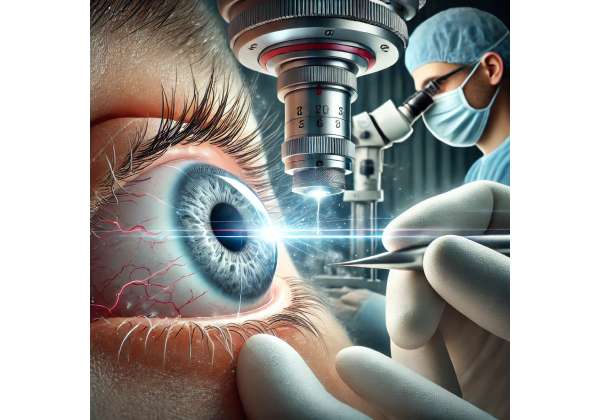
Redefining Vision Restoration: A Fresh Look at Femtosecond Laser Cataract Procedures (Introduction)
Cataracts remain a leading cause of reversible vision loss, affecting millions of people worldwide. They occur when the crystalline lens in the eye becomes clouded, often due to age-related changes, but also arising from factors like trauma, metabolic disorders, or certain medications. Traditionally, the gold standard for cataract removal has been phacoemulsification, where a surgeon uses ultrasound energy to break up and extract the cloudy lens. While this approach drastically improved outcomes compared to older methods, it still relies on manual incisions and circular capsulotomies—steps that can introduce variability based on surgeon expertise and patient eye anatomy.
Femtosecond laser-assisted cataract surgery (FLACS) modernizes these steps by harnessing ultrafast laser pulses to automate and perfect parts of the procedure. Lauded for its precision in creating corneal incisions, anterior capsulotomies, and initial lens fragmentation, FLACS can reduce the margin of human error, enhance predictability, and potentially expedite recovery. Patients frequently appreciate that this advanced technology may lower their dependence on glasses postoperatively, while surgeons find more consistent results and improved workflow.
Yet, the question persists: Are femtosecond lasers truly transformative for every cataract patient? Although the approach has garnered enthusiastic endorsements from many ophthalmologists, cost and accessibility can limit its universal adoption. Furthermore, not all surgeons or centers offer FLACS, and some debate remains about its incremental benefits in straightforward cataract cases. Below, we explore the underpinnings of femtosecond laser technology, how it integrates into modern cataract workflows, supportive research findings, safety considerations, and financial dimensions so patients and practitioners can make informed decisions about whether femtosecond laser-assisted cataract surgery is the right path to clearer vision.
Examining the Technology: Insights into Femtosecond Laser-Assisted Cataract Surgery (Therapy Overview and Insights)
The Evolution of Laser in Cataract Procedures
Laser systems are not entirely new to ophthalmology. Excimer lasers revolutionized corneal refractive surgery, while Nd:YAG lasers have long been employed for posterior capsulotomy post-cataract. However, the development of femtosecond lasers—which emit ultrashort bursts of energy measured in quadrillionths (10^-15) of a second—opened additional possibilities. At such high speeds, laser energy can incise tissue with remarkable accuracy and minimal collateral damage.
For cataract removal, femtosecond lasers accomplish the following critical tasks:
- Corneal Incisions: The laser can create self-sealing corneal cuts at precise depths and angles, improving reproducibility and reducing induced astigmatism.
- Anterior Capsulotomy: A circular opening in the lens capsule is formed, bypassing the need for a manual capsulorhexis. Laser pulses define this perfect circle, which can optimize lens positioning for advanced intraocular lens (IOL) implants.
- Lens Fragmentation: Femtosecond pulses segment or soften the lens nucleus, reducing the phaco energy required. This step can be especially beneficial in dense cataracts, diminishing ultrasound time and potential corneal endothelial damage.
