Shining a Light on Innovation: A New Way to Manage Glaucoma
Glaucoma remains one of the foremost causes of irreversible blindness worldwide. Characterized by progressive optic nerve damage, it often stems from elevated intraocular pressure (IOP) due to poor aqueous humor drainage. Although pharmaceutical eye drops, lasers, and incisional procedures have long formed the backbone of glaucoma management, they may fail to control IOP in some patients or require complex regimens that erode adherence. As the disease advances, optimizing the outflow of aqueous fluid—thereby reducing chronic optic nerve stress—becomes paramount.
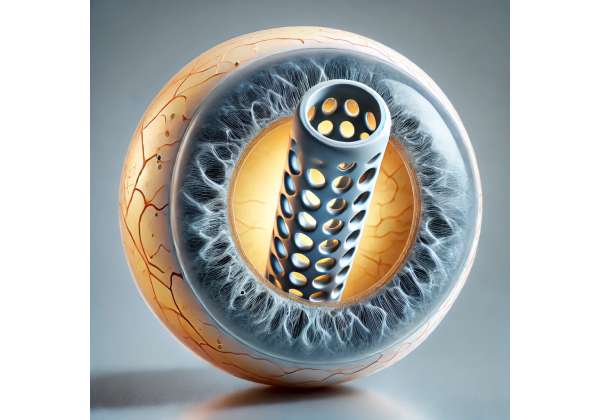
Enter the EyeFlow Stent, a next-generation, minimally invasive device designed to facilitate aqueous humor drainage and stabilize IOP long-term. The EyeFlow Stent builds on the successes of earlier microinvasive glaucoma surgery (MIGS) approaches while also addressing their limitations. By providing a consistent outflow pathway with minimal tissue disruption, the EyeFlow Stent can help people maintain healthier IOP levels with fewer medications and potentially fewer follow-up procedures. Coupled with an emphasis on patient-friendly design, this novel stent seeks to simplify glaucoma treatment and boost patient quality of life.
Below, we explore the EyeFlow Stent in detail—covering everything from its working principles and potential advantages to real-world treatment protocols, preliminary research findings, and cost considerations. Whether you’re a patient looking for new options or a clinician seeking advanced treatments, the EyeFlow Stent may offer a transformative path to long-lasting IOP control.
Understanding the Therapy: Key Insights into the EyeFlow Stent
Glaucoma results from impaired outflow of aqueous humor, the clear fluid that nourishes the lens and cornea while regulating intraocular pressure. Various anatomical or physiological changes in the trabecular meshwork, Schlemm’s canal, or other drainage structures can raise IOP. Over time, elevated IOP damages retinal ganglion cells and the optic nerve head, culminating in progressive, irreversible vision loss.
What Makes the EyeFlow Stent Unique
Building on years of MIGS innovation, the EyeFlow Stent aims to simplify and enhance fluid outflow. Earlier devices like the iStent, XEN Gel Stent, or Hydrus Microstent have significantly reduced dependence on eye drops and improved patient satisfaction. The EyeFlow Stent introduces further refinements:
- Advanced Material: EyeFlow is constructed from a biocompatible polymer or titanium alloy (depending on the model) optimized for minimal inflammatory response and robust long-term patency. Some designs feature a specialized surface coating to deter biofilm formation or fibrotic encapsulation.
- Streamlined Design: The stent is typically very small—only a few millimeters in length—and shaped to anchor securely within the eye’s drainage structures without risking migration or corneal contact.
- Enhanced Flow Control: By creating a predictable conduit, EyeFlow fosters a steady rate of fluid drainage, helping maintain target IOP levels without significant fluctuation. Certain variants have microvalves or flow-regulating elements that adapt to changes in ocular pressure.
- Minimally Invasive Insertion: Surgeons often implant the device via microincision approaches, preserving conjunctival tissue and reducing scarring compared to more extensive filtering surgeries (like trabeculectomy).
Targeted Drainage Pathways
Where exactly does the fluid go? The EyeFlow Stent is typically placed in the trabecular meshwork or suprachoroidal space, depending on the stent type and surgical approach:
- Trabecular Bypass: In open-angle glaucoma, placing the stent to bypass the diseased trabecular meshwork allows fluid to flow directly into Schlemm’s canal, facilitating physiological outflow.
- Uveoscleral Pathway: Alternative devices direct fluid to the suprachoroidal or subconjunctival space, creating new drainage routes and lowering IOP. EyeFlow variants may tap either or both pathways, depending on clinical strategy.
