The eyes are our windows to the world, providing us with the essential ability to see and interpret our surroundings. They are complex sensory organs responsible not only for vision but also for regulating light, aiding balance, and even conveying emotional expressions. With intricate layers and numerous specialized structures, the eyes capture light and convert it into electrical signals that the brain interprets as images. This comprehensive guide explores the detailed anatomy and physiology of the eyes, discusses common disorders and conditions that may affect vision, reviews state-of-the-art diagnostic techniques and treatment options, and offers practical nutritional and lifestyle tips to maintain optimal ocular health.
Table of Contents
- Structural Overview & Composition
- Visual Dynamics & Physiology
- Common Eye Conditions
- Diagnostic Methods & Evaluations
- Treatment Interventions & Therapies
- Nutritional Strategies & Supplementation
- Lifestyle Tips for Ocular Health
- Trusted Resources & Further Reading
- Frequently Asked Questions
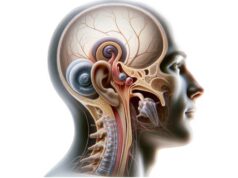
Structural Overview & Composition
The human eye is a sophisticated organ divided into two major components: the external structures and the internal structures. Each part contributes uniquely to the overall function of vision and protection.
External Structures
Eyelids (Palpebrae)
The eyelids are the first line of defense for the eyes. Composed of skin, muscle, and connective tissue, they protect the eyes from debris, bright light, and injury. The orbicularis oculi muscle controls blinking, which spreads tears across the eye’s surface and removes foreign particles. Additionally, the levator palpebrae superioris muscle raises the upper eyelid, enabling clear vision.
Eyelashes
Eyelashes act as physical barriers, preventing dust, sweat, and other foreign matter from entering the eye. They also trigger the blink reflex when something comes too close, adding an extra layer of protection.
Conjunctiva
This thin, transparent membrane covers the sclera (the white part of the eye) and lines the inner surface of the eyelids. It secretes mucus and tears, which lubricate the eye, reduce friction during blinking, and provide a protective barrier against infections.
Lacrimal Apparatus
The lacrimal apparatus consists of the lacrimal gland, lacrimal ducts, and lacrimal sac. The lacrimal gland produces tears that not only lubricate the eye but also contain enzymes and antibodies that help protect against infections. Tears drain through the lacrimal ducts into the nasal cavity, which is why your nose may run when you cry.
Internal Structures
Cornea
The cornea is the transparent, dome-shaped front part of the eye that covers the iris, pupil, and anterior chamber. It plays a crucial role in focusing light onto the retina, contributing up to 70% of the eye’s total focusing power. Its avascularity and high density of collagen fibers make it both strong and transparent.
Sclera
The sclera is the tough, white outer layer that provides structure and protection. It forms the eye’s supportive framework and is continuous with the cornea at the front, while at the back it meets the optic nerve.
Iris and Pupil
The iris is the colored part of the eye, composed of smooth muscle fibers that control the size of the pupil. The pupil is the central opening in the iris that regulates the amount of light entering the eye. In bright conditions, the iris constricts the pupil to limit light; in dim conditions, it dilates to allow more light in.
Lens
Located directly behind the iris, the lens is a transparent, flexible structure that further focuses light onto the retina. The ciliary muscles adjust the lens’s shape—a process known as accommodation—to ensure clear vision at various distances.
Ciliary Body
The ciliary body contains the ciliary muscles that control the lens’s shape during accommodation. It also produces aqueous humor, the fluid that fills the anterior chamber of the eye, providing nourishment and maintaining intraocular pressure.
Choroid
The choroid is a vascular layer situated between the sclera and retina. It supplies oxygen and nutrients to the outer layers of the retina and contains pigments that absorb excess light, preventing internal reflections that could degrade visual clarity.
