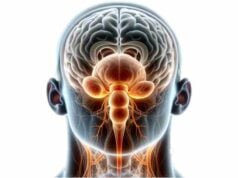
The hypothalamus is a small but powerful region at the base of the brain that serves as the master regulator of the body’s homeostasis. It controls critical functions such as hormone release, appetite, body temperature, sleep-wake cycles, and emotional responses. Despite its modest size, the hypothalamus integrates signals from the nervous and endocrine systems to orchestrate processes that affect growth, metabolism, stress response, and reproduction. Understanding the complex anatomy and physiology of the hypothalamus is essential for recognizing disorders that impact overall health. This guide explores its detailed structure, multifaceted functions, common disorders, diagnostic techniques, advanced treatment options, and lifestyle strategies to maintain optimal hypothalamic health.
Table of Contents
- Anatomical Insights & Structure
- Functional Roles & Physiological Processes
- Hormonal Regulation & Neuroendocrine Axis
- Autonomic & Behavioral Control
- Common Hypothalamic Disorders
- Diagnostic Approaches & Techniques
- Treatment Strategies & Innovations
- Nutritional Strategies & Supplements
- Lifestyle Practices for Hypothalamic Health
- Trusted Resources & Further Reading
- Frequently Asked Questions
Anatomical Insights & Structure
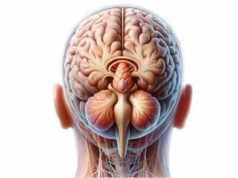
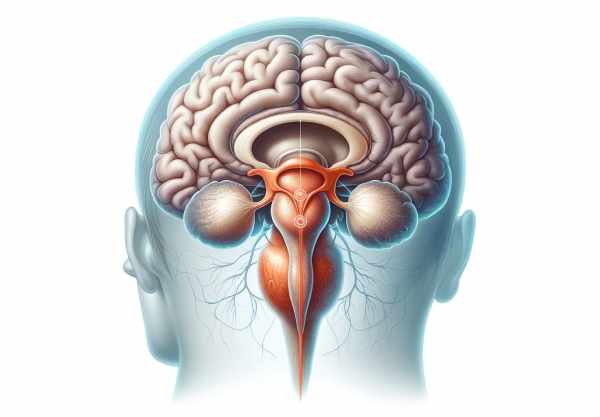
The hypothalamus is a small, highly specialized brain region located on the ventral surface of the diencephalon, forming the floor of the third ventricle. Despite its diminutive size, it comprises numerous nuclei—clusters of neurons—each dedicated to specific functions. Anatomically, the hypothalamus is organized into three regions: the anterior (supraoptic), middle (tuberal), and posterior (mammillary). Each of these regions houses distinct nuclei responsible for diverse functions ranging from hormone secretion and thermoregulation to appetite control and circadian rhythms.
Regional Organization
- Anterior Region (Supraoptic Area):
This area contains nuclei such as the paraventricular, supraoptic, and suprachiasmatic nuclei. The paraventricular nucleus produces corticotropin-releasing hormone (CRH) and oxytocin, which are crucial for stress response and reproductive functions. The supraoptic nucleus primarily secretes vasopressin, essential for water balance. The suprachiasmatic nucleus (SCN) functions as the master circadian clock, orchestrating daily physiological rhythms. - Middle Region (Tuberal Area):
The tuberal region includes the arcuate, ventromedial, and dorsomedial nuclei. The arcuate nucleus plays a pivotal role in appetite regulation, synthesizing neuropeptide Y (NPY) and proopiomelanocortin (POMC) to modulate hunger and satiety. The ventromedial nucleus acts as a satiety center, while the dorsomedial nucleus integrates various hormonal and sensory signals related to energy balance. - Posterior Region (Mammillary Area):
In the posterior region, the mammillary bodies and the posterior hypothalamic nucleus contribute to memory processing and thermoregulation. The mammillary bodies serve as relay stations for memory circuits, linking the hippocampus with the thalamus, whereas the posterior hypothalamic nucleus influences sympathetic output and heat production.