Whichever route the stent takes, the goal is to restore or augment natural drainage with minimal disruption, resulting in better patient comfort and fewer complications than traditional filtering surgeries that rely on large blebs or external drainage devices.
Combining EyeFlow with Other Interventions
No single therapy fits every glaucoma scenario. The EyeFlow Stent frequently works best in conjunction with:
- Pharmacological Support: Some patients remain on a reduced number of eye drops post-stent implantation. For instance, a single topical medication can sometimes suffice in place of a multi-drop regimen.
- Cataract Surgery: Many MIGS devices, including EyeFlow, can be implanted simultaneously with cataract extraction. This synergy streamlines operative times and uses the same incision site, often maximizing patient benefit.
- Laser Therapies: If additional IOP reduction is needed, selective laser trabeculoplasty (SLT) or other lasers can supplement stent function.
- Advanced Disease Management: In severe or refractory glaucoma, EyeFlow can be part of a staged approach, perhaps preceding a more traditional tube shunt if necessary.
By meshing seamlessly with existing glaucoma treatments, the EyeFlow Stent expands therapeutic flexibility, letting ophthalmologists tailor solutions for each patient’s ocular anatomy and disease severity.
Implementation: Surgical Techniques and Treatment Protocols
Despite the EyeFlow Stent’s minimal invasiveness, expert surgical technique and thorough patient evaluation remain critical. Successful outcomes hinge on precise device placement, appropriate anesthesia, and vigilant postoperative care.
Preoperative Assessment
Patient Selection: EyeFlow is best suited for individuals with mild to moderate primary open-angle glaucoma (POAG) who have not achieved sufficient IOP control with medications alone or who cannot tolerate or adhere to multi-drop regimens. Patients who require moderate IOP lowering (e.g., mid-teen targets) often benefit the most from MIGS-based solutions. Additionally:
- Those with visually significant cataracts needing surgery might elect combined phacoemulsification and EyeFlow insertion.
- Individuals with advanced or secondary glaucomas (e.g., neovascular or uveitic) may require alternative or adjunctive measures, as MIGS devices alone might be insufficient.
- Angle-closure glaucomas typically need angle-opening procedures (like goniosynechialysis) or other specialized approaches before a stent can help.
Diagnostic Imaging: Gonioscopic examinations, anterior segment OCT (AS-OCT), or ultrasound biomicroscopy can reveal angle anatomy, identify peripheral anterior synechiae, and confirm feasibility for stent placement.
Medical Optimization: Thoroughly controlling systemic factors—like blood pressure, diabetes, or inflammatory conditions—can help ensure stable wound healing and reduce the risk of postoperative spikes. Patients on anticoagulants may require dose adjustments to minimize surgical bleeding risks.
Surgical Workflow
- Anesthesia and Incision: Typically performed under topical or local anesthesia in an outpatient setting. Surgeons create a small corneal incision, often the same used for cataract extraction if combining both procedures.
- Gonioscopic Guidance: A gonio lens helps visualize the angle structures. The EyeFlow Stent is loaded onto a specialized inserter that guides it toward the desired location.
- Stent Insertion: With careful micro-movements, the surgeon advances the stent into the trabecular meshwork (or suprachoroidal region, depending on model). A secure anchoring is checked to confirm stable placement.
- Verification: Gentle irrigation or slight vitreous humor manipulation ensures correct stent orientation. Surgeons may observe fluid egress or verify stable IOP.
- Wound Closure: In many cases, the microincision is self-sealing. Otherwise, a single suture or ocular sealant can secure it. Combined phaco-EyeFlow procedures end with intraocular lens placement followed by stent insertion.
Postoperative Care
Medication Adjustments: While the EyeFlow Stent aims to reduce medication burden, patients often continue some eyedrops initially—such as steroids or antibiotic prophylaxis—to prevent inflammation and infection. Gradual tapering of IOP-lowering medications occurs based on postoperative results and IOP readings.
Follow-Up Visits: Standard follow-up might involve checks at day 1, week 1, and monthly intervals for the first few months. These appointments monitor:
- IOP stability or reductions.
- Detection of any stent occlusion, migration, or undue scarring.
- Corneal health, given that malpositioned stents can injure the endothelium if they contact corneal tissue.
