abnormalities such as coloboma or aniridia, which can impair vision. Any changes in visual acuity should prompt additional investigation and intervention.
Correction of Refractive Errors
Many people with Waardenburg syndrome may have refractive errors, including myopia (nearsightedness), hyperopia (farsightedness), or astigmatism. Corrective lenses, such as glasses or contact lenses, can help to improve visual acuity and quality of life.
- Glasses or Contact Lenses: These are the primary ways to correct refractive errors. In cases of strabismus, prismatic lenses can be used to help align the eyes and reduce double vision.
- Surgical Correction: If non-surgical methods fail to correct significant strabismus, surgery may be required. This procedure involves adjusting the muscles surrounding the eyes to improve alignment, which improves both appearance and binocular vision.
Management of Structural Abnormalities
Certain structural abnormalities associated with Waardenburg syndrome, such as coloboma, aniridia, or microphthalmia, may necessitate specialized management strategies to prevent or treat vision loss.
- Coloboma Management: There is no cure for coloboma, but management aims to maximize the remaining vision. This may entail the use of low-vision aids or, in some cases, surgical procedures to repair large colobomas that affect the retina or optic nerve. Sunglasses may be recommended to protect the eyes from excessive light exposure, particularly if the coloboma affects the iris.
- Aniridia Management: Aniridia can cause extreme light sensitivity and visual impairment. To reduce photophobia and improve comfort, management may suggest wearing tinted contact lenses or sunglasses. In severe cases, surgical procedures such as implanting an artificial iris may be considered.
- Microphthalmia Treatment: Microphthalmia can cause severe visual impairment or blindness in the affected eye. Management focuses on improving vision in the better-seeing eye and, if necessary, providing cosmetic solutions such as prosthetic eyes to enhance appearance.
Genetic Counseling and Support
Waardenburg syndrome is a genetic condition, so genetic counseling is an important part of treatment. Genetic counselors can help family members understand inheritance patterns, recurrence risks, and the implications.
- Prenatal and Family Planning Counseling: Genetic counseling can help families with a known history of Waardenburg syndrome make decisions about prenatal testing and family planning. This can help prospective parents make more informed decisions about their reproductive health.
- Psychosocial Support: Living with a genetic condition such as Waardenburg syndrome can have a psychological impact, especially for people who have visible ocular or facial differences. Counseling and support groups can help people deal with the social and emotional challenges that come with the syndrome.
Addressing Cosmetic Concerns
Some people may be concerned about the cosmetic impact of Waardenburg syndrome, especially in cases of heterochromia iridum or dystopia canthorum. While these characteristics do not usually affect vision, they can be treated if they cause significant distress.
- Cosmetic Contact Lenses: Individuals with heterochromia who want to have more uniform eye color can use cosmetic contact lenses to change the appearance of the iris. These lenses can match the color of a darker or lighter eye, depending on the individual’s preference.
- Surgical Options for Telecanthus: If dystopia canthorum is a major cosmetic concern, surgical correction of telecanthus may be considered. This procedure, known as medial canthoplasty, repositions the inner corners of the eyes to create a more natural appearance.
Prevention of Vision Loss
For people with Waardenburg syndrome, preventing vision loss is a top priority. This entails not only treating existing conditions but also implementing preventive measures to safeguard eye health.
- Regular Eye Protection: People with structural ocular abnormalities like aniridia or coloboma are more susceptible to UV light damage. Wearing UV-protected sunglasses is an important precaution to protect the eyes from further damage.
- Management of Associated Conditions: Conditions like glaucoma, which can develop in conjunction with aniridia or other structural abnormalities, necessitate close monitoring and prompt treatment to avoid vision loss. Maintaining vision requires regular intraocular pressure checks and appropriate management, which may include medications or surgery.
Trusted Resources and Support
Books
- “Waardenburg Syndrome: Genetics, Clinical Features, and Management” by Alan L. Edmunds
- This comprehensive guide provides an in-depth look at Waardenburg syndrome, including its genetic basis, clinical manifestations, and management strategies. It is a valuable resource for both healthcare professionals and individuals living with the condition.
- “Genetic Diseases of the Eye” by Elias I. Traboulsi
- This book offers detailed information on various genetic eye conditions, including Waardenburg syndrome. It covers the genetic underpinnings, clinical presentations, and management approaches, making it an essential reference for understanding the ocular aspects of genetic disorders.
Organizations
- National Organization for Rare Disorders (NORD)
- NORD provides extensive resources and support for individuals with rare genetic conditions, including Waardenburg syndrome. Their website offers information on diagnosis, treatment options, and patient support services.
- American Academy of Ophthalmology (AAO)
- The AAO offers a wealth of information on eye health and genetic eye conditions. Their resources include educational materials on Waardenburg syndrome, as well as guidance on finding specialists and accessing appropriate care.