Tailoring Each Step to Patient Needs
FLACS offers surgeons the ability to customize incision parameters, from the shape and location of limbal or main incisions to the exact diameter of the capsulotomy. For patients with preexisting astigmatism, the laser can perform precise arcuate keratotomies to fine-tune corneal curvature. Additionally, by fragmenting the lens nucleus into patterns (like pie-shaped wedges or grid-like segments), the surgeon can remove lens material more gently, often accelerating the procedure while preserving corneal clarity.
Potential Benefits Over Conventional Methods
Proponents of FLACS highlight several advantages:
- Consistency in Capsulotomy: Achieving a perfect rhexis every time fosters more stable lens positioning, which can enhance refractive outcomes for premium IOLs (like toric or multifocal lenses).
- Reduced Phaco Time: By “pre-chopping” the lens with laser pulses, overall phaco energy usage drops, potentially lowering the risk of corneal edema or endothelial cell loss, leading to faster visual recovery.
- Better Wound Architecture: Laser-created incisions can align more precisely along corneal planes, potentially improving wound integrity and minimizing surgically induced astigmatism.
- Enhanced Safety: Minimizing mechanical manipulations inside the eye theoretically lowers the chance of complications such as capsule tears or lens-iris diaphragm instability.
However, critics point out that skilled manual surgeons can achieve near-flawless results without laser assistance, and not every patient sees a dramatic difference in final visual acuity or complication rates. Additionally, cost and availability may be an obstacle for some seeking FLACS.
Considerations for Optimal Outcomes
While FLACS can refine multiple aspects of the cataract procedure, it does not eliminate every risk. Success still depends on:
- Surgeon Expertise: Operating the femtosecond laser interface and seamlessly transitioning to phacoemulsification require a learning curve.
- Patient Anatomy: Patients with corneal scarring, small palpebral fissures, or advanced posterior subcapsular opacities may be less suitable.
- Co-Existing Conditions: Coexisting ocular pathologies, such as advanced glaucoma or retinal diseases, could overshadow the advantages of FLACS.
In short, femtosecond laser-assisted cataract surgery extends the precision and predictability of standard cataract approaches. Next, we delve into how surgeons incorporate FLACS in the operating room, analyzing the procedural flow from preoperative steps to postoperative advice.
Applying Femtosecond Technology: Protocols and Best Practices (Application and Treatment Protocols)
Preoperative Assessments and Planning
Before scheduling FLACS, ophthalmologists conduct thorough preoperative evaluations:
- Corneal and Lens Examination: Corneal topography or tomography helps identify astigmatism that can be corrected via femtosecond incisions. Additionally, the lens’s nuclear density is assessed so surgeons can tailor fragmentation patterns.
- Biometry and IOL Calculations: Precise axial length, keratometry, and anterior chamber depth measurements guide lens power selection, especially vital for advanced IOLs. The uniform capsulotomy from FLACS helps ensure consistent effective lens position (ELP).
- Ocular Surface Optimization: Significant dry eye or ocular surface irregularities can hamper laser docking and incisional accuracy. Surgeons typically treat dryness or blepharitis preemptively.
Step-by-Step Femtosecond Procedure
In many centers, the FLACS steps precede standard phacoemulsification:
- Docking: The patient’s eye is aligned with the femtosecond laser unit. Gentle suction or a soft docking mechanism stabilizes the globe, ensuring minimal movement.
- OCT or Imaging Guidance: Integrated systems map the cornea and lens in real time, guiding laser cuts for corneal incisions, capsulotomy, and lens fragmentation.
- Laser Delivery: In seconds, a series of pulses form precise corneal incisions, create a near-perfect circular capsulotomy, and fragment the lens nucleus. The patient sees or hears minimal cues—many describe an audible clicking from the laser or experience mild pressure.
- Transition to Phaco: After the laser portion, the surgeon typically moves the patient to a standard operating microscope. Tiny incisions (often created or partially formed by the laser) are opened, and phacoemulsification begins. However, fragmentation from the laser significantly reduces the ultrasound energy needed.