Connections and Vascular Supply
The hypothalamus is richly interconnected with other brain regions and peripheral organs. It communicates with the pituitary gland via the hypophyseal portal system, which is fundamental for hormonal regulation. Its vascular supply is derived from branches of the circle of Willis—including the anterior cerebral, posterior cerebral, and communicating arteries—ensuring that this critical region receives a continuous supply of oxygen and nutrients.
Histological Organization
The hypothalamus is composed of various neuronal and glial cell types arranged into nuclei and fiber tracts. Its complex microarchitecture enables it to integrate diverse signals from the internal and external environments, setting the stage for its multifaceted regulatory roles.
Functional Roles & Physiological Processes
The hypothalamus is at the core of homeostatic regulation, coordinating a broad spectrum of physiological processes through its neural and hormonal outputs. Its functions extend from basic survival mechanisms to complex behavioral responses.
Endocrine Regulation
- Hypothalamic-Pituitary Axis:
The hypothalamus controls the endocrine system by releasing hormones that either stimulate or inhibit the secretion of pituitary hormones. This axis regulates growth, metabolism, reproduction, and stress responses. For example, corticotropin-releasing hormone (CRH) from the paraventricular nucleus stimulates the release of adrenocorticotropic hormone (ACTH) from the anterior pituitary, which in turn stimulates cortisol production from the adrenal glands. - Direct Hormonal Secretion:
In addition to its influence on the anterior pituitary, the hypothalamus directly secretes hormones like vasopressin and oxytocin via the posterior pituitary. Vasopressin plays a key role in water conservation and blood pressure regulation, while oxytocin is essential for social bonding, lactation, and uterine contractions.
Autonomic and Behavioral Control
- Autonomic Nervous System (ANS) Regulation:
The hypothalamus is a central regulator of the ANS, balancing sympathetic and parasympathetic outputs to maintain physiological stability. It modulates heart rate, blood pressure, and digestion, responding dynamically to internal and external stressors. - Emotional and Behavioral Responses:
By interacting with the limbic system, the hypothalamus influences emotional behavior and stress responses. It plays a role in mood regulation, aggression, and reproductive behaviors through its control over hormone secretion and autonomic function.
Thermoregulation and Energy Balance
- Temperature Control:
The preoptic area of the hypothalamus houses thermosensitive neurons that detect changes in blood temperature. Depending on these signals, the hypothalamus initiates responses such as sweating, shivering, or altering blood vessel diameter to maintain a stable core temperature. - Appetite and Metabolic Regulation:
The hypothalamus integrates signals from the digestive system, adipose tissue, and blood glucose levels to regulate appetite and energy expenditure. Neuropeptides like NPY and POMC, produced in the arcuate nucleus, work together to control hunger and satiety, thus influencing body weight and metabolic homeostasis.
Water and Electrolyte Homeostasis
- Osmoregulation:
Through the secretion of vasopressin, the hypothalamus monitors and regulates water balance and osmolarity. When blood osmolarity increases, vasopressin release prompts the kidneys to conserve water, thereby maintaining fluid balance and blood pressure.
Circadian Rhythms and Sleep
- Master Clock Function:
The suprachiasmatic nucleus (SCN) of the hypothalamus is the primary regulator of circadian rhythms, synchronizing the body’s internal clock with the external light-dark cycle. This coordination influences sleep patterns, hormonal secretion, body temperature, and other physiological processes. - Sleep-Wake Cycle:
By regulating the production of melatonin through its influence on the pineal gland, the SCN plays a crucial role in determining sleep onset and duration, thereby ensuring restorative sleep.
Through these diverse roles—ranging from hormonal regulation and autonomic control to thermoregulation and circadian rhythm maintenance—the hypothalamus orchestrates the body’s internal environment, ensuring survival and optimal functioning.
Hormonal Regulation & Neuroendocrine Axis
The hypothalamus is the control center of the endocrine system, exerting its influence via the hypothalamic-pituitary axis. It produces a variety of releasing and inhibiting hormones that regulate the secretion of key hormones from the pituitary gland, which in turn affects numerous bodily functions.
