Unraveling the Challenge of Diabetic Macular Edema
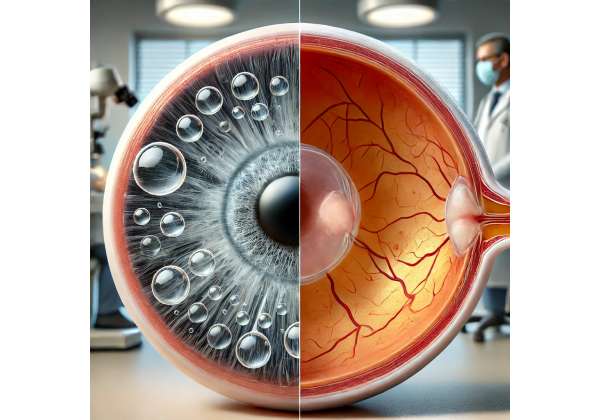
Diabetic macular edema (DME) is a vision-threatening complication that arises from diabetic retinopathy, one of the leading causes of blindness worldwide among working-age adults. People with diabetes frequently experience chronic hyperglycemia—elevated blood sugar levels—which, over time, can cause damage to the tiny blood vessels in the retina. The retina is the light-sensitive tissue at the back of the eye responsible for transforming visual input into signals transmitted to the brain. When these retinal capillaries are weakened or become leaky, the fluid accumulates in the macula, a specialized region of the retina that governs high-definition, central vision. This swelling in the macula impairs the eye’s ability to see fine details, thereby compromising essential tasks like reading, driving, and recognizing faces.
The prevalence of DME is growing globally due to the rising incidence of diabetes in diverse populations. As more individuals receive a diagnosis of Type 1 or Type 2 diabetes, the risk of developing diabetic retinopathy (and subsequently DME) increases over time. Research suggests that controlling blood sugar, blood pressure, and lipid levels can reduce the risk of retinopathy progression, yet many patients still suffer from some degree of retinal damage. Early detection through routine eye screenings remains crucial, but even with timely diagnosis, the macula can become edematous, resulting in blurred vision or dark spots in the central field.
Historically, treatment for DME involved laser photocoagulation. While laser therapy helps cauterize leaking blood vessels and slow disease progression, it does not always significantly improve lost vision. Intravitreal corticosteroids entered the treatment paradigm to mitigate inflammation within the retina, achieving moderate success in certain patients. Still, these therapies sometimes come with side effects such as elevated intraocular pressure and potential cataract formation. Moreover, not all patients respond uniformly to corticosteroids or laser, spurring clinicians and researchers to explore new pathways for targeted management.
A major breakthrough came with the recognition of vascular endothelial growth factor (VEGF) as a key mediator in the development and progression of diabetic retinopathy and macular edema. VEGF is a protein that promotes new blood vessel formation and increases vascular permeability. In diabetic eyes, overproduction of VEGF can cause retinal blood vessels to leak fluid or proliferate abnormally, leading to macular edema or neovascular complications. Targeting VEGF specifically has thus become a cornerstone of modern treatment for diabetic macular edema.
Eylea (aflibercept) emerged as a potent anti-VEGF therapy with distinct structural features that allow it to bind VEGF-A, VEGF-B, and placental growth factor (PlGF). By inhibiting these molecules, Eylea reduces vascular leakage and swelling in the retina. This approach represents a more refined strategy compared to conventional laser or broad-spectrum anti-inflammatory agents. Through multiple clinical studies and real-world usage, Eylea has repeatedly demonstrated its capacity to preserve and sometimes restore central vision in patients with DME.
Despite its proven track record, administering Eylea is not a standalone solution. Comprehensive diabetes management and routine monitoring for retinopathy are still critical. Patients and healthcare providers must adopt a holistic perspective that includes glycemic control, blood pressure management, and timely ophthalmic evaluations. The integration of these measures bolsters the effects of anti-VEGF therapy, helping sustain retinal health over the long term.
In the sections that follow, we delve into how Eylea specifically combats DME at the molecular level, the recommended protocols for its administration, the latest clinical evidence surrounding its safety and efficacy, and practical considerations related to cost. We also look at how Eylea is positioned in comparison to other treatments that target similar pathways. Through detailed exploration, patients and practitioners alike can gain insights into the practical and scientific basis for using Eylea, which has become one of the leading solutions for diabetic macular edema in modern ophthalmic practice.
