What is Fuchs Dystrophy?
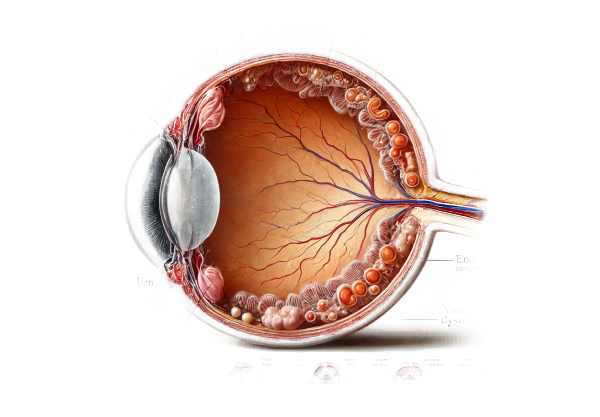
Fuchs’ Dystrophy is a progressive eye disease that affects the cornea, or clear front surface of the eye. This condition is distinguished by the progressive deterioration of the endothelial cells that line the inner layer of the cornea. These cells are in charge of maintaining the proper fluid balance within the cornea, which keeps it clear. As endothelial cells deteriorate, fluid accumulates, causing the cornea to swell and become cloudy, resulting in vision problems. Fuchs’ Dystrophy usually affects both eyes and is more common in older people, especially women.
Detailed Investigation of Fuchs’ Dystrophy
Fuchs’ Dystrophy (FECD) is an inherited disorder that primarily affects the cornea’s endothelium. This inner layer of the cornea is responsible for keeping the cornea clear by removing excess fluid. The disease progresses slowly, often over several decades, and can severely impair vision if not treated properly.
Pathophysiology
The primary issue in Fuchs’ Dystrophy is the degeneration of endothelial cells. These cells are necessary for corneal deturgescence, which is the state of relative dehydration required for corneal transparency. Endothelial cells in a healthy eye regulate fluid levels through an active pump mechanism. In Fuchs’ Dystrophy, the loss of these cells disrupts the balance, causing fluid accumulation, swelling (edema), and corneal thickening.
Clinical Stages
Fuchs’ Dystrophy is usually divided into two stages.
- Early Stage (Guttata): The disease begins with the formation of tiny bumps known as guttae on the back surface of the cornea. These guttae are focal thickenings of Descemet’s membrane, which serves as the basement membrane for endothelial cells. Patients may not notice any significant symptoms at this stage, but some may experience minor visual disturbances or glare.
- Later Stage (Edematous Stage): As the disease progresses, more endothelial cells are lost, resulting in increased corneal edema. This causes significant visual impairment. Symptoms include blurred vision, especially in the morning, which may improve throughout the day as the cornea dries. In severe cases, persistent swelling can cause painful blisters on the cornea’s surface, a condition known as bullous keratopathy.
Symptoms
The symptoms of Fuchs’ Dystrophy vary depending on the stage of the disease.
- Blurred Vision: This is usually worse when you wake up and may improve throughout the day.
- Glare and Halos: Increased sensitivity to light, causing glare and halos around lights, particularly at night.
- Pain: In the advanced stages, bullous keratopathy can cause pain.
- Decreased Contrast Sensitivity: Difficulty distinguishing between subtle grey tones or colors.
- Cloudy or Hazy Vision: An overall cloudiness or haziness that makes it difficult to see fine details.
Risk Factors
Fuchs’ Dystrophy is more common in women than men and typically affects people over 50. While the exact cause is unknown, genetics play a major role. The condition can be inherited in an autosomal dominant manner, which means that a single copy of the altered gene in each cell is enough to cause the disorder. Other risk factors are:
- Family History: A strong family history of the disease heightens the risk.
- Gender: Women are more likely to develop Fuchs Dystrophy.
- Age: The risk rises with age, especially after 50.
Genetic Basis
Fuchs’ Dystrophy is associated with mutations in several genes, including the TCF4 gene. These genetic changes can disrupt endothelial cells’ normal function, causing gradual degeneration. Genetic testing can occasionally detect these mutations, providing useful information for diagnosis and family planning.
