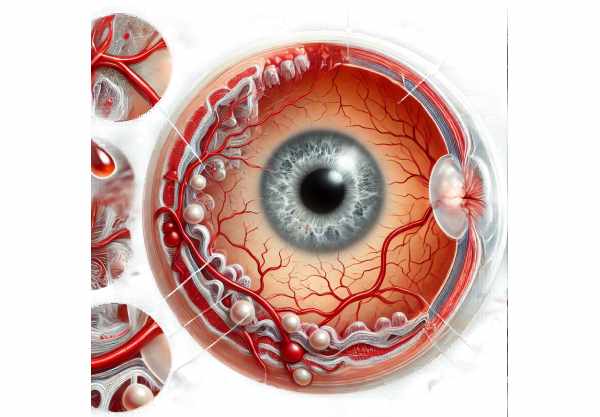
What is Corneal Neovascularization?
Corneal neovascularization is a pathological condition characterized by the formation of new blood vessels within the normally avascular cornea. This condition can be caused by a variety of factors, including chronic inflammation, infection, hypoxia (low oxygen levels), or corneal trauma. The presence of these abnormal blood vessels can reduce corneal transparency, causing vision impairment and, in severe cases, blindness. Understanding the mechanisms, causes, and effects of corneal neovascularization is critical for successful prevention, diagnosis, and treatment.
Corneal Neovascularization Detailed Examination
Corneal neovascularization occurs in response to stimuli that disrupt the cornea’s normal avascular state. The cornea retains its clarity and function despite the absence of blood vessels, relying instead on the tear film and aqueous humor for nourishment and waste removal. However, prolonged stress or injury to the cornea can cause new blood vessels to grow from the limbus.
Mechanisms of Neovascularization
The process of corneal neovascularization consists of several stages:
- Angiogenic Stimuli: The initial cause of neovascularization is frequently an insult to the corneal epithelium or stroma. This can include infections, hypoxia, mechanical trauma, and inflammatory diseases. These insults cause the release of angiogenic factors, including VEGF, FGF, and MMPs.
- Endothelial Cell Activation: Angiogenic factors cause endothelial cells in the limbal blood vessels to proliferate and migrate to the corneal tissue. These cells produce new capillary sprouts that extend into the cornea.
- Extracellular Matrix Degradation: MMPs degrade the extracellular matrix, allowing endothelial cells to invade the corneal stroma. This degradation process promotes the formation of new vascular structures.
- New Blood Vessel Formation: As endothelial cells proliferate, they form new blood vessels that are immature and leaky. These vessels mature and become more stable over time, which may result in persistent corneal neovascularization if the underlying stimulus is not addressed.
Causes and Risk Factors
- Contact Lens Wear: Prolonged or improper use of contact lenses can cause hypoxia and mechanical irritation of the cornea, which promotes neovascularization. Inadequate oxygen supply from tight-fitting lenses or poor lens hygiene can aggravate this condition.
- Inflammatory Diseases: Chronic inflammatory conditions like keratitis, scleritis, and autoimmune diseases can lead to neovascularization. Persistent inflammation alters the normal corneal environment, causing the release of angiogenic factors.
- Infections: Bacterial, viral, and fungal infections can significantly irritate and damage the cornea. Infections such as herpes simplex keratitis are particularly known for causing neovascularization.
- Trauma: Physical injuries to the cornea, such as surgical procedures and accidental trauma, can trigger the angiogenic process as part of the wound healing response.
- Hypoxia: Conditions that reduce oxygen supply to the cornea, such as severe dry eye syndrome or eyelid abnormalities that limit exposure, can promote neovascularization.
- Corneal Transplants: Graft rejection and inflammation after corneal transplantation can cause neovascularization, compromising graft survival and visual outcomes.
Symptoms and Clinical Features
Corneal neovascularization can cause a variety of symptoms and clinical signs:
- Visual Disturbances: The formation of new blood vessels in the normally clear cornea can cause blurred vision, reduced visual acuity, and, in severe cases, significant vision loss.
- Redness and Inflammation: The appearance of new blood vessels is frequently accompanied by redness and signs of inflammation, such as conjunctival injection and swelling.
- Pain and Discomfort: The inflammatory processes associated with neovascularization can cause pain, foreign body sensation, and photophobia (light sensitivity).