How Eylea Works to Reduce DME and Protect Vision
Intravitreal anti-VEGF medications have revolutionized the therapeutic landscape of diabetic macular edema, and Eylea ranks prominently among them. Understanding how Eylea combats the pathophysiological underpinnings of DME begins with recognizing the pivotal role of VEGF and related growth factors in vascular leakage and retinal damage.
The Role of VEGF in DME
VEGF, or vascular endothelial growth factor, increases vessel permeability and stimulates the formation of new blood vessels, a process known as neovascularization. In eyes with diabetic retinopathy, chronic hyperglycemia triggers an elevated production of VEGF. Excess VEGF weakens the blood-retinal barrier, leading to leakage of fluid and proteins into the macular region. This accumulation of fluid thickens the macula, thereby distorting the delicate architecture responsible for fine, color-detailed vision.
Because DME directly impairs the macula, even moderate swelling can translate into noticeable vision loss. Traditional treatments such as laser therapy aim to seal off leaking vessels, but these approaches may not address the underlying pathological stimulus—namely VEGF. Here, anti-VEGF therapies step in, blocking the key molecules driving leakage and abnormal vessel growth.
What Sets Eylea Apart
Eylea (aflibercept) differentiates itself by its specific binding mechanism. It is composed of portions of the VEGF receptors (VEGFR-1 and VEGFR-2) fused to an immunoglobulin component, creating a soluble decoy receptor. This receptor traps not only VEGF-A but also VEGF-B and PlGF (placental growth factor). PlGF itself can amplify the effects of VEGF-A, contributing to pathologic angiogenesis and increased vascular permeability.
By sequestering these growth factors, Eylea prevents them from binding to their natural receptors on the endothelial cells of retinal vessels. This action curtails the cascade of events that leads to increased capillary permeability and macular swelling. The result is a more robust blockade of the VEGF family’s pathological effects, offering both a reduction in current edema and a preventive measure against further deterioration.
Dual Benefit: Reducing Edema and Slowing Disease Progression
Beyond acute reduction in macular swelling, Eylea also helps mitigate the ongoing cycle of VEGF-driven retinal damage. By lowering the availability of VEGF in the microenvironment of the retina, Eylea impedes the formation of new fragile vessels that can bleed or leak. Hence, patients often see benefits not only in stabilized or improved vision, but also in decreased severity of diabetic retinopathy. While each patient’s response may vary, many individuals experience fewer disease flare-ups and improved retinal anatomy as observed through imaging modalities like optical coherence tomography (OCT).
Direct Impact on Visual Acuity
Given that DME primarily compromises the central vision needed for reading, driving, and detailed tasks, any therapy aiming to improve vision must target swelling in the macula. Clinical studies show that, in many cases, patients receiving Eylea injections gain letters on a standard visual acuity chart, reflecting a tangible improvement in their ability to see fine detail. Although not every patient regains perfect 20/20 vision, even moderate improvements can be life-changing—enabling greater independence and quality of life.
Complementary Role with Systemic Management
Despite its targeted approach, Eylea does not address all aspects of diabetic retinopathy. Optimal glycemic, lipid, and blood pressure control remain fundamental to slowing the progression of microvascular complications. When used in conjunction with good metabolic control, Eylea yields the most durable benefits. Many ophthalmologists work closely with primary care physicians or endocrinologists, forming an integrated care team to address both the ocular and systemic facets of diabetes.
Eylea Compared to Alternative Anti-VEGF Agents
While other anti-VEGF medications, such as ranibizumab (Lucentis) and bevacizumab (Avastin), also show efficacy in DME, Eylea’s unique binding structure and extended durability in the eye can translate to specific advantages. Some patients may require fewer injections or experience more substantial improvements in certain functional vision measures. However, choices between anti-VEGF agents often hinge on factors such as treatment protocols, cost, and patient-specific responses. Ophthalmologists frequently tailor therapy to suit an individual’s disease state, lifestyle, and access to medical care.