Effect on Vision and Quality of Life
As Fuchs’ Dystrophy progresses, the effects on vision and daily life can be severe. In the early stages, patients may experience minor visual disturbances, which can interfere with activities such as reading or driving at night. In later stages, vision can become severely impaired, making it difficult to perform daily tasks and lowering overall quality of life. Bullous keratopathy can also cause debilitating pain.
Complications
If left untreated, Fuchs’ Dystrophy can cause severe complications, including:
- Persistent Corneal Edema: Chronic swelling can cause scarring and further loss of vision.
- Bullous Keratopathy: Painful blisters on the cornea may form, causing significant discomfort.
- Corneal Scarring: Prolonged edema and inflammation can cause permanent scarring on the cornea, necessitating a corneal transplant.
Differential Diagnosis
Several other conditions can present with symptoms similar to Fuchs’ Dystrophy, so differential diagnosis is critical. This includes:
- Other Corneal Dystrophies include posterior polymorphous dystrophy and congenital hereditary endothelial dystrophy.
- Keratoconus is a condition in which the cornea thins and bulges into a cone shape.
- Corneal Edema from Other Causes: This includes trauma, surgery, or inflammation.
Epidemiology: Fuchs’ Dystrophy is a common corneal dystrophy. It is expected to affect 4% of people over the age of 40 in the United States. However, the prevalence may differ across populations and geographical regions.
Diagnostic methods
Fuchs’ Dystrophy is diagnosed using a combination of clinical evaluation, imaging studies, and genetic testing to confirm the diagnosis and determine the disease’s severity.
Clinical Evaluation
An ophthalmologist usually performs a comprehensive eye examination to make the initial diagnosis of Fuchs’ Dystrophy. This includes:
- Slit-Lamp Examination: A thorough examination of the cornea with a slit lamp microscope allows the ophthalmologist to see guttae, corneal edema, and other distinguishing features.
- Visual Acuity Test: Evaluates the patient’s vision to determine the degree of visual impairment.
- Intraocular Pressure Measurement: Measuring the pressure inside the eye to rule out glaucoma, which can occur in conjunction with Fuchs’ Dystrophy.
Imaging Studies
Advanced imaging techniques provide detailed information about the cornea’s structure and aid in assessing the progression of the disease.
- Specular Microscopy: This non-invasive imaging technique enables the visualization and counting of endothelial cells. It aids in measuring cell density and detecting morphological changes in cells.
- Optical Coherence Tomography (OCT): OCT generates high-resolution cross-sectional images of the cornea, allowing for the measurement of corneal thickness and edema.
- Pachymetry: Measuring corneal thickness can help determine the extent of edema. Advanced Fuchs’ Dystrophy is characterized by increased corneal thickness.
Genetic Testing
In some cases, genetic testing can be used to identify mutations linked to Fuchs’ Dystrophy. This is especially useful for confirming diagnoses in atypical cases and for family planning. Testing typically includes:
- Blood Sample: A blood sample is taken for DNA testing.
- Genetic Sequencing: Sequencing the TCF4 gene and other related genes to detect pathogenic mutations.
Additional Diagnostic Tools
Other diagnostic tools and tests that can be used are:
- Confocal Microscopy: Provides detailed images of the corneal layers, including the endothelium, which can be used to assess cell morphology and density.
- Fluorescein Angiography: While not commonly used to diagnose Fuchs’ Dystrophy, this test can help assess corneal health and detect other ocular conditions.
Treatment
Treatment for Fuchs’ Dystrophy focuses on symptom management, slowing disease progression, and improving vision. The approach changes depending on the stage of the disease and the severity of the symptoms. Here are some innovative and emerging therapies, as well as standard treatment options:
- Medications and Eye Drops: – Hypertonic Saline Drops/Ointments can reduce corneal swelling by drawing fluid out. They are especially effective for reducing morning vision blur.
- Anti-inflammatory Drops: Nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce inflammation and pain.
