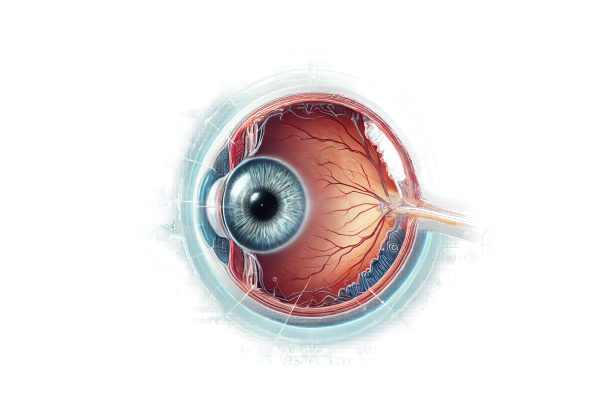
What is Glaucoma?
Glaucoma caused by retinal disorders is a secondary type of glaucoma that develops as a result of underlying retinal diseases. These retinal conditions can raise intraocular pressure (IOP) or damage the optic nerve, resulting in glaucomatous changes. Retinal disorders such as diabetic retinopathy, retinal vein occlusion, and retinopathy of prematurity can disrupt aqueous humor outflow or cause neovascularization, both of which contribute to the development of glaucoma. Understanding the relationship between retinal diseases and glaucoma is critical for proper diagnosis and treatment.
Comprehensive Examination of Glaucoma in conjunction with Retinal Disorders
Glaucoma and retinal disorders are caused by a complex interplay of pathophysiological mechanisms that result in increased intraocular pressure (IOP) and damage to the optic nerve. This condition can result from a variety of retinal diseases, each of which contributes to the development of glaucoma via a different pathway. Understanding these mechanisms is critical for successful management and treatment of this type of glaucoma.
Pathophysiology
The pathophysiology of glaucoma associated with retinal disorders entails several key mechanisms:
- Neovascularization: Neovascularization is a primary mechanism in which abnormal blood vessels form on the iris and trabecular meshwork. Retinal disorders like diabetic retinopathy and retinal vein occlusion frequently cause ischemia, which causes the release of vascular endothelial growth factor (VEGF). This, in turn, promotes the formation of new blood vessels, which can obstruct the trabecular meshwork and impede aqueous humor outflow, resulting in increased IOP.
- Inflammation: Chronic inflammation caused by retinal disorders can also lead to glaucoma. Conditions such as uveitis and retinitis can cause inflammatory cells and mediators to accumulate in the anterior chamber, blocking the trabecular meshwork and raising IOP. In addition, inflammation can cause synechiae to form, obstructing aqueous outflow even more.
- Mechanical Obstruction: Retinal detachment and proliferative vitreoretinopathy may cause retinal pigment epithelial cells and fibroblasts to migrate into the eye’s anterior segment. These cells can form membranes that physically block the trabecular meshwork, resulting in elevated IOP.
- Pigment Dispersion: Certain retinal disorders can cause pigment dispersion, which occurs when pigment granules from the iris or ciliary body are released into the anterior chamber. These granules can accumulate in the trabecular meshwork, reducing its ability to drain aqueous humor and thus increasing IOP.
Retinal Disorders Associated With Glaucoma
Several retinal disorders are frequently associated with the development of glaucoma.
- Diabetic Retinopathy: This condition causes damage to the retinal blood vessels as a result of prolonged high blood glucose levels. Diabetic retinopathy can cause neovascularization and subsequent neovascular glaucoma, which is especially difficult to treat due to the aggressive nature of the new blood vessels.
- Retinal Vein Occlusion: This condition develops when a vein in the retina becomes clogged, resulting in hemorrhage and swelling. The resulting ischemia can cause neovascularization, raising the risk of neovascular glaucoma.
- Retinopathy of Prematurity: This condition affects premature infants and causes abnormal blood vessel growth in the retina. The abnormal vessels can spread into the anterior segment, resulting in secondary glaucoma.
- Uveitis: Inflammation of the uveal tract can affect the retina, resulting in the accumulation of inflammatory cells in the anterior chamber. Chronic uveitis can lead to the formation of synechiae and secondary angle closure, resulting in high IOP and glaucoma.
- Retinal Detachment: In cases of retinal detachment, the migration of retinal cells into the anterior chamber can result in the formation of membranes that prevent aqueous outflow. Proliferative vitreoretinopathy, a complication of retinal detachment surgery, can exacerbate the situation.