Long-Term Outlook
Because diabetes is typically a lifelong condition, the potential for DME to recur remains. Eylea’s role in modern treatment is significant because it offers a way to continually suppress the destructive processes triggered by VEGF, enabling many patients to preserve functional vision. With ongoing follow-up and regular injections when necessary, patients often experience a stable or improved visual trajectory. Paired with vigilant oversight for diabetic control, this approach underscores how Eylea strategically addresses both immediate and long-term complications of DME.
In essence, Eylea’s mechanism of action is elegantly simple yet powerfully effective—deactivating the molecular drivers of macular swelling to protect and enhance vision. Armed with a clear picture of how this medication works, patients and care providers can approach diabetic macular edema with greater confidence, knowing that modern science offers an advanced treatment option specifically designed to intercept the core pathological events driving vision loss.
Step-by-Step Guidelines for Administering Eylea
Eylea’s proven efficacy in treating diabetic macular edema largely depends on a carefully structured administration schedule. While the idea of receiving an injection directly into the eye can be intimidating for some patients, proper technique, infection control measures, and follow-up protocols are designed to ensure a safe and effective experience. Below is an in-depth look at how Eylea is administered and the steps patients can expect.
Pre-Treatment Evaluation and Patient Preparation
- Confirming Indication: Before initiating treatment, an ophthalmologist conducts detailed examinations including fluorescein angiography, fundus photography, and OCT imaging. These tests confirm that macular edema is present and that anti-VEGF therapy is suitable.
- Review of Medical History: A comprehensive review of the patient’s systemic health and ocular history ensures there are no major contraindications, such as active ocular infections.
- Informed Consent: The physician explains potential benefits, risks, and alternatives. Patients are encouraged to ask questions, fostering a collaborative environment where they feel involved in decision-making.
The Injection Procedure
- Anesthetic Application: To minimize discomfort, local anesthesia in the form of eye drops or a mild anesthetic gel is administered. Some clinics may use a combination of methods to ensure optimal comfort.
- Antiseptic Protocol: The ocular surface is thoroughly cleaned with an antiseptic solution like povidone-iodine to reduce infection risk. The eyelids and surrounding skin are also disinfected.
- Sterile Environment: The injection is typically performed in a clean procedure room or minor operating theater under strict aseptic conditions. Surgeons or retina specialists use gloves, masks, and sometimes sterile drapes around the eye.
- Speculum Placement: A small eyelid speculum keeps the eye open, allowing the specialist unobstructed access to the injection site while preventing accidental blinking.
- Injection Technique: A fine-gauge needle is used to deliver Eylea (aflibercept) into the vitreous cavity—the gel-like substance filling the eye. The physician typically injects the drug through the pars plana, located about 3.5 to 4 millimeters behind the corneal limbus, ensuring that the medication reaches the retina effectively.
- Post-Injection Antibiotics: Some clinics apply antibiotic eye drops after the procedure to further reduce infection risk. Although clinical guidelines vary, this step remains common in many practices.
Patient Experience and Immediate Aftercare
- Mild Discomfort: Patients may notice slight pressure during the injection, but pain is usually minimal due to local anesthesia. After the procedure, mild irritation or a foreign-body sensation is possible.
- Visual Check: Right after the injection, vision might be somewhat blurry, and a few patients see temporary floaters or bubbles—often small pockets of air introduced during the procedure. These typically resolve within a day or two.
- Steroid Drops: Ophthalmologists may prescribe short-term steroid drops or additional medication to reduce inflammation. The patient receives instructions on how often to apply these drops and for how many days.
Follow-Up Appointment Schedules
- Immediate Post-Injection Review: A follow-up visit is usually scheduled within one to two weeks to assess any signs of infection, elevated intraocular pressure, or other complications.
- Ongoing Appointments: Eylea is often given on a fixed regimen—once a month or once every two months for a certain induction period—followed by a treat-and-extend or as-needed schedule. The exact protocol can vary depending on the patient’s response and severity of edema.
- OCT Imaging and Visual Acuity Testing: Ongoing imaging via OCT helps quantify changes in macular thickness, while standard visual acuity tests track improvements or stability in vision.
Treatment Duration and Customization
DME management necessitates an individualized plan:
- Loading Phase: Some regimens suggest monthly injections for the first five or six months. This loading phase helps achieve maximum control over the edema.