- Use of Hairdryer: Blowing warm air from a hairdryer at arm’s length can help dry the cornea, reducing morning blurriness and temporarily improving vision.
- Contact Lenses: – Soft Contact Lenses: Can enhance vision and protect the cornea.
- Bandage Contact Lenses: By forming a protective layer over the cornea, these lenses can help relieve the pain and discomfort associated with bullous keratopathy.
- Surgical Options: – Endothelial Keratoplasty (DSEK/DSAEK/DMEK): The most commonly used surgical treatment for advanced Fuchs’ dystrophy. The damaged endothelial layer is selectively removed and replaced by healthy donor tissue. Descemet’s Stripping Endothelial Keratoplasty (DSEK) and Descemet Membrane Endothelial Keratoplasty (DMEK) are two popular techniques, with DMEK producing better visual results and faster recovery.
- Penetrating Keratoplasty (PKP): Also known as a full-thickness corneal transplant, this procedure replaces the entire cornea with a donor cornea. This is usually reserved for situations where other surgical methods are not appropriate.
Innovative and Emerging Therapies
- Rho Kinase Inhibitors: These are emerging as potentially effective treatments for Fuchs’ Dystrophy. Rho kinase inhibitors can help improve endothelial cell regeneration and function. Clinical trials are underway to determine their efficacy and safety.
- Gene Therapy: Research into gene therapy aims to target the genetic mutations that cause Fuchs’ Dystrophy. Correcting the underlying genetic defect may allow disease progression to be halted or reversed.
- Stem Cell Therapy: Stem cell research has the potential to regenerate damaged corneal endothelial cells. Techniques include using stem cells to generate healthy endothelial cells that can be transplanted into the cornea.
- Tissue Engineering: Advances in tissue engineering are paving the way for the creation of artificial corneal tissues capable of replacing damaged ones. This approach has the potential to reduce reliance on donated tissues while also improving treatment accessibility.
- Pharmacological Advances: New drugs are being developed to improve endothelial cell function and reduce cell loss. These medications target specific pathways involved in endothelial cell survival and function.
Combining standard treatments with these innovative approaches offers the possibility of more effective management and potentially curative treatments for Fuchs’ Dystrophy.
Reducing Fuchs’ Dystrophy Risk
While Fuchs’ Dystrophy is primarily genetic and cannot be completely avoided, there are steps that can be taken to reduce risk and manage early symptoms:
- Regular Eye Exams: Schedule regular eye exams to detect early signs of Fuchs’ Dystrophy and track its progression.
- Manage Blood Pressure: Excessive blood pressure can worsen corneal edema. Maintain a healthy blood pressure with diet, exercise, and medication, if necessary.
- Avoid Eye Trauma: Wear safety glasses when participating in activities that pose a risk of eye injury.
- Healthy Diet: Eat a well-balanced diet high in antioxidants to promote overall eye health. Include foods rich in vitamins A, C, E, and omega-3 fatty acids.
- Stay Hydrated: Proper hydration promotes corneal health. Drink plenty of water during the day.
- Use Humidifiers: In dry environments, a humidifier can help keep moisture levels in the air, preventing the eyes from drying out.
- Avoid Smoking: Smoking increases the likelihood of developing eye diseases. Avoid smoking, and limit your exposure to secondhand smoke.
- Wear Sunglasses: When you’re outside, protect your eyes from UV radiation by wearing UV-protective sunglasses.
Individuals who follow these best practices can improve their overall eye health and potentially slow the progression of Fuchs’ dystrophy.
Trusted Resources
Books
- “Cornea: Fundamentals, Diagnosis, and Management” by Jay H. Krachmer, Mark J. Mannis, and Edward J. Holland
- “Fuchs’ Endothelial Dystrophy: Pathogenesis and Management” by Kathryn Colby
Online Resources
- National Eye Institute: NEI
- American Academy of Ophthalmology: AAO
- Mayo Clinic: Mayo Clinic
- Cornea Research Foundation of America: CRFA