Releasing and Inhibiting Hormones
- Corticotropin-Releasing Hormone (CRH):
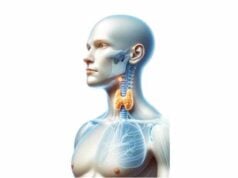
Produced in the paraventricular nucleus, CRH stimulates the anterior pituitary to release ACTH, which triggers cortisol production in the adrenal glands—essential for stress responses. - Thyrotropin-Releasing Hormone (TRH):
TRH regulates the release of thyroid-stimulating hormone (TSH) from the pituitary, influencing metabolic rate and energy balance. - Gonadotropin-Releasing Hormone (GnRH):
GnRH is crucial for reproductive function, stimulating the release of LH and follicle-stimulating hormone (FSH), which govern reproductive processes in both men and women. - Growth Hormone-Releasing Hormone (GHRH) and Somatostatin:
These hormones regulate growth hormone release, influencing growth, metabolism, and body composition.
Direct Hormonal Outputs
- Vasopressin (Antidiuretic Hormone):
Produced in the supraoptic and paraventricular nuclei and released via the posterior pituitary, vasopressin plays a key role in water balance, kidney function, and blood pressure regulation. - Oxytocin:
Also released via the posterior pituitary, oxytocin is essential for reproductive functions such as uterine contractions during labor and milk ejection during breastfeeding, as well as for social bonding.
Integration with the Pituitary Gland
The hypothalamus communicates with the pituitary gland through the hypophyseal portal system, a specialized network of blood vessels that ensures rapid transport of releasing and inhibiting hormones. This direct link allows the hypothalamus to precisely control the output of pituitary hormones, orchestrating a coordinated response to internal and external stimuli.
Neuroendocrine Feedback Loops
Feedback mechanisms are crucial for maintaining hormonal balance. Elevated levels of target hormones (e.g., cortisol or thyroid hormones) typically exert negative feedback on the hypothalamus and pituitary gland, reducing the release of stimulating hormones. This finely tuned regulatory system ensures that hormone levels remain within a narrow, optimal range.
The hypothalamic-pituitary axis is fundamental to regulating numerous physiological processes, making it a critical focus for understanding and treating endocrine disorders.
Autonomic & Behavioral Control
The hypothalamus not only manages hormonal output but also plays a central role in controlling the autonomic nervous system (ANS), which governs involuntary bodily functions. Its influence on the ANS ensures that the body can adapt rapidly to stress, maintain homeostasis, and respond to environmental changes.
Autonomic Nervous System Regulation
- Sympathetic Activation:
In response to stress or danger, the hypothalamus stimulates the sympathetic nervous system. This activation leads to increased heart rate, blood pressure, and the release of adrenaline, preparing the body for a “fight or flight” response. - Parasympathetic Modulation:
Conversely, the hypothalamus promotes parasympathetic activity during restful states. This modulation slows the heart rate, enhances digestion, and conserves energy, supporting restorative processes.
Behavioral and Emotional Control
- Stress Response and Mood Regulation:
Through its interaction with the limbic system, the hypothalamus influences emotional responses, mood, and behavior. The hypothalamic-pituitary-adrenal (HPA) axis plays a critical role in the body’s response to stress by regulating cortisol levels, which affect mood, immune function, and energy metabolism. - Sleep-Wake Cycles:
The suprachiasmatic nucleus (SCN) in the hypothalamus acts as the master circadian clock, synchronizing the sleep-wake cycle with environmental cues such as light. Proper regulation of sleep is essential for overall health and well-being. - Reproductive Behavior:
The hypothalamus influences reproductive behaviors through its regulation of gonadotropin-releasing hormone (GnRH) and interactions with the limbic system. This coordination affects sexual behavior, fertility, and parental bonding.
Integration of Sensory Input
The hypothalamus receives diverse sensory inputs, such as light intensity, temperature, and even emotional stimuli. This information is integrated and used to adjust autonomic and endocrine responses accordingly, ensuring that the body’s internal environment is finely tuned to meet external challenges.
By managing the autonomic nervous system and modulating behavior and emotions, the hypothalamus plays a pivotal role in ensuring that the body responds appropriately to both physiological and psychological stressors.