- IOL Placement: The chosen IOL (monofocal, toric, multifocal, or extended depth of focus) is inserted into the capsular bag. The precisely shaped capsular opening can optimize IOL positioning and rotational stability, particularly for toric designs.
Immediate Postoperative Management
Eye Shielding: A protective cover prevents accidental rubbing or minor trauma. Patients generally start antibiotic and anti-inflammatory drops to avert infection or excessive inflammation.
Activity Restrictions: These typically resemble those for standard cataract surgery—no heavy lifting or forceful eye rubbing for the initial days. Short walks and mild daily activities are permissible soon after.
Follow-Up Schedules: Usually day 1 or day 2 post-op, then about a week later, and again at a month. Surgeons track corneal clarity, lens stability, and early visual acuity to confirm no emergent complications.
Potential Complications or Challenges
While FLACS is widely heralded, no procedure is foolproof:
- Suction Break: If the eye moves or docking loosens, incomplete or misaligned incisions can occur. Surgeons may revert to manual steps if the laser portion is disrupted.
- Corneal Edema: Although phaco energy is often reduced, corneal edema can still arise from fluid usage or mild endothelial stress. However, one advantage of FLACS is typically less ultrasound stress.
- Capsule-Related Issues: A mismatch between laser patterns and lens anatomy can occasionally lead to incomplete capsulotomy tags or micro-rips, though rates are low with modern systems.
Integrating FLACS with Advanced IOL Strategies
Femtosecond lasers unify elegantly with premium lens implants. Toric IOLs demand accurate alignment and minimal rotation, benefits reinforced by a perfect capsulotomy and consistent effective lens position from FLACS. Meanwhile, multifocal or extended depth-of-focus IOLs also benefit from the lens centration possible through uniform capsular openings. As a result, FLACS can offer synergy for patients seeking the best chance at spectacle independence.
The next section details the evidence behind these protocols, highlighting how both major clinical trials and real-world experiences support claims of improved outcomes and safe usage.
Backing it Up: Clinical Data and Developments in FLACS (Latest Research and Studies)
Landmark Trials and Comparative Research
Multiple prospective trials have compared femtosecond laser-assisted cataract surgery to conventional phacoemulsification:
- PRECISION and INDEPENDENCE Studies: Large, multi-center randomized trials concluded that FLACS yields significantly more accurate capsulotomy sizing and centration, correlating to improved refractive outcomes for premium IOLs.
- Reduced Phaco Energy: Studies repeatedly show FLACS can slice phaco time and energy by up to 40-50%, beneficial in advanced nuclear sclerotic cataracts. Surgeons reported lower corneal endothelial cell loss and faster visual rehabilitation.
- Equivalent or Superior Visual Acuity: While final visual acuity in standard monofocal patients often ends up similar to manual phaco, the FLACS group typically sees faster early recovery and less postoperative cylinder. Multifocal or toric-lens recipients show more distinct advantages, with better refractive predictability.
Real-World Experiences
Observational series in diverse clinical settings confirm the core advantages of FLACS:
- High Patient Satisfaction: Patients appreciate the automated approach that feels technologically advanced and can accelerate healing. Many cite minimal astigmatism and crisp vision within days.
- Learning Curve: Surgeons mention an initial learning curve for docking and laser interface, but once surmounted, operative flow is streamlined. Efficiency gains manifest as the team becomes adept at switching from laser suite to phaco room.
- Fewer Wound-Induced Cylinders: A consistent theme is that laser incisions can better maintain corneal architecture, fostering stable refractions with minimal induced cylinders.
Emerging Directions
Ongoing research explores advanced features in FLACS systems:
- Intelligent Imaging: Next-gen devices integrate topography or wavefront data to plan more refined laser incisions, particularly for correcting high astigmatism.
- Presbyopia Solutions: Some lasers experiment with partial-thickness radial or arcuate micro-incisions in the cornea to slightly improve near vision, akin to corneal inlays or presbyLASIK.