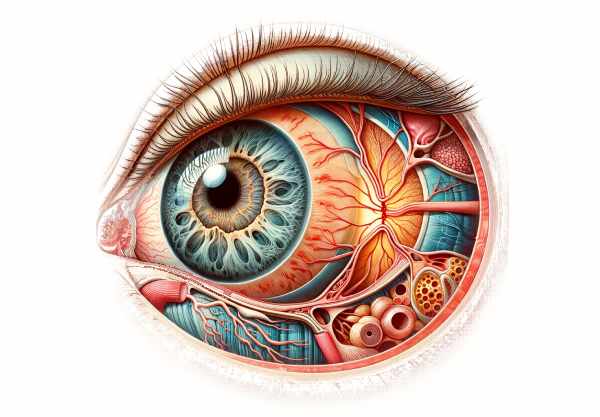
Retina
The retina is the light-sensitive inner layer of the eye that contains photoreceptor cells—rods and cones. Rods are responsible for vision in low light, while cones are crucial for color vision and visual acuity. The retina converts light into electrical signals through a process called phototransduction.
Macula and Fovea
The macula is a small, central area of the retina that is responsible for high-resolution vision. The fovea, located at the center of the macula, has a high density of cones and is critical for tasks requiring sharp vision, such as reading and driving.
Optic Nerve
The optic nerve transmits the electrical impulses generated by the retina to the brain’s visual cortex, where they are processed into images. It is composed of over a million nerve fibers and is essential for vision.
Vitreous Humor
Filling the space between the lens and retina, the vitreous humor is a clear, gel-like substance that helps maintain the eye’s shape and keeps the retina in place.
Visual Dynamics & Physiology
The physiology of the eye is a fascinating interplay of light, optics, and neural processing. From the moment light enters the eye until it is transformed into an image in the brain, a series of precise mechanisms ensures that we see clearly and accurately.
Light Entry and Refraction
- Corneal Refraction:
The journey of light begins at the cornea, which refracts (bends) incoming light rays toward the pupil. This initial refraction is critical as it accounts for a large part of the eye’s focusing power. - Pupil Regulation:
The iris adjusts the size of the pupil to control the amount of light entering the eye. In bright conditions, the pupil constricts to protect the retina; in low light, it dilates to allow more light in, enhancing vision. - Lens Accommodation:
Once light passes through the pupil, it is further focused by the lens. The ciliary muscles modify the shape of the lens—making it more convex for near vision and flatter for distant vision—ensuring that light is sharply focused on the retina.
Phototransduction
- Role of Photoreceptors:
In the retina, photoreceptor cells (rods and cones) convert light into electrical signals. Rods are highly sensitive to low light levels, while cones are responsible for color vision and fine detail. The distribution and density of these cells determine the quality of our visual perception. - Signal Conversion:
The process of phototransduction begins when light photons are absorbed by photopigments in the photoreceptors, triggering a cascade of chemical reactions. This cascade ultimately generates electrical impulses that are transmitted to the brain.
Neural Processing and Vision
- Bipolar and Ganglion Cells:
The electrical signals generated by photoreceptors are relayed to bipolar cells and then to ganglion cells within the retina. Ganglion cells integrate these signals and send them along the optic nerve to the brain. - Optic Nerve and Visual Cortex:
The optic nerve carries visual information to the brain’s visual cortex, where it is processed and interpreted as images. This complex integration allows us to perceive color, depth, movement, and form.
Coordination with Eye Movements
- Extraocular Muscles:
The eyes are controlled by six extraocular muscles that facilitate a wide range of movements. These muscles work together to maintain binocular vision, ensure precise focus, and track moving objects. - Fixation and Saccades:
Fixation allows the eyes to maintain focus on a single point, while saccadic movements enable rapid shifts in focus. These dynamic processes are critical for reading, driving, and navigating our environment.
Protective Mechanisms
- Tear Production and Blinking:
The lacrimal apparatus produces tears that lubricate the ocular surface, nourish the cornea, and protect against infections. Blinking spreads these tears evenly and helps clear debris from the eye. - Eyelids and Eyelashes:
Eyelids and eyelashes serve as physical barriers against foreign particles, reducing the risk of injury and infection. They also help regulate light exposure to the sensitive retina.
