Introduction to Elevated EVP Glaucoma
Glaucoma with elevated episcleral venous pressure (EVP) is a type of secondary open-angle glaucoma in which an increase in intraocular pressure (IOP) is directly related to increased pressure in the episcleral veins. This condition occurs when normal aqueous humor drainage is disrupted due to elevated pressure in the episcleral venous system, resulting in increased IOP. Over time, this elevated pressure can damage the optic nerve, resulting in progressive visual field loss. Understanding the underlying causes, symptoms, and implications of elevated EVP is critical for accurate diagnosis and treatment.
Clinical Features of Elevated EVP Glaucoma
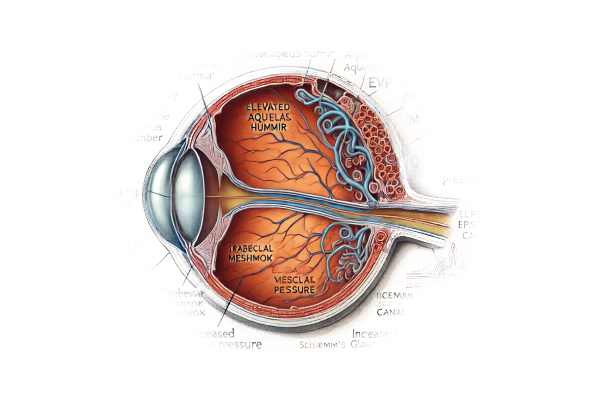
Glaucoma with elevated episcleral venous pressure (EVP) is a complex condition that disrupts the normal ocular drainage system. In a healthy eye, the ciliary body’s aqueous humor flows through the pupil into the anterior chamber before exiting the eye via the trabecular meshwork into Schlemm’s canal and eventually draining into the episcleral veins. This drainage system maintains a delicate balance, keeping intraocular pressure (IOP) within normal limits. However, when episcleral venous pressure rises, this equilibrium is disrupted, resulting in elevated IOP and subsequent glaucoma.
Pathophysiology
The pathophysiology of glaucoma associated with elevated EVP includes several key factors:
- Episcleral Venous Pressure: The episcleral veins are an important part of the eye’s aqueous humor outflow system. Elevated EVP can be caused by a variety of conditions, including arteriovenous malformations, Sturge-Weber syndrome, and thyroid disease. When the pressure in these veins rises, it prevents the normal outflow of aqueous humor, resulting in higher IOP.
- Increased Intraocular Pressure: Elevated EVP obstructs aqueous humor outflow, resulting in increased IOP. Prolonged elevated IOP puts pressure on the optic nerve, resulting in optic neuropathy and glaucomatous changes. Optic nerve damage is progressive and can result in irreversible vision loss if not treated properly.
- Optic Nerve Damage: Elevated IOP causes mechanical compression and impaired blood flow to the optic nerve, resulting in axonal damage and loss of retinal ganglion cells. This process causes characteristic glaucomatous changes, such as optic disc cupping and visual field defects.
Causes of Elevated EVPs
Several conditions can result in high episcleral venous pressure:
- Orbital and Systemic Conditions: Thyroid eye disease, arteriovenous malformations, carotid-cavernous fistulas, and Sturge-Weber syndrome can all result in elevated EVP. These conditions are characterized by abnormal blood flow or vascular malformations that elevate venous pressure in the episcleral veins.
- Idiopathic: In some cases, elevated EVP may be caused by an unknown systemic or orbital condition. Idiopathic cases pose a diagnostic challenge and necessitate a thorough examination to rule out other possible causes.
- Medications and External Factors: Certain medications, including corticosteroids, and external factors, such as wearing tight neckties, can temporarily increase EVP. Identifying and modifying these factors can help manage the condition.
Clinical Presentation
Patients with glaucoma with elevated EVP usually have symptoms related to elevated IOP and optic nerve damage:
- Elevated Intraocular Pressure: Patients frequently have consistently elevated IOP despite standard glaucoma treatments. The refractory nature of IOP elevation raises the possibility of secondary causes, including elevated EVP.
- Visual Field Loss: Glaucoma causes progressive peripheral vision loss. Patients may be asymptomatic at first but develop peripheral vision problems, which can progress to tunnel vision if not treated.
