Retinitis Pigmentosa (RP) is a collection of hereditary retinal disorders characterized by the gradual loss of photoreceptor cells, often beginning with rod cells and eventually impacting cone cells responsible for central, high-acuity, and color vision. As the disease progresses, individuals typically experience symptoms like night blindness, peripheral vision loss, and difficulties with contrast sensitivity. Over time, these symptoms can become debilitating, significantly affecting daily life and overall well-being. The pursuit of innovative strategies to slow, halt, or even reverse such retinal degeneration is at the forefront of ophthalmic research. A promising new avenue focuses on cell-based therapies designed to preserve cone function and maintain light sensitivity, thereby sustaining valuable aspects of sight.
InGel Cell Therapy has emerged in this dynamic landscape as a novel approach aimed at protecting and revitalizing cone cells within the diseased retina. Drawing on advances in regenerative medicine, InGel therapy employs specialized cells embedded in a supportive matrix that can integrate with damaged retinal tissue. By delivering growth factors and offering structural support to existing cones, this therapy seeks to forestall further degeneration while enhancing the overall health of surviving photoreceptors. Researchers and clinicians alike are optimistic about its potential, noting early evidence suggesting improved light perception and extended cone viability in patients. Through a blend of precise cellular engineering, cutting-edge delivery systems, and specialized aftercare protocols, InGel Cell Therapy holds strong promise for shaping the future of RP treatment and preserving vision for those who need it most.
Exploring the Science and Potential of InGel Cell Therapy
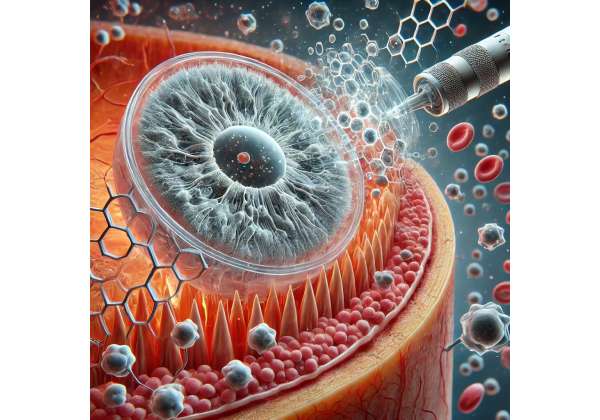
InGel Cell Therapy represents a sophisticated intervention targeting the degenerative processes characteristic of Retinitis Pigmentosa. At the core of this approach is the idea that damaged or dysfunctional cone cells can be supported by introducing new, healthy cells into the retina—often stem cells or progenitor cells—encapsulated in a specially designed gel matrix. This gel-like scaffold offers multiple advantages, including improved cell survival rates, optimized nutrient delivery, and localized growth factor release.
Researchers have discovered that an optimal microenvironment can help combat the hostile conditions caused by inflammation, oxidative stress, and abnormal protein accumulation in RP. Within the retina, chronic inflammation and the gradual breakdown of supportive structures compromise cone cells, making them susceptible to degeneration. With InGel Cell Therapy, these engineered or lab-grown cells come armed with protective signals that can mitigate the negative stimuli contributing to photoreceptor loss. Additionally, the gel itself, designed from biocompatible materials, helps protect transplanted cells from immune attack and local stressors, effectively bolstering their survival.
How InGel Therapy Targets Cone Preservation
Traditional strategies for addressing RP often focus on general photoreceptor protection, but the advanced stages of the disease leave patients with predominantly cone photoreceptors—critical for reading, face recognition, and color discrimination. This therapy concentrates its mechanisms on stabilizing and safeguarding these remaining cone cells. By secreting supportive growth factors, the transplanted cells in the gel matrix can promote synaptic repair and potentially even guide the formation of new connections within the retinal network.