- Sickle Cell Retinopathy: This condition is distinguished by the occlusion of retinal blood vessels as a result of sickle cell disease. Ischemia and neovascularization are common, which increases the risk of neovascular glaucoma.
Clinical Presentation
Patients with glaucoma and retinal disorders may exhibit a range of symptoms and clinical findings:
- Elevated Intraocular Pressure: Persistent elevation of IOP despite standard glaucoma treatments is a reliable indicator of secondary glaucoma. This elevation could be acute or chronic, depending on the underlying retinal condition.
- Visual Disturbances: Patients may experience blurred vision, visual field defects, or sudden vision loss, especially if the retinal disorder causes significant ischemia or detachment.
- Ocular Pain: Pain can be caused by an increase in intraocular pressure or inflammation associated with the retinal disorder.
- Visible Blood Vessels: In neovascular glaucoma, abnormal blood vessels can be seen on the iris’ surface and in the anterior chamber angle.
- Red Eye: Chronic redness and inflammation may be associated with retinal disorders that cause uveitis or neovascularization.
Diagnostic Challenges
Diagnosing glaucoma associated with retinal disorders poses several challenges:
- Atypical Presentation: A retinal disorder can cause an atypical presentation of glaucoma. Standard glaucoma treatments may not effectively control IOP, necessitating further investigation.
- Detection of Retinal Disorder: Recognizing the presence of a retinal disorder requires a high level of suspicion, particularly in patients with refractory glaucoma. Detailed ocular examinations and imaging studies are required.
- Differential Diagnosis: Differentiating glaucoma caused by retinal disorders from other types of secondary glaucoma, such as neovascular or inflammatory glaucoma, necessitates careful consideration of clinical and imaging findings.
Diagnostic Tools for Retinal Disorder Glaucoma
Glaucoma associated with retinal disorders is diagnosed using a combination of clinical examinations, imaging studies, and specialized tests. Here are the main diagnostic methods used:
Clinical Examination
- Comprehensive Eye Exam: A complete eye examination is required, which includes intraocular pressure (IOP) measurement, slit-lamp biomicroscopy, and gonioscopy. These evaluations aid in the detection of anterior segment abnormalities, angle structure, and the presence of a retinal disorder.
- Dilated Fundus Examination: A thorough examination of the retina and optic nerve is necessary. This examination may reveal signs of retinal detachment, retinal vein occlusion, diabetic retinopathy, and other retinal disorders.
Imaging Studies
- Optical Coherence Tomography (OCT): OCT can produce high-resolution images of the retina and optic nerve head. It can assist in detecting macular edema, retinal detachment, and other posterior segment abnormalities associated with retinal disorders.
- Fluorescein Angiography: Fluorescein angiography evaluates the retinal vasculature. It is especially useful in detecting areas of ischemia, neovascularization, and other vascular changes caused by retinal disorders.
- Ultrasound Biomicroscopy (UBM): UBM can produce high-resolution images of the anterior segment structures, such as the iris, ciliary body, and anterior chamber angle. It is especially useful in detecting membranes and synechiae that may obstruct aqueous outflow.
- B-Scan Ultrasonography: This imaging modality is useful for assessing the size and extent of larger intraocular structures. B-scan ultrasonography detects retinal detachments and other structural changes.
Specialized Tests
- Electroretinography (ERG): ERG measures the electrical responses of different cell types in the retina, such as photoreceptors and ganglion cells. It is useful in evaluating retinal function in conditions such as retinitis pigmentosa and diabetic retinopathy.
- Visual Field Testing: This test measures the extent of visual field loss, which can aid in determining the severity of glaucomatous damage and tracking disease progression.
- Anterior Segment Optical Coherence Tomography(AS-OCT): AS-OCT provides detailed images of the anterior segment structures, which aid in identifying angle closure and other changes that can contribute to elevated IOP.
Treatment
The treatment of glaucoma caused by retinal disorders must address both the elevated intraocular pressure (IOP) and the underlying retinal condition. Here are the conventional and emerging treatment options:
- Medications: Medications to lower IOP are typically used as the first line of treatment. This includes:
- Prostaglandin Analogs: Enhance uveoscleral outflow of aqueous humor.
- Beta-blockers: Decrease aqueous humor production.
