Stargardt disease is one of the most common forms of inherited juvenile macular degeneration, affecting children and young adults and often leading to progressive vision loss. Characterized by mutations in the ABCA4 gene, this retinal condition compromises the photoreceptors and the retinal pigment epithelium (RPE) in the macula, gradually eroding central vision while leaving peripheral sight mostly intact. Daily tasks like reading, recognizing faces, and driving can become increasingly difficult, severely impacting quality of life. Historically, management options for Stargardt disease have been largely limited to low-vision aids and lifestyle adjustments. These measures can help patients adapt but do not address the underlying loss of photoreceptors and RPE cells.
In recent years, regenerative medicine has offered a new horizon for individuals with Stargardt disease. One particularly promising approach focuses on transplanting human embryonic stem cell–derived retinal pigment epithelial (hESC-RPE) cells into the subretinal space. RPE cells support photoreceptor function by supplying nutrients, managing waste byproducts, and participating in the visual cycle. When the native RPE is damaged, photoreceptors starve and die. By replacing or supplementing these vital support cells through hESC-RPE transplantation, researchers aim to stabilize or restore some measure of retinal function, potentially delaying disease progression and preserving precious central vision. Below, we explore how this technology works, the procedures involved, key research findings, clinical safety data, and the costs associated with these cutting-edge stem cell transplants.
Foundations and Key Insights of Stem Cell Therapy
Since its inception, stem cell research has attracted considerable attention for its capacity to regenerate tissues damaged by injury or disease. Human embryonic stem cells (hESCs) stand out for their pluripotent nature, meaning they can develop into any specialized cell type in the body under the right conditions. This trait makes them highly appealing for diseases such as Stargardt disease, where a specific cell population—in this case, RPE cells—requires restoration.
Why RPE Transplants Matter in Stargardt Disease
In healthy eyes, RPE cells line the back of the retina, just beneath the photoreceptor layer. They perform several key tasks:
- Nutrient and Oxygen Supply: They ferry essential nutrients from the choroid to photoreceptors while removing waste.
- Photoreceptor Recycling: RPE cells digest shed outer segments of photoreceptors, keeping the retina free from harmful debris.
- Protective Barrier and Immune Modulation: They help regulate the movement of molecules between the retina and the systemic circulation, maintaining a stable microenvironment.
When ABCA4 mutations lead to lipofuscin buildup, RPE cells become overwhelmed and eventually dysfunctional, culminating in the progressive demise of photoreceptors. The rationale behind hESC-RPE transplants is straightforward: if healthy RPE cells can be introduced, they might preserve photoreceptor function by taking over the supportive tasks the native RPE can no longer manage.
Transitioning from Bench to Bedside
The leap from laboratory studies to actual human treatments involves navigating multiple complexities. Before being used in patients, hESC-RPE cells must be:
- Differentiated Properly: Scientists guide embryonic stem cells through a rigorous differentiation protocol, coaxing them into adopting an RPE-like phenotype—pigmented, hexagonally arranged cells akin to those in the native retina.
- Purified and Characterized: Quality control ensures that the final product is predominantly RPE cells, free from contaminants or undifferentiated stem cells that might form teratomas (abnormal tissue growths).
- Verified for Function: Laboratory tests confirm that these cells exhibit normal RPE markers (e.g., bestrophin, RPE65) and can perform tasks such as phagocytosing photoreceptor outer segments.
- Packaged for Transplant: Investigational teams then embed cells within a scaffold or inject them in suspension, ensuring that they reach the subretinal space and remain viable.
This process demands collaboration among basic scientists, bioengineers, and ophthalmic surgeons. Safety tests and preclinical animal experiments pave the way, ensuring that by the time hESC-RPE reach human trials, they have already cleared extensive scrutiny.
Potential Advantages Over Alternative Therapies
While certain emerging gene therapies aim to correct ABCA4 mutations at the genetic level, hESC-RPE transplantation addresses the downstream tissue damage more directly. Even if gene editing successfully halts lipofuscin accumulation, advanced disease stages often involve large-scale RPE atrophy that cannot be reversed simply by halting further mutations. Reintroducing functional RPE cells provides a structural foundation to rescue or prolong the life of remaining photoreceptors.