These physiological processes—spanning light entry, refraction, phototransduction, neural processing, and protective mechanisms—enable our eyes to deliver a seamless, dynamic visual experience while safeguarding the delicate structures of the visual system.
Common Eye Conditions
The eyes are susceptible to a range of conditions that can affect vision and overall ocular health. Early diagnosis and proper treatment are crucial to prevent permanent damage and preserve sight.
Refractive Errors
- Myopia (Nearsightedness):
Caused by an elongated eyeball or excessive curvature of the cornea, myopia results in blurred distant vision while near vision remains clear. Correction is typically achieved through glasses, contact lenses, or refractive surgery. - Hyperopia (Farsightedness):
Hyperopia occurs when the eyeball is too short or the cornea is too flat, causing difficulty focusing on near objects while distant vision may be relatively unaffected. Treatment options include corrective lenses and refractive surgery. - Astigmatism:
An irregular curvature of the cornea or lens leads to distorted or blurred vision at all distances. Corrective measures include specialized glasses, contact lenses, and surgical procedures. - Presbyopia:
An age-related loss of lens flexibility, presbyopia results in difficulty focusing on close objects. Reading glasses, bifocals, or multifocal lenses are common solutions.
Eye Diseases
- Cataracts:
A condition characterized by the clouding of the lens, cataracts lead to gradual vision loss, glare, and color distortion. Surgical removal of the cloudy lens followed by implantation of an intraocular lens is the most effective treatment. - Glaucoma:
A group of diseases that damage the optic nerve, often due to increased intraocular pressure, glaucoma can lead to irreversible vision loss. Early detection through regular eye exams and treatment with medications or surgery is essential to prevent progression. - Age-Related Macular Degeneration (AMD):
AMD affects the macula, leading to a loss of central vision. There are two types: dry (atrophic) and wet (neovascular). Treatments include nutritional supplements, anti-VEGF injections for wet AMD, and lifestyle modifications. - Diabetic Retinopathy:
A complication of diabetes, this condition damages the retinal blood vessels, leading to vision impairment. Control of blood sugar levels, laser therapy, and intravitreal injections are among the treatment options.
Inflammatory and Infectious Conditions
- Conjunctivitis (Pink Eye):
Inflammation of the conjunctiva caused by infections, allergies, or irritants. Symptoms include redness, itching, and discharge. Treatment varies based on the cause, including antibiotics for bacterial infections and antihistamines for allergies. - Uveitis:
Inflammation of the uveal tract, which includes the iris, ciliary body, and choroid, can lead to pain, light sensitivity, and blurred vision. Corticosteroids and immunosuppressants are often used to manage uveitis.
Retinal Disorders
- Retinal Detachment:
A medical emergency in which the retina separates from the underlying tissue, retinal detachment can lead to permanent vision loss if not promptly treated with surgery. - Tinnitus and Visual Disturbances:
While tinnitus is primarily an auditory condition, it can be associated with certain retinal or optic nerve disorders that affect overall ocular health.
These conditions underscore the importance of regular eye examinations and early intervention. Prompt diagnosis and treatment can prevent permanent damage and maintain optimal visual function.
Diagnostic Methods & Evaluations
Accurate diagnosis of eye disorders involves a variety of specialized tests and imaging techniques that help assess both structural and functional aspects of the visual system.
Comprehensive Eye Examination
- Visual Acuity Testing:
Using standardized eye charts, this test evaluates how clearly a person can see at various distances. It forms the basis of diagnosing refractive errors. - Refraction Assessment:
Conducted with a phoropter, this test determines the correct prescription for glasses or contact lenses to correct vision deficiencies. - Slit Lamp Examination:
A biomicroscope with a high-intensity light is used to examine the anterior structures of the eye in detail. This examination can reveal abnormalities in the cornea, iris, lens, and conjunctiva.