- Maintenance Phase: Once edema is under control, injection frequency may be tapered—either monthly, bimonthly, or even longer intervals if the macula remains stable without fluid accumulation.
- Re-Evaluation: Some patients can go longer between injections, while others require more frequent treatments. Specialists can decide on an “as-needed” (PRN) approach or a “treat-and-extend” protocol in which intervals between injections lengthen steadily, provided the retina shows no signs of recurrent swelling.
Potential Side Effects and How They Are Managed
- Infection: One of the most feared complications is endophthalmitis (intraocular infection), though it remains rare when sterile procedures are followed. Symptoms like increasing eye pain, severe redness, or abrupt worsening of vision after injection warrant immediate medical attention.
- Elevated Intraocular Pressure: A temporary spike in eye pressure may occur post-injection, but routine checks and medications can typically manage this if it arises.
- Retinal Detachment: Extremely rare, but individuals should be aware of sudden increases in floaters, flashes of light, or a shadowy curtain in their vision—signs that call for urgent evaluation.
Communicating and Coordinating Care
Successful administration of Eylea for DME benefits from integrated care between the ophthalmologist, primary care physician, or endocrinologist. Since tight control of blood sugar levels can amplify the positive outcomes of intravitreal injections, consistent dialogue ensures that patients manage their diabetes effectively while receiving ocular treatments. Some specialists also recommend lifestyle adjustments—such as balanced diets, regular exercise, and smoking cessation—to further stabilize the patient’s metabolic and vascular status.
In summary, the intravitreal injection process with Eylea is a well-established, patient-friendly procedure. With meticulous adherence to a structured treatment schedule and vigilant follow-up, many individuals with DME can maintain or improve their visual function, reducing the risk of severe vision loss. Through these protocols, Eylea proves to be a cornerstone in the quest for effective DME management.
Current Research and Evidence
Eylea’s role in the management of diabetic macular edema is supported by robust clinical evidence and ongoing research. Multiple large-scale trials and real-world studies consistently highlight Eylea’s ability to reduce macular swelling, preserve retinal integrity, and improve visual acuity in a significant proportion of patients. Below, we examine some pivotal studies and emerging investigations that underscore the medication’s value for individuals grappling with DME.
Landmark Clinical Trials
- VIVID-DME and VISTA-DME
These two phase III clinical trials paved the way for Eylea’s regulatory approval for DME. Patients treated with Eylea injections exhibited significant improvements in best-corrected visual acuity (BCVA) compared to those receiving laser photocoagulation alone. By the conclusion of the one-year primary endpoint period, the average BCVA gain in the Eylea arms outpaced that in the laser control groups.
Importantly, the safety profile was consistent across both studies. Reported side effects were largely manageable, and severe adverse events—such as endophthalmitis—remained quite rare. The majority of subjects continued to derive benefits through extended follow-up periods, supporting the notion that consistent anti-VEGF therapy can help sustain visual gains. - DRCR.net Protocol T
The Diabetic Retinopathy Clinical Research Network (DRCR.net) conducted Protocol T, a head-to-head comparison of Eylea, ranibizumab, and bevacizumab for DME. Overall, Eylea demonstrated a distinct advantage in patients with more severe baseline vision loss (20/50 or worse). Over a year, these individuals achieved greater improvements in BCVA when compared with the other two anti-VEGF drugs.
While Eylea, ranibizumab, and bevacizumab all produced meaningful gains in many patients, the data suggested that Eylea might be particularly beneficial when starting from lower levels of visual acuity. Such findings guide clinicians in personalizing treatment choices based on disease severity.
Real-World Evidence and Long-Term Outcomes
Clinical trials offer controlled environments, but real-world studies further validate whether such results translate into everyday practice. Registries and observational studies in various countries have shown:
- Sustained Vision Improvement: Even beyond the initial loading phase, patients who maintain follow-up schedules and receive injections as needed often retain better central vision.
- Reduced Need for Rescue Therapy: Once the macular edema is under control, the intervals between Eylea injections can sometimes be extended, and fewer additional treatments (like laser or corticosteroids) are necessary.
- Improved Retinopathy Grading: Some patients also demonstrate an improvement in the severity of their overall diabetic retinopathy, indicating that controlling macular edema with Eylea might carry broader benefits for retinal health.