Lifestyle and Eye Protection: Patients should avoid strenuous activities that increase venous pressure for a short time after surgery. They may also need to temporarily skip contact lens wear or heavy rubbing of the eyes until the incision fully stabilizes.
Troubleshooting and Reoperations
A small fraction of patients may see insufficient IOP lowering due to stent misplacement, angle scarring, or advanced disease. Revision procedures or additional MIGS implants can be considered, though removing or repositioning the original stent might pose technical challenges. In complicated scenarios, more traditional filtering surgeries, tube shunts, or cyclodestructive procedures remain potential fallback options.
In sum, while the EyeFlow Stent procedure is substantially simpler than full filtering surgeries, meticulous planning and execution are essential to ensure robust results. By skillfully integrating the stent into a patient’s broader glaucoma treatment plan, surgeons can leverage this advanced technology to offer stable, durable IOP reductions with minimal postoperative disruption.
Latest Clinical Insights: Research and Studies on the EyeFlow Stent
Early-Stage Trials and Observational Reports
The EyeFlow Stent’s journey began with small pilot trials assessing feasibility in mild to moderate open-angle glaucoma patients. Preliminary data revealed:
- Consistent IOP Reductions: Many participants achieved a 20–30% drop in IOP, sometimes dipping into the mid-teens.
- Reduced Medication Dependence: Over half reduced their medication burden by at least one class of glaucoma drug after 6–12 months.
- Minimal Invasive Footprint: Adverse events (e.g., transient hypotony, mild corneal edema) resolved quickly, indicating a favorable safety profile.
These initial findings prompted expanded prospective studies to confirm the device’s reliability across broader patient populations and to refine insertion techniques.
Randomized Controlled Trials (RCTs)
More robust RCTs soon followed, often comparing EyeFlow Stent implantation with standard approaches, such as selective laser trabeculoplasty (SLT) or standalone medication therapy. Key outcomes included:
- Equivalent or Superior IOP Control: At 1-year follow-up, EyeFlow groups typically matched or slightly outperformed baseline treatments, achieving stable IOP in the 14–17 mmHg range without additional interventions.
- Greater Quality-of-Life Scores: Surveys frequently indicated improved convenience, fewer daily drops, and less ocular surface irritation in the EyeFlow cohort. Many participants cited fewer ocular dryness complaints—often attributed to reduced reliance on topical medications.
- Low Revision Rates: Revision or second MIGS procedures remained below 5% in most trials, testifying to consistent stent patency over the year. Nonetheless, longer-term data are ongoing to ascertain how well the device endures over 3–5+ years.
Integrating with Cataract Surgery
Cataract extraction can lower IOP slightly by itself, freeing space in the anterior chamber and sometimes boosting aqueous outflow. Combining EyeFlow insertion with phacoemulsification thus became an appealing synergy. Observational cohorts found:
- Further IOP Declines: Patients who had both cataract removal and stent placement saw an incremental 2–3 mmHg dip beyond what was achieved by cataract surgery alone.
- High Rate of Medication Cessation: Many individuals discontinued one or more drops postoperatively, hinting at an enduring synergy in fluid dynamics.
- Time Efficiency: Surgeons found that adding the stent only marginally extended operative time, while patients avoided multiple separate procedures.
International Registry Data and Multi-Center Collaborations
Beyond single studies, large registry databases track real-world outcomes across diverse clinical settings and patient demographics. Such registries underscore:
- Safety Across Races and Anatomic Variations: The EyeFlow Stent performed well in patients of different ethnic backgrounds, many with prior ocular procedures (like prior LASIK or failed trabeculectomy).
- Stable IOP Out to Two Years: Data show that about 80–90% of eyes maintain target IOP under 18 mmHg without re-intervention at the two-year mark, consistent with or better than similarly placed MIGS devices.
- Learning Curve: Surgeons with MIGS experience quickly master EyeFlow insertion; novices, however, might require about 10–20 cases to reach plateau levels of efficiency and success.
Ongoing Investigations
While the EyeFlow Stent is already reaching clinics in some regions, further studies target:
- Head-to-Head Comparisons: Trials pitting EyeFlow directly against other MIGS devices (Hydrus, iStent) under standardized conditions.
- Expanded Indications: Investigating stent viability in angle-closure glaucoma after successful angle opening or in certain secondary glaucomas (e.g., pseudoexfoliation).
- Longer Horizons: Five-year outcome data to gauge whether stent performance wanes, stays stable, or improves over time with scar remodeling.