- Expanded Indications: Certain complicated cataract subtypes—e.g., posterior polar cataracts or very dense brunescent nuclei—are being studied to see if FLACS confers a definitive safety margin.
Although no single study declares FLACS superior in every dimension, the overall consensus from trials and real-world usage indicates that it significantly refines certain aspects of cataract surgery, delivering measureable benefits especially for complex or premium-lens cases.
Key Considerations for Safety and Efficacy (Effectiveness and Safety)
Achieving Consistent Results
Advocates for FLACS emphasize:
- Predictable Capsulotomy: Irregular or incomplete capsulotomies occasionally occur if the laser energy is miscalibrated or if the patient moves, but overall rates of such issues remain quite low.
- Reduced Intraocular Trauma: By fragmenting the lens before phaco, the procedure often uses less ultrasound energy. This theoretically translates to a kinder approach for corneal endothelium and a smoother postoperative course.
- Fewer Postoperative Complications: Some data suggest a reduced incidence of posterior capsular rupture, though both techniques remain very safe with experienced surgeons.
Potential Drawbacks and Risks
Still, FLACS is not without critiques or hazards:
- Suction Break or Incomplete Laser Pass: If the patient’s eye shifts significantly, the procedure might produce partial or incomplete incisions, forcing a shift to manual methods mid-procedure.
- Cost and Accessibility: The high expense of femtosecond laser platforms can be passed on to patients. This can dissuade those seeking standard insurance coverage or with limited budgets.
- Learning Curve: Surgeons must refine docking, planning incisions, and verifying real-time imaging. Mistakes can cause misalignment, creating potential complications.
- No Guaranteed Refractive Edge: Some argue that for routine, straightforward cataracts, manual phaco by a skilled surgeon yields nearly identical outcomes, calling into question the cost-benefit ratio for FLACS in simpler cases.
Postoperative Healing
FLACS can speed up early stability in some patients, letting them experience clearer vision within days. However, final outcomes remain dependent on typical healing factors: patient compliance with drops, corneal health, and potential coexisting ocular conditions (like mild macular changes or meibomian gland dysfunction).
Patient Suitability and Informed Consent
Surgeons assess each patient’s ocular anatomy, lens hardness, and financial considerations. Detailed explanations about the procedure’s enhancements, possible extra costs, and realistic outcome differences empower patients to make a comfortable choice. Typically, FLACS is particularly favored by those seeking premium IOL implants or who have borderline corneal or lens complexities—groups likely to appreciate the refined control offered by femtosecond lasers.
Considering the Price Tag: Therapy Cost for Femtosecond Laser-Assisted Cataract Surgery
Prices for femtosecond laser-assisted cataract surgery (FLACS) vary among surgical centers, influenced by the laser’s capital expense, maintenance fees, and local market factors. Some clinics charge a premium “technology fee” from a few hundred to over a thousand dollars per eye in addition to standard cataract surgery costs. Insurance typically covers the base cataract procedure but may not fully reimburse the extra FLACS portion—especially if considered elective or “premium.” Patients opting for advanced IOLs (like toric or multifocal lenses) often find the combined cost higher, but many appreciate the synergy of FLACS for precise lens positioning. Financing plans, medical credit lines, or “cash pay” discounts might ease the burden. As a rule, verifying coverage details and discussing payment options beforehand helps patients plan for any out-of-pocket expenses.
Disclaimer: This article is for informational purposes only and does not replace professional medical advice, diagnosis, or treatment. Always consult a qualified eye care specialist to determine whether femtosecond laser-assisted cataract surgery is appropriate for your specific condition.
We invite you to share this article with friends, family, or online communities. Feel free to use our Facebook and X (formerly Twitter) share buttons—or any preferred platform—to help others discover how femtosecond laser-assisted cataract surgery can deliver precision and speed for optimal cataract recovery.