- Alpha Agonists: Both reduce production and increase outflow.
- Carbonic Anhydrase Inhibitors: Reduces aqueous humor production.
- Rho Kinase Inhibitors: Enhances trabecular outflow.
- Laser Therapy: Laser treatments are commonly used to manage IOP.
- Laser Trabeculoplasty: Improves outflow from the trabecular meshwork.
- Panretinal Photocoagulation (PRP): Used to treat neovascular glaucoma, particularly diabetic retinopathy, by reducing retinal ischemia and subsequent neovascularization.
- Surgical Interventions: Surgery may be needed when medications and laser therapy are insufficient.
- Trabeculectomy: Opens a new drainage pathway for aqueous humor.
- Glaucoma Drainage Devices: Implants such as the Ahmed and Baerveldt devices aid in aqueous humor drainage.
- Cyclophotocoagulation: Reduces aqueous humor production by focusing on the ciliary body.
Retinal Disorder-Specific Treatments
- Anti-VEGF Therapy: Intravitreal injections of anti-VEGF agents (e.g., bevacizumab, ranibizumab) are used to prevent neovascularization in diabetic retinopathy and retinal vein occlusion.
- Vitrectomy: Surgical removal of the vitreous gel, especially in cases of proliferative vitreoretinopathy or retinal detachment, to relieve traction and treat anterior segment complications.
- Retinal Laser Treatment: Focal or grid laser photocoagulation is used to treat macular edema caused by retinal vein occlusion or diabetic retinopathy.
Innovative and Emerging Therapies
- Minimally Invasive Glaucoma Surgery (MIGS): New techniques aim to reduce IOP while minimizing complications:
- iStent: A small device implanted to increase trabecular outflow.
- Hydrus Microstent: Promotes aqueous humor outflow via the trabecular meshwork.
- Gene Therapy: Researchers are looking into therapies that can address genetic factors that contribute to both retinal disorders and glaucoma.
- Neuroprotection: New treatments seek to protect the optic nerve from damage. These include pharmacological agents that promote retinal ganglion cell health and function.
- Regenerative Medicine: Methods such as stem cell therapy are being studied for their ability to repair or replace damaged retinal and optic nerve tissues.
To effectively treat glaucoma associated with retinal disorders, a personalized approach is required, taking into account the specific type and characteristics of the retinal disease, the severity of the glaucoma, and the patient’s overall health.
Best Practices to Avoid Glaucoma Related to Retinal Disorders
- Regular Eye Exams: Have comprehensive eye exams to detect any early signs of retinal disorders and associated glaucoma. Early detection is critical to effective management.
- Control Systemic Conditions: Treat systemic conditions like diabetes, hypertension, and vascular disease, which can all contribute to retinal disorders.
- Monitor Retinal Health: If you have a retinal disorder, follow your ophthalmologist’s recommendations for monitoring and managing the condition to avoid complications that may lead to glaucoma.
- Healthy Lifestyle: To support overall eye health, live a healthy lifestyle that includes a balanced diet, regular exercise, and abstaining from smoking and excessive alcohol consumption.
- Protective Eyewear: Wear protective eyewear in environments where there is a risk of eye injury or exposure to hazardous substances.
- Family History Awareness: Know your family’s history of retinal disorders and glaucoma. Genetic predispositions can heighten risk.
- UV Exposure Avoidance: Wear UV-blocking sunglasses to protect your eyes from excessive ultraviolet (UV) light.
- Manage Stress: Chronic stress can be detrimental to overall health, including eye health. Practice stress-reduction techniques such as meditation, exercise, and getting enough sleep.
- Stay Informed: Learn about the symptoms and risk factors for retinal diseases and glaucoma. Early detection can lead to timely medical treatment.
- Adhere to Treatment Plans: If you have a retinal disorder, follow your prescribed treatment plan to avoid complications and lower your risk of developing secondary glaucoma.
Individuals who follow these preventive measures can significantly reduce their risk of developing glaucoma caused by retinal disorders while also maintaining good ocular health.
Trusted Resources
Books
- “The Glaucoma Book: A Practical, Evidence-Based Approach to Diagnosis and Management” by Paul N. Schacknow and John R. Samples
- “Retina” by Stephen J. Ryan
- “Medical Retina” by Frank G. Holz and Richard F. Spaide