Eylea in Combination Therapies
Ongoing research explores whether combining Eylea with other agents can further optimize outcomes:
- Steroid Adjuncts: Some physicians add intravitreal steroids (such as dexamethasone implants) to the regimen in cases where persistent inflammation persists or where frequent anti-VEGF injections alone are insufficient. Early findings suggest that certain patients may gain better or faster control of DME when these therapies are combined, although the risk of elevated intraocular pressure must be carefully monitored.
- Laser Therapy: While Eylea often replaces or reduces the need for laser photocoagulation, small focal lasers are sometimes used alongside anti-VEGF injections for patients who have areas of focal leakage. The synergy can be beneficial, but the standard approach has increasingly shifted toward intravitreal injections alone.
Beyond Macular Edema: Impact on Diabetic Retinopathy
One fascinating area of research involves exploring Eylea’s effect on the progression of diabetic retinopathy itself, even aside from macular edema. Several studies, including DRCR.net trials, have documented that anti-VEGF therapy can delay or reverse some manifestations of proliferative diabetic retinopathy, potentially decreasing the likelihood of severe complications like vitreous hemorrhage or tractional retinal detachment. Although these findings are encouraging, more research is needed to define the ideal injection frequency and to determine which subsets of patients gain the most prophylactic benefit.
Future Directions
As anti-VEGF therapy for DME matures, emerging data are focusing on:
- Durable Formulations: Longer-lasting forms of aflibercept or extended-release implants might reduce the frequency of intravitreal injections. Clinical trials are underway to test safety and efficacy of such innovations, promising a more convenient treatment experience.
- Biomarkers and Personalized Medicine: Researchers are investigating biomarkers—such as specific cytokine profiles or genetic markers—that predict an individual’s response to Eylea. By identifying these biomarkers, clinicians could tailor regimens more precisely, potentially improving efficiency and outcomes.
- Combination with Systemic Diabetes Control: Growing evidence supports the notion that tight glycemic management amplifies the beneficial effects of intravitreal therapy. Studies are increasingly examining how improved insulin therapy, lifestyle changes, and anti-VEGF injections collectively influence the course of DME.
Overall, extensive clinical evidence confirms Eylea’s pivotal role in minimizing DME-induced visual impairment. With numerous research efforts continuing, Eylea’s utility may expand to include improved regimens, combination strategies, and prophylactic benefits for patients at risk of diabetic retinal complications. This evolving knowledge base furnishes ophthalmologists and patients alike with an increasingly refined toolkit for safeguarding vision in the face of diabetes.
Evaluating Success Rates and Ensuring Patient Safety
While Eylea has established itself as a cornerstone therapy for diabetic macular edema, patients often seek reliable data about both its effectiveness and potential risks. Understanding how Eylea’s success rates align with safety considerations is crucial for informed decision-making. This section breaks down the nature of visual improvement with Eylea, possible side effects, and the measures that healthcare providers adopt to minimize complications.
Quantifying Visual Gains
Diabetic macular edema often presents with blurred central vision, making tasks like reading or driving difficult. Eylea’s main clinical endpoint is improving best-corrected visual acuity (BCVA), typically measured in letters gained on a standardized vision chart. Across pivotal trials:
- Vision Improvement: A significant portion of patients can gain 10 to 15 letters in BCVA over the first year of treatment if they adhere to the recommended injection schedule. Although results vary, many individuals report practical improvements in daily life—being able to read smaller print or drive more confidently under certain lighting conditions.
- Long-Term Benefits: Continued injections are commonly needed to maintain these gains. Patients who keep to a regular follow-up and treat-and-extend approach often preserve or further enhance their vision over multiple years.
Reduction in Macular Swelling
OCT (optical coherence tomography) is used to measure the thickness of the macula, serving as a reliable indicator of how effectively Eylea is reducing fluid and inflammation. Most patients experience a notable decrease in macular thickness within a few months:
- Correlation with Visual Acuity: Generally, a reduction in retinal thickness corresponds with improved or stabilized central vision. In cases where thickness remains high despite treatment, the physician may investigate underlying factors such as suboptimal glycemic control or concurrent ocular conditions.