Intraocular Pressure Measurement
- Tonometry:
Tonometry assesses the pressure inside the eye, which is vital for diagnosing glaucoma. Non-contact (air puff) and applanation tonometry are common methods used in clinical practice.
Retinal Evaluation
- Ophthalmoscopy:
Using a handheld ophthalmoscope, clinicians can inspect the retina, optic nerve, and blood vessels for signs of diabetic retinopathy, macular degeneration, and other retinal conditions. - Fundus Photography:
High-resolution images of the retina are captured to monitor changes over time, providing a valuable tool for the diagnosis and management of retinal diseases. - Optical Coherence Tomography (OCT):
OCT produces detailed cross-sectional images of the retina, allowing for the precise evaluation of retinal layers. It is particularly useful for detecting macular edema, glaucoma, and other retinal abnormalities.
Visual Field Testing
- Perimetry:
This test assesses peripheral vision and detects areas of vision loss. It is critical for diagnosing glaucoma and neurological conditions that affect the visual pathway.
Specialized Diagnostic Procedures
- Fluorescein Angiography:
A fluorescent dye is injected into the bloodstream, and images of the retina are taken to evaluate blood flow and identify leaking vessels, which is particularly useful in diabetic retinopathy and macular degeneration. - Electroretinography (ERG):
ERG measures the electrical responses of various cell types in the retina, helping to diagnose retinal dystrophies and assess overall retinal function. - Visual Evoked Potentials (VEP):
VEP tests assess the electrical response of the brain to visual stimuli, aiding in the diagnosis of optic nerve and visual pathway disorders.
By combining these diagnostic techniques, healthcare professionals can accurately assess the structural and functional integrity of the eyes, leading to early detection of disorders and the formulation of targeted treatment plans.
Treatment Interventions & Therapeutic Options
Effective management of eye disorders requires a tailored approach that may involve medications, surgical interventions, and innovative therapies. The treatment strategy depends on the specific condition, its severity, and the individual’s overall ocular health.
Medical Treatments
- Pharmacotherapy:
- Antibiotic and Antiviral Drops: Used to treat bacterial and viral infections such as conjunctivitis and keratitis.
- Anti-Inflammatory Drops: Corticosteroid and NSAID eye drops help reduce inflammation in conditions like uveitis or post-surgical inflammation.
- Antiglaucoma Medications: Beta-blockers, prostaglandin analogs, and carbonic anhydrase inhibitors are used to lower intraocular pressure in glaucoma.
- Supplementation:
- Vitamins and Antioxidants: Supplements containing vitamins C, E, zinc, lutein, and zeaxanthin may slow the progression of age-related macular degeneration (AMD) and support overall retinal health.
Laser Treatments
- Laser Trabeculoplasty:
Used for open-angle glaucoma, this procedure improves fluid drainage from the eye, lowering intraocular pressure. - Laser Photocoagulation:
This technique is used to treat retinal tears, diabetic retinopathy, and macular edema by sealing leaking blood vessels and preventing retinal detachment. - Laser Iridotomy:
Performed in angle-closure glaucoma, it creates a small opening in the iris to improve the flow of aqueous humor and reduce intraocular pressure.
Surgical Interventions
- Cataract Surgery:
One of the most common surgical procedures, cataract surgery involves removing the cloudy natural lens and replacing it with a clear artificial intraocular lens (IOL). - Refractive Surgery:
Procedures like LASIK and PRK reshape the cornea to correct refractive errors, reducing dependency on corrective lenses. - Vitrectomy:
This surgical procedure removes the vitreous gel from the eye to treat conditions such as retinal detachment, macular holes, and vitreous hemorrhage. - Glaucoma Surgery:
Surgical options such as trabeculectomy and the insertion of drainage devices are used to create new pathways for aqueous humor, thereby reducing intraocular pressure. - Retinal Surgery:
Procedures like retinal reattachment surgery and endophotocoagulation help manage retinal detachments and prevent vision loss.