Collectively, these investigations paint a bright future for the EyeFlow Stent, buttressing it with validated evidence of efficacy, safety, and broad applicability. With continued trial expansions, clinicians and patients alike gain confidence that this next-generation device can reliably meet the evolving demands of glaucoma care.
Safety and Efficacy: Confidence in the EyeFlow Stent
Clinical Outcomes and IOP Stability
One of the central benchmarks for measuring the success of any glaucoma procedure is consistent, sustained IOP reduction. Real-world experiences with the EyeFlow Stent show:
- Sustained 20–30% Pressure Reduction: Regardless of baseline IOP, many see stable declines into low- to mid-teen ranges, aligning with typical MIGS outcomes. This level of control can significantly slow optic nerve damage over time.
- Medication Reduction: A large percentage of patients either reduce the number of prescribed drops or eliminate them altogether, which can enhance adherence and reduce the risk of ocular surface disease.
- Vision Preservation: Because EyeFlow effectively stabilizes IOP, patients face a reduced risk of progressive optic neuropathy. While it doesn’t cure underlying nerve damage, it can dramatically slow disease progression.
Intraoperative and Postoperative Risks
No surgery is free from hazards. Key potential complications related to EyeFlow:
- Micro-Perforations: Inadvertent damage to the trabecular meshwork or sclera during stent insertion, typically discovered and repaired intraoperatively.
- Transient Hypotony: Overly robust drainage can temporarily drop IOP below normal. Most cases resolve spontaneously as the eye adjusts.
- Inflammation: Low-grade anterior chamber inflammation or mild iritis can occur, responding well to topical steroids.
- Device Occlusion or Malposition: Fibrosis or migration might hamper fluid flow, though advanced designs lessen these risks. If detected, repositioning or partial revision can restore function.
Surgeon expertise, specialized training, and the device’s design refinements together mitigate these concerns. Clinical data show complication rates are typically low and rarely lead to severe vision-threatening outcomes.
Long-Term Reliability
Despite the EyeFlow Stent’s relative novelty, the track record of earlier MIGS devices suggests decades of stability for implants under the right conditions. Although scarring over the stent or inadvertent closure may occur in a subset of patients, periodic follow-ups let ophthalmologists detect rising IOP or partial stent occlusion early. Surgeons can occasionally alleviate blockages via in-office maneuvers or lasers, forestalling more drastic measures.
Combined with close IOP monitoring and routine optometric or ophthalmic evaluations, EyeFlow often fosters enduring ocular pressure control. Therefore, individuals benefit from a forward-looking approach that reduces the risk of future surgeries and fosters stable visual function over the long haul.
Patient Experience and Quality of Life
A hallmark advantage of MIGS-based stents is the relatively short recovery time and minimal lifestyle disruption compared to traditional filtering surgeries. With EyeFlow, many patients can resume normal activities within days. Because the procedure is typically done under local or topical anesthesia, the surgical burden is considerably less than older methods requiring full-thickness scleral flaps or external shunts.
Post-surgery, improved IOP regulation and reduced medication frequency can also enhance day-to-day comfort. Individuals often report fewer side effects such as ocular dryness, stinging from eye drops, or scheduling burdens. For older adults, who constitute a significant portion of glaucoma populations, these comfort gains help maintain independence and confidence in disease management.
Therapy Price: Evaluating the Cost of the EyeFlow Stent
Depending on the geographic region, healthcare setting, and insurance coverage, the EyeFlow Stent’s total costs can range widely. Hospitals or clinics may price it from a few thousand to over ten thousand dollars, factoring in device fees, surgeon expertise, and facility overhead. Some specialists offer bundled packages that include preoperative evaluation, the stent itself, and postoperative follow-up. Insurance plans vary in coverage; certain policies may reimburse the majority of the cost if EyeFlow is deemed medically necessary for moderate to advanced glaucoma. Alternative financing solutions, such as monthly installments, can help mitigate out-of-pocket expenses for those without comprehensive insurance.
Disclaimer: This article is intended for informational purposes only and does not replace professional medical advice, diagnosis, or treatment. Always consult with a qualified eye care specialist to determine whether the EyeFlow Stent is suitable for your individual needs.
If you found this information insightful, please consider sharing it with friends and family or on social media. Use our Facebook and X (formerly Twitter) share buttons—or any other platform you prefer—to help others discover how the EyeFlow Stent can transform glaucoma management.