- Optic Disc Changes: An ophthalmoscopic examination reveals optic disc cupping and pallor. The optic disc appears excavated as nerve fibers are lost, and the cup-to-disc ratio increases.
- Ocular Surface Changes: Chronic high IOP can cause changes in the corneal endothelium and conjunctival hyperemia. These changes may be visible under a slit lamp.
Diagnostic Challenges
Diagnosing glaucoma with elevated EVP presents several challenges:
- Differentiating from Primary Glaucoma: Distinguishing this condition from primary open-angle glaucoma can be difficult. A detailed patient history and a thorough ocular examination are required. Patients with refractory IOP should be suspected of having elevated EVP despite receiving maximum medical therapy.
- Identifying Underlying Causes: Identifying the root cause of elevated EVP is critical for effective management. Orbital ultrasound, magnetic resonance imaging (MRI), or computed tomography (CT) angiography may be required to diagnose vascular malformations or orbital masses.
- Measuring EVP: Direct measurement of EVP can be difficult and is not commonly done in clinical settings. Indirect assessment, such as observing episcleral venous plexus dilation and blood flow, can provide clues.
Implications and Prognoses
The prognosis for patients with glaucoma and elevated EVP varies according to the underlying cause and the timing of diagnosis and treatment. Early detection and management are critical for avoiding irreversible optic nerve damage and maintaining vision. Patients with treatable underlying conditions, such as arteriovenous malformations or thyroid eye disease, may see significant improvement with the right treatment. Patients with idiopathic or refractory cases, on the other hand, may require long-term management to keep IOP under control and prevent further optic nerve damage.
Management of glaucoma with elevated EVP frequently requires a multidisciplinary approach, which includes collaboration with neurologists, endocrinologists, and vascular specialists. Surgical interventions, such as trabeculectomy or glaucoma drainage devices, may be required in refractory cases to achieve adequate IOP control.
Clinical Diagnosis of High EVP Glaucoma
Diagnosing glaucoma with elevated episcleral venous pressure is a multi-step process that includes clinical examinations, imaging studies, and specialized tests. Given the complexities and potential causes of elevated EVP, a thorough and systematic approach is required for accurate diagnosis.
Clinical Examination
- Patient History: A thorough patient history is essential for identifying potential risk factors and underlying conditions. Patients should be asked about any previous thyroid disease, vascular malformations, or symptoms of orbital pathology, such as proptosis or pulsatile tinnitus.
- Ocular Examination: A comprehensive ocular examination includes measuring intraocular pressure (IOP), assessing the optic nerve head, and evaluating the anterior and posterior segments of the eye. Elevated IOP despite maximum medical therapy may indicate secondary causes, such as elevated EVP.
- Slit-Lamp Examination: A slit-lamp examination may reveal conjunctival hyperemia and dilated episcleral veins, both of which indicate elevated EVP. An examination of the anterior chamber angle with gonioscopy can help rule out other types of secondary glaucoma.
Imaging Studies
- Orbital Ultrasound: Orbital ultrasound is a non-invasive imaging technique for detecting structural abnormalities in the orbit, such as vascular malformations or orbital masses. Doppler ultrasound can measure blood flow and identify abnormal arteriovenous communications.
- Magnetic Resonance Imaging (MRI): MRI of the orbit and brain can help visualize soft tissue structures and diagnose conditions like carotid-cavernous fistulas, orbital masses, and thyroid eye disease. MRI with contrast can improve the visualization of vascular structures.
- Computed Tomography (CT) Angiography: CT angiography produces detailed images of the vascular system and can detect arteriovenous malformations, fistulas, and other vascular anomalies that cause elevated EVP. It is especially useful when assessing the carotid-cavernous sinus region.
Specialized Tests
- Episcleral Venous Pressure Measurement: A venomanometer can be used to directly measure episcleral venous pressure, though this is not commonly done. This device measures the pressure required to collapse the episcleral veins, giving an estimate of EVP.
- Fluorescein Angiography: Fluorescein angiography can determine the health of the retina and choroidal circulation. It is useful for detecting abnormal vascular leakage or shunting caused by conditions like Sturge-Weber syndrome.
- Optical Coherence Tomography (OCT): OCT can produce high-resolution images of the retinal nerve fiber layer and optic nerve head. It is critical for monitoring glaucomatous damage and determining the extent of optic nerve atrophy.