Moreover, hESC-RPE therapies may also benefit other conditions involving RPE loss or dysfunction. This cross-applicability—spanning age-related macular degeneration (AMD), choroideremia, or even some rare dystrophies—makes the technology a broader investment in tackling degenerative retinal diseases.
Still, the approach is in its relative infancy, with ongoing clinical trials continuing to refine protocols. Early indicators show promise: stable integration of transplanted cells, potential slowing of disease progression, and in some instances modest gains in visual function. However, challenges remain regarding immunological acceptance, long-term cell survival, and scaling up production while ensuring consistent quality.
Procedure Steps and Considerations for hESC-RPE
Beyond the theoretical appeal, the success of hESC-RPE therapy hinges on meticulous surgical and clinical steps. From patient screening to injection technique, each detail shapes whether transplanted cells can survive and function, and whether patients experience tangible improvements in vision.
Patient Selection and Preoperative Evaluations
Candidates for hESC-RPE transplant typically exhibit:
- Confirmed Stargardt Diagnosis: Genetic testing can verify ABCA4 mutations, while clinical exams identify characteristic flecks and atrophic lesions in the macula.
- Residual Photoreceptors: An eye with advanced scarring or near-total atrophy may offer minimal substrate for rescue, so imaging tools like OCT (optical coherence tomography) help gauge photoreceptor viability.
- Stable Systemic Health: Severe comorbidities or compromised immune systems might escalate the risk of complications or hamper the therapy’s ability to integrate.
Most protocols also include a thorough review of the patient’s ocular history, checking for any prior surgeries, inflammatory conditions, or infections that may complicate the procedure. Clinicians assess baseline visual acuity, glare sensitivity, and retinal sensitivity through specialized tests—like fundus autofluorescence or microperimetry—to track progress post-surgery.
Delivery Methods: Suspension vs. Scaffold
Once patients are cleared for surgery, the chosen hESC-RPE product can be delivered in one of two main ways:
- Cell Suspension: A mixture of RPE cells, typically combined with a supportive medium, is injected directly into the subretinal space via a fine cannula. The rationale is that cells can disperse, settle, and form monolayers that approximate normal RPE architecture. However, ensuring uniform coverage can be challenging, and some cells may fail to integrate.
- Engineered Scaffold: In this approach, hESC-RPE cells grow on a biodegradable or synthetic scaffold, forming a cohesive monolayer. Surgeons then implant this cell-laden patch under the retina, aiming to recapitulate the natural arrangement of RPE. While more complex to produce and implant, scaffolds may enhance cell survival and uniform coverage.
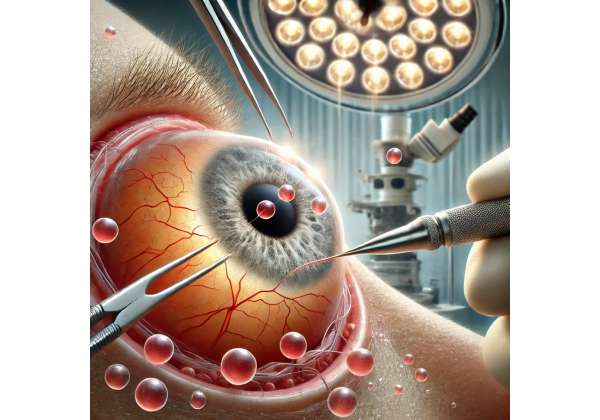
Both strategies require advanced surgical visualization tools. A common approach entails a standard three-port pars plana vitrectomy, after which a retinotomy (small retinal hole) is created. The cell suspension or scaffold is then carefully placed under the retina, displacing it slightly to allow cells contact with Bruch’s membrane or the existing RPE layer.
Managing Immunosuppression
Though the eye is considered an immune-privileged site, transplanted cells—even if derived from human embryonic sources—may prompt immunologic responses. To mitigate this risk, many clinical protocols rely on transient immunosuppression:
- Oral Medications: Drugs like tacrolimus or mycophenolate mofetil may be used for a period pre- and post-surgery, suppressing T-cell mediated immune reactions.