- Morphological Improvements: In many instances, OCT scans reveal structural restoration of the macula as fluid pockets dissipate. This morphological recovery is one reason Eylea is often chosen for DME—it addresses the root cause of leakage at the vascular level.
Managing Potential Risks and Side Effects
Although Eylea is well-tolerated in most patients, certain risks accompany any intravitreal injection:
- Infection (Endophthalmitis): Occurring in a small fraction of patients, infection inside the eye can lead to severe complications if untreated. Strict aseptic techniques and post-injection follow-up significantly lower this risk.
- Inflammation: Some individuals experience mild intraocular inflammation or soreness, often manageable with topical anti-inflammatory drops.
- Retinal Detachment: Rare but possible, it necessitates immediate medical intervention if symptoms—like sudden visual flashes or a dark curtain—arise.
- Vascular Events: There is debate about the systemic risks of anti-VEGF therapy, especially in patients with a history of stroke or cardiovascular events. While large-scale data do not consistently show a higher incidence of such events, caution and close communication with the patient’s medical team are prudent.
Safety Protocols and Monitoring
To maintain a strong safety profile, ophthalmologists follow clear guidelines:
- Rigorous Sterile Technique: Each injection is performed under sterile conditions, using povidone-iodine to disinfect the ocular surface and single-use, sterile instruments.
- Post-Injection Observation: Patients often remain in the clinic briefly after the injection for initial monitoring. If any complications arise in the hours or days following, immediate evaluation is advised.
- Ongoing Assessment of Retinal Status: OCT imaging, fundus examinations, and visual acuity tests help the specialist track progress and spot any anomalies that might require a change in strategy.
- Collaboration with Internists or Endocrinologists: Since many individuals with DME have comorbidities like hypertension, kidney disease, and cardiovascular concerns, multi-disciplinary collaboration ensures balanced management of both ocular and systemic health.
Patient Factors Influencing Outcome
- Adherence to Treatment Schedule: Missing scheduled injections or follow-up appointments can limit the ability of Eylea to control DME effectively.
- Glycemic Control: High blood sugar exacerbates microvascular damage. Patients with stable or improved hemoglobin A1c levels often have better responses to anti-VEGF therapies.
- Disease Duration and Severity: Long-standing, severe macular edema or advanced diabetic retinopathy might require additional treatments or more frequent injections.
- Other Ocular Pathologies: Conditions like epiretinal membranes or cataracts can influence visual outcomes. In some cases, surgery to address these issues can complement Eylea’s beneficial effects.
Positive Bias on Confirmed Benefits
Numerous real-world reports and controlled studies highlight Eylea’s consistent success in mitigating vision loss from DME. Many patients who once feared permanent visual disability have preserved or regained clarity—providing a renewed sense of independence. By continuously blocking VEGF and improving macular thickness, Eylea offers an evidence-based route to halting or reversing one of the most devastating complications of diabetic retinopathy.
Collectively, these insights paint a picture of Eylea as both powerful and relatively safe for the treatment of DME. Ophthalmologists remain vigilant about potential complications, but the therapy’s overall risk-benefit profile remains strongly favorable for eligible patients. When combined with diligent diabetes management, Eylea stands as a robust tool to reduce swelling, maintain retinal function, and foster better visual outcomes in the face of diabetic macular edema.
Exploring the Costs and Coverage for Eylea
Eylea injections can range from about \$1,800 to \$2,500 per dose, depending on factors such as insurance agreements, pharmacy markups, and regional variations. Many insurance plans, including private carriers and government programs, cover part or all of the drug cost when prescribed for diabetic macular edema. Some manufacturers and foundations also offer patient-assistance programs or co-pay discounts. Checking with your ophthalmologist’s billing department and exploring manufacturer coupons can help reduce out-of-pocket expenses for eligible patients.
Disclaimer:
This article is for informational purposes only and does not replace personalized medical advice. Always consult a qualified healthcare professional for any questions or concerns regarding your eye health, treatment, or medications.
We hope you found this information valuable. Feel free to share this article with friends, family, or on your social media channels—whether Facebook, X (formerly Twitter), or elsewhere—to help raise awareness about Eylea’s vital role in combating diabetic macular edema. Your support can make a meaningful difference for others seeking clearer vision and better outcomes!