Innovative Therapies
- Intravitreous Injections:
Anti-VEGF medications, such as ranibizumab and aflibercept, are injected into the eye to treat wet AMD and diabetic macular edema by inhibiting abnormal blood vessel growth. - Stem Cell Therapy and Regenerative Medicine:
Experimental treatments aim to regenerate damaged retinal tissue using stem cells and tissue engineering techniques. - Retinal Prostheses:
Emerging technologies, like retinal implants, offer hope for restoring partial vision in patients with severe retinal degeneration.
Each treatment option is selected based on the specific diagnosis, severity of the condition, and individual patient needs. A multidisciplinary approach combining medical, surgical, and innovative therapies ensures optimal outcomes and improved quality of life.
Nutritional Strategies & Supplementation
Optimal eye health is closely linked to nutrition. A well-balanced diet, rich in essential vitamins, minerals, and antioxidants, can protect the eyes from oxidative stress, support visual function, and slow age-related degeneration.
Key Nutrients for Ocular Health
- Vitamin A:
Essential for maintaining healthy vision, vitamin A is crucial for the formation of retinal photoreceptors and overall eye function. Foods such as carrots, sweet potatoes, and leafy greens are rich in vitamin A. - Vitamin C:
A powerful antioxidant, vitamin C protects the eye from free radicals and supports the health of blood vessels in the retina. Citrus fruits, strawberries, and bell peppers are excellent sources. - Vitamin E:
Vitamin E works with other antioxidants to protect eye tissues from oxidative damage. It is found in nuts, seeds, and vegetable oils. - Zinc:
Zinc plays a pivotal role in transporting vitamin A from the liver to the retina and is vital for enzyme function in the eye. Oysters, beef, and legumes provide zinc. - Lutein and Zeaxanthin:
These carotenoids are concentrated in the macula and protect the eyes from harmful blue light and oxidative stress, reducing the risk of AMD.
Omega-3 Fatty Acids
- Anti-Inflammatory Properties:
Omega-3 fatty acids, found in fish oil and flaxseed, improve retinal health by reducing inflammation and supporting proper tear production, which can alleviate dry eye symptoms.
Herbal Supplements
- Bilberry Extract:
Rich in anthocyanins, bilberry extract may improve night vision and reduce eye fatigue. - Ginkgo Biloba:
Ginkgo biloba can enhance blood circulation to the eyes and has antioxidant properties that protect retinal cells.
Antioxidants and Enzymes
- N-Acetylcysteine (NAC):
NAC helps replenish glutathione, a critical antioxidant in the eye, reducing oxidative stress and protecting against damage. - Alpha-Lipoic Acid:
This antioxidant supports cellular energy production and may reduce the risk of cataracts and AMD.
Integrating these nutritional elements into your daily diet and considering targeted supplementation can significantly enhance eye health and preserve vision over time.
Lifestyle Tips for Ocular Health
In addition to medical treatment and proper nutrition, adopting healthy lifestyle habits is crucial for maintaining optimal eye health and preventing vision problems. The following practices can help protect your eyes and promote long-term ocular wellness.
Protection and Prevention
- Wear Sunglasses:
Protect your eyes from harmful ultraviolet (UV) rays by wearing sunglasses that offer 100% UV protection. This helps prevent cataracts and other UV-related eye damage. - Use Protective Eyewear:
In environments with high risk of eye injury—such as construction sites or during sports—wear appropriate safety goggles to prevent trauma.
Screen Time and Digital Eye Strain
- Regular Screen Breaks:
Follow the 20-20-20 rule: every 20 minutes, look at something 20 feet away for at least 20 seconds to reduce digital eye strain. - Optimize Your Workspace:
Ensure proper lighting and screen positioning to minimize glare and reduce strain on your eyes.