- Steroid Eye Drops: Topical steroids help reduce local inflammation in the immediate postoperative phase, preventing tissue rejection or scarring.
- Individualized Monitoring: Depending on the patient’s response, these immunosuppressive regimens can be tapered over weeks or months. Some ongoing studies aim to identify minimal or alternative immunosuppression strategies to avoid systemic side effects.
Postoperative Recovery and Rehabilitation
Following hESC-RPE transplantation, patients typically undergo:
- Immediate Follow-Up: Monitoring for surgical complications—like retinal detachment, increased intraocular pressure, or infection—during the first week.
- Tapered Follow-Up Schedule: Subsequent visits at set intervals (1 month, 3 months, 6 months, etc.) track ocular coherence tomography (OCT) changes, autofluorescence patterns, and functional improvements in vision.
- Adherence to Medication: Immunosuppressants or anti-inflammatory drops are critical to protecting engrafted cells from rejection.
- Lifestyle Guidelines: Avoiding strenuous activities, wearing protective eyewear, and reporting any visual anomalies swiftly can head off complications.
While many patients desire immediate vision gains, any improvement in Stargardt disease may be gradual and modest. Typically, the initial goal is to preserve existing function and slow progression. Over time, some individuals may see more notable benefits—like better reading vision, improved color discrimination, or reduced central scotomata.
Breakthrough Trials and Emerging Findings
In the realm of hESC-RPE therapy for Stargardt disease, both academic institutions and private biotech companies have launched clinical trials to assess safety, feasibility, and preliminary efficacy. These studies often involve small patient cohorts but provide valuable windows into how transplanted cells behave in human retinas.
Early Phase I/II Trials
Some of the earliest efforts to treat Stargardt disease with hESC-RPE came from teams working on parallel projects for age-related macular degeneration. Early phase I/II trials typically observed:
- Safety Over Efficacy: The primary endpoint revolved around whether transplanted cells triggered harmful immune responses, uncontrolled growth, or tumorous changes. So far, no major complications like teratoma formation have been reported in these small cohorts.
- Stable or Slightly Improved Visual Acuity: While most patients had advanced disease, some displayed moderate improvements in best-corrected visual acuity (BCVA). Others reported more subjective gains such as increased contrast sensitivity or less distortion.
- Retinal Imaging Confirmation: OCT scans sometimes revealed a hyperreflective layer in the subretinal space consistent with transplanted RPE, suggesting the cells remained in place over months to years.
Encouragingly, none of these initial participants experienced catastrophic vision loss due to the procedure itself. Mild adverse events typically included transient inflammation or mild epiretinal membrane formation—both manageable with medication.
Expanding Clinical Cohorts
More recent trials recruit a broader range of Stargardt patients, including those in earlier disease stages:
- Lower Disease Stage: Studies hypothesize that earlier intervention may be more beneficial, as some viable photoreceptors remain. Preliminary results show that patients with less advanced atrophy sometimes yield stronger functional improvements.
- Refined Protocols: Some investigators are testing scaffold-based RPE implants for more uniform coverage, while others refine injection parameters to minimize surgical trauma.
- Longer Follow-Up Windows: Trials now aim for multi-year data. While short-term stability offers reassurance, researchers are curious whether transplanted cells can survive and function for 5, 10, or more years. So far, two- to three-year results remain encouraging, with many patients maintaining stable vision or showing slow improvement.
Complementary Approaches and Synergies
Other investigative strategies that may complement hESC-RPE transplants include:
- Retinal Prosthetics: In advanced cases lacking sufficient photoreceptor function, “bionic eyes” or microchip implants might interface with transplanted RPE cells to amplify visual signals.
- Gene Editing or Gene Therapy: Targeting the underlying ABCA4 mutation might reduce toxic lipofuscin build-up. If combined with RPE cell renewal, these approaches could slow or even halt disease progression more effectively.
- Nutritional and Pharmacologic Support: Vitamins, antioxidants, and visual cycle modulators might give transplanted cells a better environment to thrive. Trials investigating these add-ons remain in early stages.
While no single therapy currently guarantees complete vision restoration in Stargardt disease, hESC-RPE research stands out for shifting the conversation from managing symptoms to genuinely repairing degenerating retinal tissue. The synergy between transplanting fresh RPE and preserving photoreceptors fosters optimism that broader improvements in vision may one day become attainable.