Moreover, InGel Cell Therapy aligns with the push towards personalized medicine. Each patient’s disease can manifest in varying severity, and the therapy can be adapted by calibrating the types of cells delivered or modifying the gel composition. Early lab results suggest that this adaptability can address individual patient profiles more effectively than generic treatments. When integrated into a well-rounded RP management plan, including nutritional guidance, pharmacological agents, and assistive visual devices, InGel therapy could play a central role in prolonging useful vision.
Advancing the Science Through Collaborative Research
This innovative approach is backed by an ever-growing body of preclinical and clinical research. Multidisciplinary teams—comprising ophthalmologists, cell biologists, materials scientists, and biomedical engineers—collaborate to refine both the biological aspects of the therapy and the mechanisms of its delivery. Animal models have provided the proof-of-concept necessary for further exploration, demonstrating that cell-seeded gels remain stable in the subretinal space and confer measurable benefits in photoreceptor preservation. As the therapy continues to progress toward larger human trials, ongoing studies are broadening our understanding of optimal dosing, patient selection criteria, and long-term safety.
Although the therapy remains in its relatively early stages, experts are increasingly optimistic about its potential. The emphasis on preserving cone function aligns closely with patient needs, as these cells govern the tasks most crucial for day-to-day life. Furthermore, advances in gene editing and stem cell biology could synergize with InGel therapies, offering possibilities such as gene-corrected cells embedded in biodegradable gels for targeted restoration of damaged regions.
Why the Future Looks Promising
While no single therapy can claim to cure RP outright, InGel Cell Therapy provides a meaningful step forward for a condition long considered intractable. By proactively supporting cone cells, individuals might retain clearer central vision and color discrimination for longer, improving quality of life. The synergy between cell-based interventions and ongoing developments in gene therapy, pharmacology, and visual prosthetics suggests that integrated treatment plans may soon offer more profound benefits than any standalone intervention. For individuals grappling with the persistent loss of sight from RP, a therapy designed explicitly for cone preservation represents a critical addition to the treatment repertoire, embodying the progress made in regenerative ophthalmology.
Practical Approaches and Detailed Treatment Methods
When it comes to delivering InGel Cell Therapy to individuals with Retinitis Pigmentosa, a disciplined and carefully planned protocol is essential to maximize therapeutic efficacy and safety. Each step in the process—from the assessment of disease progression to the postoperative care regimen—plays a crucial role in ensuring that the cone cells receive optimal support for function preservation.
Initial Patient Assessment and Diagnostics
Before recommending any form of InGel therapy, an ophthalmologist conducts an in-depth evaluation of a patient’s retinal health. Standard tests include fundus examinations, optical coherence tomography (OCT), and electroretinography (ERG). These diagnostic tools provide insight into how well photoreceptors (including cones) are functioning and help identify the stage of RP. Clinicians also evaluate the patient’s medical history to rule out contraindications that might interfere with transplant acceptance or elevate procedural risks.
In this phase, it is also common to discuss potential outcomes and set realistic expectations. While many patients hope for improvements in visual acuity, physicians often emphasize the therapy’s principal goal: slowing or halting the ongoing loss of cone cells and, in some cases, modestly improving existing visual function. By clearly articulating the intended benefits and the limitations, clinicians help patients make informed decisions regarding the therapy.
Creating the Personalized Treatment Plan
Once a patient qualifies for InGel Cell Therapy, the medical team devises a personalized plan. Two key components stand out in this phase:
- Cell Sourcing and Preparation:
- The cells utilized in InGel therapy may be adult stem cells, induced pluripotent stem cells (iPSCs), or other specialized progenitor cells capable of sustaining cone photoreceptors.
- These cells must undergo rigorous quality checks to ensure purity, viability, and safety. Often, they are cultured in a laboratory setting specifically for implantation, sometimes requiring weeks of preparation to ensure the cells are fully functional and free from contaminants.
- In certain protocols, autologous cells—derived from the patient’s own tissue—reduce the risk of immune rejection. Alternatively, donor cells, thoroughly matched and screened, can be employed if the autologous supply is insufficient.