Physical Activity and Overall Health
- Exercise Regularly:
Regular physical activity improves blood circulation, which benefits the eyes by delivering oxygen and essential nutrients. Exercise also helps maintain a healthy weight, reducing the risk of conditions such as diabetes that can affect vision. - Stay Hydrated:
Proper hydration is essential for maintaining tear production and overall eye moisture, reducing the risk of dry eyes.
Healthy Habits
- Quit Smoking:
Smoking is associated with a higher risk of cataracts, AMD, and other eye diseases. Quitting smoking can significantly improve overall ocular health. - Limit Alcohol Consumption:
Excessive alcohol intake can negatively affect eye health and overall well-being. Moderation is key. - Manage Chronic Conditions:
Keep conditions like diabetes and hypertension under control through regular monitoring, as they can lead to serious eye complications if left unmanaged.
Regular Eye Examinations
- Routine Check-Ups:
Regular eye exams are critical for early detection of eye conditions. Comprehensive eye exams can identify refractive errors, glaucoma, retinal diseases, and other issues before they cause significant vision loss.
Implementing these lifestyle tips can help safeguard your vision, reduce the risk of eye disease, and ensure your eyes remain healthy throughout your life.
Trusted Resources & Further Reading
Staying informed about eye health is essential for both patients and healthcare providers. Below are some reliable resources that offer up-to-date research, detailed information, and practical guidance on maintaining ocular health.
Recommended Books
- “The Eye Care Revolution” by Robert Abel Jr.:
This book provides a comprehensive overview of eye care, offering insights into prevention, treatment, and lifestyle modifications for maintaining optimal vision. - “Eat Right for Your Sight” by Jennifer Trainer Thompson and Johanna M. Seddon:
A practical guide that combines nutritional advice with eye care tips, helping readers make informed dietary choices to support eye health. - “Macular Degeneration: The Complete Guide to Saving and Maximizing Your Sight” by Lylas G. Mogk and Marja Mogk:
Focuses on age-related macular degeneration and provides strategies for managing and preventing further vision loss.
Academic Journals
- Investigative Ophthalmology & Visual Science:
This peer-reviewed journal publishes cutting-edge research on various eye diseases, diagnostic techniques, and treatment innovations. - Ophthalmology:
The official journal of the American Academy of Ophthalmology, offering a wealth of research on clinical and surgical treatments for eye disorders.
Digital Tools and Mobile Apps
- EyeCare Live:
This app connects users with eye care professionals for virtual consultations, providing easy access to expert advice and guidance. - Eye Handbook:
A comprehensive reference tool for both patients and professionals, offering information on eye conditions, medications, and treatment procedures. - SightBook:
An app designed to help users track changes in their vision over time, providing data that can be shared with eye care providers to monitor ocular health.
These resources offer valuable insights and practical tools for maintaining and improving eye health, ensuring that you have the information needed to protect your vision.
Frequently Asked Questions About the Eyes
What are the primary functions of the eyes?
The eyes capture light, refract it through various structures, and convert it into electrical signals that are transmitted to the brain for image interpretation. They also play a critical role in balance by providing visual cues for spatial orientation.
How does the eye focus light onto the retina?
Light is focused onto the retina through the combined refraction provided by the cornea and the lens. The ciliary muscles adjust the lens shape—a process called accommodation—to focus light at various distances.
What causes common refractive errors?
Refractive errors such as myopia, hyperopia, astigmatism, and presbyopia result from abnormalities in the eye’s shape, corneal curvature, or lens flexibility. These errors disrupt the proper focusing of light on the retina, leading to blurred vision.
How is eye health evaluated?
Eye health is assessed through comprehensive eye exams that include visual acuity tests, refraction assessments, slit lamp examinations, tonometry, retinal imaging (OCT, fundus photography), and visual field testing.
What lifestyle changes can support eye health?
Maintaining a balanced diet, wearing UV-protective sunglasses, taking regular screen breaks, quitting smoking, managing chronic conditions, and scheduling regular eye exams are effective ways to support and preserve eye health.
Disclaimer:
The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a healthcare provider for personalized guidance.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about eye health and visual wellness.