Evaluating Benefits, Safety, and Long-Term Outlook
Despite high anticipation, prospective patients and clinicians must weigh potential gains against unresolved questions about long-term performance and safety. Understanding the known advantages while realistically acknowledging limitations helps manage expectations and fosters informed decisions.
Documented Benefits
Based on published studies and ongoing clinical trials, the main advantages of hESC-RPE therapy include:
- Stabilization of Vision: For many individuals, halting or slowing progressive vision loss can be as significant as outright improvement. Even small gains or stability over several years can have enormous quality-of-life implications.
- Potential for Functional Improvement: Some patients observe modest but meaningful enhancements in visual acuity, reading speed, color perception, or contrast sensitivity. These changes may appear over months or more, reflecting slow integration of transplanted cells.
- Applicability Across Early and Mid-Stage Disease: While those with advanced atrophy may see limited benefit, trials have shown that patients with moderate Stargardt disease can experience improved outcomes when treated promptly.
- Broad Relevance: As an RPE-focused therapy, hESC-RPE transplants may benefit other diseases characterized by RPE loss, potentially fueling further innovation for conditions like AMD.
Potential Risks and Unknowns
It’s crucial to emphasize that hESC-RPE therapy is still experimental, with many aspects not fully settled:
- Rejection or Immune Reaction: Despite ocular immune privilege, transplanted cells can still provoke inflammation. Prolonged immunosuppression carries its own risks, including infection.
- Long-Term Survival of Cells: Though encouraging short-term data exist, it remains uncertain whether transplanted RPE will persist intact for a decade or more, particularly amid progressive Stargardt pathology.
- Surgical Complications: As with any intraocular surgery, there’s a low but real chance of retinal detachment, hemorrhage, or infection.
- Scalability and Consistency: Large-scale manufacturing of uniform, high-quality hESC-RPE lines is challenging. Variations in cell batches may affect outcomes.
- Ethical and Regulatory Hurdles: hESC-based treatments spark ethical debate in some regions, potentially limiting broader availability or complicating insurance coverage.
Strikingly, none of these challenges appear insurmountable. Refinements in cell lines, scaffolding materials, and immunomodulatory protocols continue to enhance reliability. Furthermore, the track record from early-phase studies suggests that catastrophic complications—like tumor formation—are exceedingly rare, thanks to improved differentiation and screening protocols.
Position in the Therapeutic Timeline
Given current trends, many experts view hESC-RPE transplantation as a potential stepping stone to more robust retina rejuvenation strategies. For patients, this therapy might be recommended at a stage when the macula is threatened but not fully lost. The future may see integrative treatments combining gene correction, neuronal rescue factors, or photoreceptor precursors alongside RPE transplants to rebuild the entire macular architecture.
Nonetheless, even as a stand-alone approach, hESC-RPE can offer new hope to individuals previously resigned to gradual, irreversible vision loss. For the motivated patient—well-informed about both the possibilities and the risks—enrolling in a clinical trial or seeking emerging protocols can open doors to transformative outcomes.
Understanding Treatment Costs
Pricing for hESC-RPE transplant procedures can vary significantly, often spanning tens of thousands of dollars per eye. These figures depend on factors such as hospital charges, surgeon fees, immunosuppressive regimens, and the specialized laboratory production of stem cell–derived grafts. Clinical trials may offset some or all costs for participants, while private treatments at specialized centers can entail out-of-pocket expenses. Given the experimental nature of hESC-RPE therapy, insurance plans often do not cover it fully, although exceptions can occur if the procedure is deemed medically necessary under research protocols. Individuals interested in this approach should explore potential financial assistance, crowdfunding, or clinical trial enrollment to manage costs effectively.
Disclaimer: This article is for educational purposes only and does not replace personalized medical advice. Always consult with a qualified healthcare provider for guidance on your specific health concerns.
We invite you to share this article on Facebook, X (formerly Twitter), or any other social media platform you prefer. By spreading the word, you can help others discover the potential of hESC-RPE transplants for Stargardt disease and other conditions affecting the retina.