Common Hypothalamic Disorders
The hypothalamus is vulnerable to a range of disorders that can disrupt its regulatory functions, affecting numerous bodily systems. Early identification and treatment of these conditions are vital for preserving overall health.
Hypothalamic Dysfunction
- Overview:
Hypothalamic dysfunction can result from trauma, tumors, infections, or genetic conditions. Disruption in hypothalamic function can lead to abnormalities in temperature regulation, appetite, sleep patterns, and hormonal secretion. - Symptoms:
Symptoms may include erratic body temperature, irregular appetite or weight changes, sleep disturbances, and hormonal imbalances. - Management:
Treatment depends on the underlying cause and may involve hormone replacement, surgical intervention, or supportive therapies.
Hypothalamic Obesity
- Etiology:
Hypothalamic obesity occurs when damage to the hypothalamic regions that control satiety and energy expenditure—often due to surgery, trauma, or congenital defects—leads to uncontrollable weight gain. - Clinical Manifestations:
Patients typically experience rapid weight gain, hyperphagia (excessive eating), and resistance to conventional weight-loss strategies. - Treatment Strategies:
Management includes lifestyle modifications, dietary interventions, pharmacotherapy to regulate appetite, and in some cases, bariatric procedures.
Diabetes Insipidus
- Pathophysiology:
Diabetes insipidus is characterized by an inability to concentrate urine due to a deficiency of vasopressin (antidiuretic hormone) or kidney resistance to it. The central form arises from hypothalamic or pituitary dysfunction. - Symptoms:
Key symptoms include excessive urination (polyuria) and extreme thirst (polydipsia). - Management:
Central diabetes insipidus is commonly treated with desmopressin, a synthetic vasopressin analogue, while nephrogenic diabetes insipidus is managed by addressing the underlying cause and adjusting fluid intake.
Hypopituitarism
- Overview:
Hypopituitarism results from insufficient hormone production by the pituitary gland, often secondary to hypothalamic dysfunction. This condition can lead to deficiencies in growth hormone, thyroid-stimulating hormone, and gonadotropins. - Symptoms and Treatment:
Symptoms vary widely and may include fatigue, growth retardation, and reproductive issues. Hormone replacement therapy is typically required to restore hormonal balance.
Kallmann Syndrome
- Definition:
Kallmann syndrome is a genetic disorder marked by GnRH deficiency, resulting in delayed or absent puberty and an impaired sense of smell. - Mechanism and Management:
The syndrome arises from mutations that disrupt the development or migration of GnRH neurons. Treatment involves hormone replacement therapy to induce and maintain puberty and secondary sexual characteristics.
Hypothalamic Hamartomas
- Characteristics:
These benign tumors, often present from birth, can interfere with hypothalamic functions. They are associated with precocious puberty, gelastic seizures (inappropriate laughter), and cognitive or behavioral challenges. - Diagnosis and Treatment:
Diagnosis is made through imaging, particularly MRI. Treatment options include surgical removal, radiation therapy, and medication to manage seizures and hormonal imbalances.
Understanding these hypothalamic disorders is crucial for early diagnosis and targeted treatment, as disruptions in hypothalamic function can have widespread effects on the body.
Diagnostic Approaches & Evaluation Methods
A comprehensive evaluation of hypothalamic function involves a combination of clinical assessments, imaging studies, laboratory tests, and specialized procedures. These diagnostic approaches help pinpoint the source of dysfunction and guide appropriate interventions.
Clinical Assessment
- Medical History and Symptom Evaluation:
A detailed history that includes questions about appetite changes, sleep disturbances, weight fluctuations, and temperature regulation is essential. Physicians also assess symptoms related to hormonal imbalances and behavioral changes. - Physical Examination:
A thorough physical exam evaluates signs such as abnormal growth patterns, obesity, and changes in vital signs. Neurological and endocrine assessments are also performed to gauge overall hypothalamic function.
Imaging Techniques
- Magnetic Resonance Imaging (MRI):
MRI is the gold standard for visualizing the hypothalamus and surrounding brain structures. It provides high-resolution images that can detect tumors, lesions, or congenital abnormalities. - Computed Tomography (CT) Scan:
CT scans offer rapid imaging and are useful in emergency settings to assess acute trauma or hemorrhage involving the hypothalamic region. - Functional MRI (fMRI):
fMRI measures changes in blood flow to assess functional activity in the hypothalamus, particularly in research settings focused on behavioral and emotional responses.
