Introduction to Acrochordon
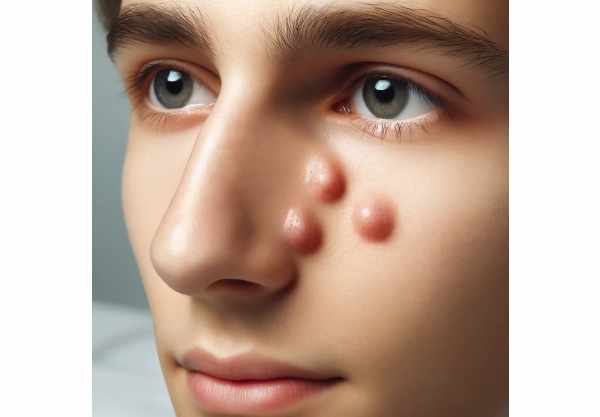
Acrochordon, also known as skin tags, is a benign condition marked by small, soft, flesh-colored growths that appear in areas where the skin creases. Although not harmful, these growths can be a cosmetic concern and occasionally cause discomfort or irritation, especially in sensitive areas like the eyes. Awareness and early detection of acrochordons are critical for effective management, especially since these growths can be mistaken for other dermatologic conditions. Early intervention can also help to avoid complications like bleeding or infection caused by prolonged friction or self-removal attempts.
Understanding The Condition
Acrochordons are pedunculated lesions, which means they are attached to the skin by a thin stalk. They are made up of loose collagen fibers, blood vessels, and occasionally fat cells that are covered by an epidermal layer. While the exact cause of acrochordon formation is unknown, several factors contribute to its development:
- Genetic Predisposition: A familial tendency has been observed, indicating a genetic component in the development of skin tags.
- Friction and Irritation: Skin tags are commonly found in areas where skin rubs against skin or clothing, such as the neck, armpits, groin, and eyelids. Mechanical irritation and constant friction in these areas are thought to promote the development of skin tags.
- Metabolic Syndrome and Obesity: Acrochordons are strongly associated with metabolic disorders. Obesity and metabolic syndrome are associated with an increased risk of developing skin tags. This association is thought to be linked to insulin resistance, which can result in elevated levels of growth factors that promote skin tag formation.
- Hormonal Changes: Hormonal fluctuations, especially during pregnancy, can cause the development of skin tags. During pregnancy, estrogen and progesterone levels are thought to rise, which contributes to their formation.
- Human Papillomavirus (HPV): Some studies indicate a link between HPV infection and the development of skin tags. HPV DNA has been found in a subset of skin tags, implying that viral infection may contribute to their development.
- Aging: As people get older, they are more likely to develop skin tags. They are more common in middle-aged and elderly people, most likely due to repeated exposure to friction and other risk factors over time.
Clinical Presentation
Skin tags are typically asymptomatic and appear as small, soft, flesh-colored or lightly pigmented papules. They can range in size from a few millimeters to several centimeters. They can cause cosmetic issues or occasionally interfere with vision if they grow large enough. Torsion of skin tags can cause necrosis and secondary infection, which can be painful in rare cases.
Differential Diagnosis
To avoid misdiagnosis, it is critical to distinguish acrochordon from a variety of other conditions that can resemble skin tags.
- Seborrheic Keratosis: These harmless growths can resemble skin tags, but they are usually more keratinized and have a warty surface.
- Fibroepithelial Polyps: These resemble skin tags but are typically larger and have a broader base.
- Nevus: A pigmented nevus, also known as a mole, can resemble a skin tag, especially if pedunculated.
- Basal Cell Carcinoma (BCC): In rare cases, a BCC may appear as a pedunculated lesion, making differentiation critical.
- Melanoma: Although rare, melanoma, particularly the nodular subtype, can occasionally present as a pedunculated growth. Any suspicious or rapidly changing lesion should be investigated with a biopsy.
Pathophysiology
Skin tags are caused by a combination of mechanical, hormonal, and possibly infectious factors, which result in the proliferation of fibrovascular tissue. The role of insulin-like growth factor (IGF) in the formation of skin tags has been highlighted, particularly in people with metabolic syndrome. IGF is known to promote cell growth and proliferation, and high levels in insulin resistance may contribute to skin tag formation.
Psychological and Social Impact
Although skin tags are harmless, their presence, especially around the eyes, can have serious psychological and social consequences. They can lower a person’s self-esteem and body image, causing distress and social embarrassment. Addressing these concerns with appropriate management and treatment options is critical to the patient’s overall well-being.
Treatment
Treatment for acrochordon is rarely medically necessary, but it may be sought for cosmetic reasons or if the skin tags cause discomfort. There are several treatment options available.
- Cryotherapy: This involves freezing the skin tag with liquid nitrogen, which causes it to fall off within a few days. Cryotherapy is quick and effective, but it can cause temporary discomfort and blisters.
- Electrosurgery: This technique involves burning off the skin tag with an electric current. It is effective and produces immediate results, but it requires local anesthesia to alleviate discomfort.
- Surgical Excision: Small skin tags can be removed using scissors or a scalpel while under local anesthesia. Larger or multiple skin tags may necessitate more extensive surgical procedures. Surgical excision produces immediate results but has a low risk of scarring and infection.
- Ligation: In this method, a string or suture is tied around the base of the skin tag to cut off its blood supply, causing it to wither and fall off. Ligation is simple and can be performed at home, but the skin tag may take several days to fall off completely.
Innovative and Emerging Therapies
Innovative skin tag treatments are constantly being developed in order to improve efficacy and reduce discomfort. Laser therapy, for example, employs concentrated light energy to remove skin tags with minimal discomfort and scarring. This technique is gaining popularity due to its precision and aesthetic results. Furthermore, research into topical treatments that can dissolve skin tags non-invasively is underway, with the promise of simpler and less invasive options for patients.
Emerging therapies are also investigating the role of antiviral treatments, particularly in cases of HPV infection. These treatments, which target the underlying viral cause, have the potential to prevent the recurrence of skin tags and provide a more permanent solution.
Essential Preventive Measures
To reduce the risk of developing acrochordon, especially around the eyes, consider the following preventive measures:
- Maintain Healthy Weight: Because obesity is a risk factor, eating a well-balanced diet and exercising regularly can help reduce the likelihood of developing skin tags.
- Reduce Friction: Avoid tight clothing and limit skin-to-skin contact in areas prone to friction. To reduce irritation, use talcum powder or barrier cream.
- Manage Blood Sugar Levels: For people with metabolic syndrome or diabetes, managing blood sugar levels through diet, exercise, and medication can help prevent skin tags from forming.
- Regular Skin Examinations: Perform regular self-examinations of your skin, particularly in areas where skin tags are common. Early detection enables timely management.
- Prevent Skin Trauma: Treat your skin gently, especially in areas prone to friction. To avoid irritation and complications, don’t scratch or pick at existing skin tags.
- Consult a Dermatologist: Schedule regular dermatological appointments, especially if you have a family history of skin tags or other skin conditions. A dermatologist can offer personalized advice and early intervention if necessary.
Trusted Resources
Books
- “Clinical Dermatology” by Thomas P. Habif
- “Dermatology” by Jean L. Bolognia, Joseph L. Jorizzo, and Julie V. Schaffer
- “Fitzpatrick’s Dermatology in General Medicine” by Klaus Wolff and Lowell A. Goldsmith