Therapies for Elevated EVP Glaucoma
The treatment of glaucoma with elevated episcleral venous pressure (EVP) focuses on lowering intraocular pressure (IOP) while also addressing the underlying cause of the elevated EVP. Here are the conventional and emerging treatment options:
- Medications: Topical and systemic medications are frequently used to lower IOP during the initial phase of treatment. This may include:
- Prostaglandin Analogs: Enhance uveoscleral outflow of aqueous humor.
- Beta-blockers: Decrease aqueous humor production.
- Alpha Agonists: Reduces aqueous humor production while increasing uveoscleral outflow.
- Carbonic Anhydrase Inhibitors: Reduces aqueous humor production.
- Rho Kinase Inhibitors: Enhances trabecular outflow.
- Laser Therapy: Laser treatments can help to improve aqueous humor outflow. Common procedures include:
- Selective Laser Trabeculoplasty (SLT): This procedure improves outflow by targeting the trabecular meshwork.
- Argon Laser Trabeculoplasty (ALT): Similar to SLT, but with a different type of laser.
- Surgical Interventions: When medications and laser therapy are insufficient, surgical options may be considered.
- Trabeculectomy: Opens a new drainage pathway for aqueous humor.
- Glaucoma Drainage Devices: Implants such as the Ahmed or Baerveldt implants aid in aqueous humor drainage.
- Cyclophotocoagulation: Uses a laser to reduce ciliary body function and aqueous humor production.
Innovative and Emerging Therapies
- Minimally Invasive Glaucoma Surgery (MIGS): Newer techniques designed to lower IOP with fewer complications than traditional surgery. This includes:
- iStent: A small device implanted in the trabecular meshwork to increase outflow.
- Xen Gel Stent: A soft, gelatinous implant that opens a new drainage pathway.
- Hydrus Microstent is an intracanalicular scaffold that improves outflow.
- Gene Therapy: Researchers are looking into gene therapies that target the underlying mechanisms of glaucoma. These treatments seek to modify the genetic factors that contribute to the disease.
- Neuroprotection: Strategies to protect the optic nerve from damage are being investigated. These include pharmacological agents that promote retinal ganglion cell health and function.
- Regenerative Medicine: Stem cell therapy and other regenerative methods are being investigated to repair or replace damaged optic nerve tissue.
Effective management of glaucoma with elevated EVP necessitates a tailored approach that takes into account the underlying cause, severity of the disease, and the patient’s overall health.
Best Practices to Avoid Glaucoma Caused by Increased Episcleral Venous Pressure
Preventive measures and risk-reduction strategies can have a significant impact on the likelihood of developing glaucoma in patients with elevated EVP. Here are key steps to consider:
- Regular Eye Exams: Get comprehensive eye exams on a regular basis, especially if you have a family history of eye problems or systemic conditions like hypertension or thyroid dysfunction.
- Monitor Systemic Health: Treat any systemic conditions that may affect episcleral venous pressure, such as hypertension, thyroid disorders, or vascular malformations.
- Prevent High Neck Pressure: Avoid wearing tight neckties or collars, which can raise venous pressure in the head and neck.
- Manage Intraocular Pressure: To avoid optic nerve damage, strictly adhere to the prescribed treatments for elevated IOP.
- Healthy Lifestyle: Lead a healthy lifestyle by eating a well-balanced diet, exercising regularly, and refraining from smoking and drinking excessively.
- Protective Measures: Wear protective eyewear in environments where there is a risk of eye injury or exposure to hazardous substances.
- Stay Informed: Learn about the symptoms and risk factors of glaucoma, and seek medical attention immediately if you notice any changes in your vision.
- Control Systemic Inflammation: Treat systemic inflammatory conditions as soon as possible, as they can cause vascular changes that affect EVP.
Individuals who follow these preventive measures can reduce their risk of developing glaucoma caused by elevated EVP while also maintaining their ocular health.
Trusted Resources
Books
- “Glaucoma: Science and Practice” by John C. Morrison and Irvin P. Pollack
- “Clinical Glaucoma Care: The Essentials” by John R. Samples and Paul N. Schacknow
- “Pediatric Glaucoma” by Sharon F. Freedman, Tarek M. Shaarawy, and Mark M. Blecher