Laboratory Tests
- Hormonal Assays:
Blood tests measuring levels of hormones such as cortisol, TSH, ACTH, and gonadotropins provide insights into hypothalamic-pituitary axis function. - Electrolyte and Osmolality Measurements:
These tests assess water balance and can help diagnose conditions like diabetes insipidus by evaluating serum sodium and osmolality. - Genetic Testing:
For congenital disorders such as Kallmann syndrome, genetic testing identifies mutations that affect the development or migration of GnRH neurons.
Specialized Functional Tests
- Water Deprivation Test:
Used to diagnose diabetes insipidus, this test evaluates the kidney’s ability to concentrate urine in response to fluid deprivation. The response to administered vasopressin helps differentiate between central and nephrogenic diabetes insipidus. - Dynamic Endocrine Testing:
Tests like the insulin tolerance test (ITT) assess the function of the HPA axis by monitoring the hormonal response to induced hypoglycemia. - Polysomnography:
For patients with sleep disturbances, sleep studies measure various physiological parameters during sleep, helping to detect abnormalities linked to hypothalamic dysfunction.
These diagnostic methods collectively enable a thorough evaluation of hypothalamic structure and function, leading to accurate diagnosis and tailored treatment strategies.
Treatment Strategies & Therapeutic Interventions
Effective management of hypothalamic disorders involves addressing the underlying cause, managing symptoms, and restoring hormonal balance. Treatments range from hormone replacement therapy and medications to surgical interventions and innovative therapies.
Hormone Replacement Therapy
- Vasopressin Analogues:
In cases of central diabetes insipidus, synthetic vasopressin (desmopressin) is used to replace the deficient hormone, reducing excessive urination and thirst. - Corticosteroids:
For patients with secondary adrenal insufficiency resulting from hypothalamic dysfunction, corticosteroid replacement therapy restores normal cortisol levels. - Thyroid Hormone Replacement:
When hypothalamic dysfunction leads to insufficient stimulation of the thyroid gland, levothyroxine therapy is implemented to normalize thyroid hormone levels. - Gonadal Steroids:
Hormone replacement for deficiencies in gonadotropin secretion may involve testosterone, estrogen, or progesterone, particularly in conditions like Kallmann syndrome or hypopituitarism.
Surgical Interventions
- Tumor Resection:
Surgical removal of hypothalamic tumors (e.g., hamartomas, craniopharyngiomas) can alleviate symptoms and restore normal function. Given the proximity of the hypothalamus to critical structures, such surgeries require meticulous planning. - Endoscopic Procedures:
Minimally invasive endoscopic techniques allow for targeted biopsy or resection of hypothalamic lesions, reducing recovery time and surgical risk.
Medications and Supportive Therapies
- Appetite Modulators:
For hypothalamic obesity, medications that regulate appetite and energy expenditure, such as metformin or GLP-1 receptor agonists, are used to control weight gain. - Antiepileptic Drugs:
In patients with hypothalamic hamartomas experiencing gelastic seizures, antiepileptic medications help control seizure activity. - Antidepressants and Anxiolytics:
Medications that regulate serotonin and norepinephrine levels can alleviate mood disorders associated with hypothalamic dysfunction. - Behavioral Therapy:
Psychological support and cognitive-behavioral therapy (CBT) help patients manage the emotional and behavioral consequences of chronic hypothalamic disorders.
Innovative and Experimental Treatments
- Deep Brain Stimulation (DBS):
DBS is being explored as a treatment for refractory hypothalamic obesity and certain seizure disorders. It involves implanting electrodes to modulate neural activity in the hypothalamus. - Gene Therapy:
Experimental gene therapies target genetic mutations that affect hypothalamic development and function, aiming to correct underlying defects. - Stem Cell Therapy:
Investigational stem cell therapies offer the potential to regenerate damaged hypothalamic tissue, which may restore hormonal regulation and improve overall function.