- Corneal Opacity: Neovascularization can cause scarring and opacification of the cornea, which impairs vision.
- Chronic Eye Irritation: Persistent neovascularization can cause chronic irritation and discomfort, reducing the patient’s quality of life.
Impact on Vision
The extent and location of the new blood vessels determine how corneal neovascularization affects vision.
- Central Neovascularization: Blood vessels that invade the central cornea can significantly impair vision by blocking the visual axis. This can cause blurry vision, glare, and halos around lights.
- Peripheral Neovascularization: While blood vessels in the peripheral cornea may not cause immediate visual disturbance, they can still deteriorate corneal health and increase the risk of recurrent inflammation and scarring.
- Recurrent Neovascularization: Chronic or recurring neovascularization can cause progressive corneal scarring and thinning, eventually jeopardizing corneal integrity and vision.
Complications
If left untreated, corneal neovascularization can cause a variety of complications:
- Corneal Scarring: Persistent inflammation and vascularization can cause scarring, reducing corneal transparency and vision.
- Corneal Ulcers: Neovascularization raises the risk of corneal ulcers, which are painful and can lead to other complications if not treated promptly.
- Secondary Glaucoma: Chronic inflammation and increased vascularization can cause elevated intraocular pressure, resulting in secondary glaucoma and possible optic nerve damage.
- Corneal Perforation: Severe neovascularization can result in corneal thinning and perforation, which is a sight-threatening emergency.
Corneal Neovascularization: Risk Reduction
- Practice Good Contact Lens Hygiene: Adhere to proper contact lens hygiene protocols, such as regular cleaning and lens replacement as recommended. Avoid wearing contact lenses overnight or for extended periods of time.
- Use Oxygen-Permeable Lenses: Choose contact lenses that allow sufficient oxygen transmission to the cornea, lowering the risk of hypoxia and neovascularization.
- Manage Inflammatory Conditions: If you have chronic inflammatory conditions like dry eye syndrome or autoimmune diseases, consult with your doctor to effectively manage them and reduce your risk of corneal complications.
- Protect Your Eyes from Trauma: Wear protective eyewear when participating in activities that increase the risk of eye injury, such as sports, construction work, or handling hazardous materials.
- Treat Infections Promptly: If you have an eye infection, seek medical attention right away to avoid inflammation and the risk of neovascularization. Adhere strictly to the prescribed treatment plans.
- Avoid Long-Term Use of Eye Medications: Certain eye medications, such as topical steroids, can raise the risk of neovascularization. Use these medications only as prescribed by your healthcare provider.
- Regular Eye Examinations: Get regular eye exams to look for early signs of corneal neovascularization, especially if you have risk factors like contact lens use or a history of ocular inflammation.
- Maintain Adequate Hydration: Drink plenty of water to promote overall eye health and keep the tear film stable. Proper hydration can lower the risk of dry eye syndrome and its complications.
- Use Artificial Tears: If you have dry eyes, use artificial tears to keep them lubricated and lower the risk of corneal irritation and neovascularization.
- Avoid Smoking: Smoking can worsen inflammation and raise the risk of neovascularization. To protect your eyes, avoid smoking and being exposed to secondhand smoke.
Methods to Diagnose Corneal Neovascularization
To accurately assess the extent and severity of corneal neovascularization, a clinical examination is combined with advanced imaging techniques. Here are the main diagnostic methods used:
- Slit Lamp Examination: The slit lamp is a necessary tool for inspecting the cornea. During this examination, an ophthalmologist uses a high-intensity light source and a microscope to get a close look at the corneal surface and the anterior segment of the eye. This enables the detection of new blood vessels, the determination of their location, and the evaluation of any associated inflammation or scarring.
- Fluorescein Angiography is an imaging technique that involves injecting fluorescein dye into the bloodstream. As the dye circulates through the eye’s blood vessels, it fluoresces under a special light, highlighting the newly formed blood vessels in the cornea. Fluorescein angiography provides detailed images of vascularization patterns, which aid in determining the extent and activity of neovascularization.
- Anterior Segment Optical Coherence Tomography (AS-OCT): AS-OCT is a non-invasive imaging technique that produces high-resolution cross-sections of the cornea and anterior segment. This technique enables detailed visualization of corneal layers, detection of new blood vessels, and measurement of corneal thickness and structural integrity. AS-OCT is especially effective for tracking changes over time and assessing treatment efficacy.