Tailoring treatment strategies to individual needs is crucial for managing hypothalamic disorders. A combination of hormone replacement, surgical intervention, medications, and innovative therapies often yields the best outcomes.
Nutritional Strategies & Supplements for Hypothalamic Health
Proper nutrition is essential for supporting brain function and maintaining the health of the hypothalamus. A balanced diet enriched with key nutrients and targeted supplements can help optimize hypothalamic function, reduce inflammation, and promote overall hormonal balance.
Essential Nutrients
- Omega-3 Fatty Acids:
Found in fatty fish, flaxseed, and walnuts, omega-3 fatty acids support neuronal health and reduce inflammation, which benefits the hypothalamus and overall brain function. - Vitamin D:
Adequate vitamin D levels are associated with improved mood and cognitive function. Supplementing with vitamin D can help support hypothalamic regulation of hormones and immune responses. - Magnesium:
Magnesium plays a critical role in neurotransmitter regulation and stress response. It helps improve sleep quality and reduces anxiety, which supports the proper functioning of the hypothalamus. - Vitamin B Complex:
B-vitamins, particularly B6, B9 (folate), and B12, are essential for energy production and neurological function. They support neurotransmitter synthesis and help maintain the integrity of the nervous system.
Herbal and Natural Supplements
- Ashwagandha:
This adaptogenic herb helps reduce stress and strengthen the hypothalamic-pituitary-adrenal (HPA) axis, promoting hormonal balance and resilience against stress. - Curcumin:
The active compound in turmeric, curcumin has potent anti-inflammatory and antioxidant properties. It may protect neural tissue in the hypothalamus and enhance cognitive function. - Phosphatidylserine:
A phospholipid essential for maintaining cell membrane integrity, phosphatidylserine supports cognitive function and can help improve memory and mood, indirectly benefiting hypothalamic function.
Antioxidant Support
- N-Acetylcysteine (NAC):
NAC enhances the production of glutathione, a major antioxidant that protects brain cells from oxidative stress, supporting healthy hypothalamic function. - Coenzyme Q10 (CoQ10):
CoQ10 is vital for energy production in neurons and acts as an antioxidant. Supplementing with CoQ10 may improve overall brain health and resilience.
These nutritional strategies and supplements help create an optimal environment for the hypothalamus, supporting its crucial role in maintaining homeostasis and regulating the endocrine and autonomic nervous systems.
Lifestyle Practices for Hypothalamic Health
A holistic approach to maintaining hypothalamic health involves not only proper nutrition and medical care but also adopting lifestyle practices that reduce stress and promote overall well-being. The following practices can help support hypothalamic function and maintain homeostasis.
Stress Management
- Mindfulness and Meditation:
Regular mindfulness practices and meditation can significantly reduce stress levels, thereby lessening the strain on the hypothalamic-pituitary-adrenal (HPA) axis. This improves hormonal balance and emotional regulation. - Yoga and Tai Chi:
These gentle exercises promote relaxation, improve body awareness, and help regulate the autonomic nervous system, contributing to overall hypothalamic health.
Sleep Hygiene
- Regular Sleep Schedule:
Consistent sleep patterns are critical for maintaining circadian rhythms, which are regulated by the hypothalamus. Aim for 7–9 hours of quality sleep each night. - Optimize Your Sleep Environment:
Keep your bedroom cool, dark, and quiet to support deep, restorative sleep, allowing the hypothalamus to regulate body temperature and hormonal cycles effectively.
Physical Activity
- Regular Exercise:
Engaging in moderate aerobic exercise enhances blood flow to the brain, promotes neurogenesis, and helps manage stress, all of which support healthy hypothalamic function. - Balanced Workouts:
Include a mix of cardio, strength training, and flexibility exercises to maintain overall physical and mental health.
Dietary Habits
- Balanced Diet:
A diet rich in whole foods—fruits, vegetables, lean proteins, and whole grains—provides the essential nutrients required for optimal brain function. - Hydration:
Adequate water intake is essential for maintaining cellular function and supporting the hypothalamus in regulating body temperature and metabolism.
Weight and Metabolic Health
- Maintain a Healthy Weight:
Avoid rapid weight loss or gain, as fluctuations can stress the hypothalamus and disrupt hormonal regulation. - Monitor Blood Sugar Levels:
Balanced blood sugar levels support overall brain health and help maintain proper hypothalamic control over metabolism.
Avoiding Harmful Substances
- Limit Alcohol and Drug Use:
Excessive alcohol consumption and illicit drugs can impair hypothalamic function and disrupt hormonal balance. Moderation and avoidance are key. - Quit Smoking:
Smoking negatively affects blood flow and increases oxidative stress, both of which can impair hypothalamic and overall brain function.
Social Engagement and Mental Health
- Stay Socially Active:
Social interactions stimulate brain function and can improve mood, which supports the hypothalamus in regulating emotional responses. - Seek Professional Help When Needed:
If you experience chronic stress, depression, or anxiety, professional counseling or therapy can help manage these conditions and reduce their impact on hypothalamic health.
By adopting these lifestyle practices, you can create a supportive environment for the hypothalamus, enhancing its ability to regulate essential functions and maintain overall homeostasis.
Trusted Resources & Further Reading
Staying informed about hypothalamic health and function is essential for both individuals and healthcare professionals. The following resources provide in-depth information, the latest research, and practical strategies for supporting hypothalamic function.
Recommended Books
- “The Body Keeps the Score” by Bessel van der Kolk:
Explores how stress and trauma affect brain structures, including the hypothalamus, and offers insights into healing and recovery. - “Brain Body Diet” by Sara Gottfried:
Focuses on hormonal balance and how diet can influence brain function, including the regulation of the hypothalamus. - “Spark: The Revolutionary New Science of Exercise and the Brain” by John J. Ratey:
Examines the impact of physical activity on brain health, including the roles of stress, mood, and neurogenesis in hypothalamic function.
Academic Journals
- Journal of Neuroendocrinology:
Publishes cutting-edge research on the interactions between the nervous and endocrine systems, focusing on hypothalamic regulation and hormonal balance. - Endocrinology:
Offers comprehensive studies on hormonal regulation and the role of the hypothalamus in maintaining overall endocrine function.
Mobile Apps
- Headspace:
A meditation and mindfulness app that can help reduce stress and support mental well-being, indirectly benefiting hypothalamic function. - MyFitnessPal:
A diet and exercise tracking app that helps maintain a balanced lifestyle and healthy weight, essential for optimal hypothalamic regulation. - Sleep Cycle:
An app designed to monitor sleep patterns and improve sleep quality, aiding the hypothalamus in regulating circadian rhythms and hormonal balance.
These trusted resources provide valuable information and practical tools to help you understand, monitor, and optimize hypothalamic function, supporting overall health and well-being.
Frequently Asked Questions About the Hypothalamus
What is the primary function of the hypothalamus?
The hypothalamus is the master regulator of the body’s homeostasis, controlling hormone release, appetite, body temperature, sleep-wake cycles, and stress responses through its interactions with the endocrine and autonomic nervous systems.
How does the hypothalamus regulate hormones?
The hypothalamus produces releasing and inhibiting hormones that travel to the pituitary gland via the hypophyseal portal system, controlling the secretion of various hormones that regulate growth, metabolism, reproduction, and stress responses.
What role does the hypothalamus play in thermoregulation?
The hypothalamus contains thermosensitive neurons that monitor blood temperature. It triggers responses such as sweating, shivering, and vasodilation or vasoconstriction to maintain a stable core body temperature.
How does hypothalamic dysfunction affect health?
Dysfunction of the hypothalamus can lead to hormonal imbalances, abnormal appetite, disrupted circadian rhythms, and impaired stress responses, resulting in conditions like obesity, diabetes insipidus, and mood disorders.
What lifestyle changes can support hypothalamic health?
A healthy diet, regular exercise, adequate sleep, stress management through mindfulness or meditation, and avoiding harmful substances like excessive alcohol and tobacco can help maintain proper hypothalamic function and overall brain health.
Disclaimer:
The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a healthcare provider for personalized guidance.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about hypothalamic health and overall wellness.