- Corneal Topography: Corneal topography maps the cornea’s surface curvature, revealing detailed information about its shape and any irregularities. This technique detects changes in corneal curvature and thickness caused by neovascularization, allowing for a better assessment of the impact on corneal structure and vision.
- Confocal Microscopy: Confocal microscopy provides in-vivo, high-resolution images of the cornea at the cellular level. This method is useful for detecting and characterizing new blood vessels, assessing the health of corneal cells, and identifying inflammatory cells linked to neovascularization.
- Ultrasound Biomicroscopy: The anterior segment, including the cornea, is imaged in detail using high-frequency ultrasound. It is particularly useful for determining the depth and extent of neovascularization, especially when the cornea is opaque or edematous.
- Tear Osmolarity Test: This test determines the concentration of solutes in the tear film, providing information about tear film stability and dry eye disease, which can lead to neovascularization. Elevated tear osmolarity is a sign of dry eye disease and can aid in determining underlying conditions that may exacerbate neovascularization.
Using these diagnostic methods, ophthalmologists can accurately diagnose corneal neovascularization, determine its severity, and devise an effective treatment plan.
Corneal Neovascularization: Treatment Methods
The treatment of corneal neovascularization aims to slow the growth of new blood vessels, alleviate symptoms, and address the underlying causes. Here are some emerging therapies, as well as standard treatment options:
Standard Treatments
- Topical Steroids: Corticosteroid eye drops are widely used to reduce inflammation and suppress the immune system. These medications help to reduce the production of angiogenic factors and control the growth of new blood vessels. However, long-term use should be closely monitored to avoid potential side effects such as increased intraocular pressure and cataract formation.
- Anti-VEGF Therapy: Anti-vascular endothelial growth factor (anti-VEGF) agents like bevacizumab (Avastin) and ranibizumab (Lucentis) are used to block the action of VEGF, a key factor in angiogenesis. These agents can be used as eye drops or intravitreal injections to reduce neovascularization and improve corneal clarity.
- Immunosuppressive Agents: If neovascularization is associated with autoimmune disease or severe inflammation, systemic immunosuppressive medications such as cyclosporine or methotrexate may be prescribed. These medications help control the underlying immune response and slow the progression of neovascularization.
- Laser Therapy: Laser photocoagulation can be used to specifically target and destroy new blood vessels in the cornea. This technique reduces neovascularization and prevents further vascular growth. Laser therapy is typically used when other treatments have proven ineffective.
Innovative and Emerging Therapies
- Gene Therapy: Research into gene therapy seeks to target specific genes involved in the angiogenic process. Gene therapy has the potential to provide long-term control of neovascularization by changing the expression of these genes, reducing the need for ongoing treatment.
- Nanoparticle-Based Drug Delivery: Advances in nanotechnology are enabling the development of nanoparticle-based drug delivery systems capable of providing targeted and sustained release of anti-angiogenic agents. These systems improve treatment efficacy and reduce side effects.
- Stem Cell Therapy: Stem cell-based therapies are under investigation for their ability to regenerate damaged corneal tissue and restore normal function. These therapies seek to replace damaged endothelial cells and improve corneal health, thereby lowering the risk of neovascularization.
- Biosynthetic Corneas: Biosynthetic corneas, made from biocompatible materials, are being researched as potential donor cornea transplant alternatives. These corneas can serve as a scaffold for new cell growth while also lowering the risk of neovascularization by preserving corneal clarity and health.
- Amniotic Membrane Transplantation: The amniotic membrane, which originates from the placenta’s innermost layer, has anti-inflammatory and anti-scarring properties. It can be used as a graft to promote healing and reduce inflammation in cases of severe neovascularisation.
- Photodynamic Therapy (PDT): PDT uses photosensitizing agents and light to selectively target and destroy neovascular tissue. This therapy has shown promise in treating ocular neovascularization while causing minimal damage to the surrounding healthy tissue.
Healthcare providers can effectively manage corneal neovascularization by combining standard treatments with innovative therapies that reduce complications and improve patient outcomes.
Trusted Resources
Books
- “Corneal Disorders: Clinical Diagnosis and Management” by Howard M. Leibowitz
- “Corneal Angiogenesis: Methods and Protocols” by Daniel S. O’Connor