- The Gel Matrix Formulation:
- The gel acts as both a protective scaffold and a delivery mechanism for growth factors. The composition typically incorporates biodegradable polymers that break down over time, leaving minimal residue and promoting healthy tissue integration.
- Researchers continually modify gel formulations to optimize oxygen and nutrient diffusion while maintaining sufficient structural integrity to anchor the cells in the subretinal space.
- Growth factors, cytokines, and other supportive molecules may be blended into the gel. These elements help sustain transplanted cells while simultaneously delivering protective signals to the existing cone cells.
Surgical Delivery and Procedure Steps
Delivering InGel therapy involves a delicate surgical procedure performed under sterile conditions, often in a specialized ophthalmic surgery suite. While the specific techniques may vary among treatment centers, the general steps typically include:
- Anesthesia and Preparation:
- Local anesthesia is commonly used to ensure patient comfort during surgery.
- The ophthalmologist or surgeon carefully sterilizes and drapes the operative area, focusing on the region around the eye to minimize the risk of infection.
- Incision and Access:
- A tiny incision is made in the sclera (the white part of the eye), providing access to the subretinal space.
- Microscopic instruments and advanced surgical visualization techniques, such as intraoperative OCT, help the surgeon navigate the delicate retinal layers.
- InGel Material Injection:
- The prepared cell-laden gel is gently injected into the subretinal area where cone cells are most affected. Because the therapy is site-specific, precise placement is vital to maximize contact between transplanted and native cells.
- Once injected, the gel expands slightly, forming a thin layer that envelops the existing retinal tissue. This ensures the transplanted cells maintain close proximity to the cone photoreceptors and can release growth factors effectively.
- Closure and Immediate Aftercare:
- The incision is sealed, typically with fine sutures if needed, or self-sealing microincisions.
- After the operation, the medical team monitors intraocular pressure and checks for any immediate complications.
- Patients may be advised to remain in a specific head position for a short period to optimize the gel’s placement and reduce the chance of displacement.
Postoperative Management and Follow-Up
A well-defined follow-up schedule is crucial for safeguarding both the transplanted cells and the native cone population. Within days of the procedure, patients return for thorough evaluations, which generally include:
- Visual Assessments: Tests to measure changes in visual acuity, color perception, and visual fields over time.
- Imaging: OCT remains the gold standard for tracking any improvement in photoreceptor structure, as well as monitoring for complications like fluid accumulation or inflammation.
- Medical Therapies: To enhance compatibility and reduce immune responses, clinicians may prescribe anti-inflammatory medications, often in the form of eye drops or oral drugs, for a set period. In some cases, mild immunosuppressants are used to protect transplanted cells.
- Lifestyle Recommendations: Patients are generally advised to avoid strenuous activities and protect their eyes from direct trauma or bright light during the initial recovery period. Foods rich in antioxidants and Omega-3 fatty acids, as well as vitamin supplementation, may further support eye health.
Postoperative care extends over the long term, not only to track the effectiveness of the therapy but also to respond promptly to any changes in visual function. Because RP is progressive, even a partially successful therapy can translate into meaningful quality-of-life improvements. InGel Cell Therapy aims to complement other interventions—gene therapy, pharmacological treatments, or low-vision aids—thus integrating seamlessly into a multifaceted management plan for Retinitis Pigmentosa.
Emerging Clinical Evidence and Ongoing Research Initiatives
As with any cutting-edge therapy, the success of InGel Cell Therapy for Retinitis Pigmentosa hinges on rigorous research and the collaborative efforts of multiple scientific and clinical disciplines. While the therapy is in an advanced investigative phase, a wealth of encouraging data has begun to shape a more complete understanding of its safety profile, potential benefits, and long-term viability.
Key Preclinical Findings
Researchers have conducted extensive animal studies—often using rodent models genetically engineered to mimic human Retinitis Pigmentosa—to demonstrate the feasibility and benefits of InGel therapy. These studies reveal several core findings:
- Enhanced Cone Survival: In animals treated with cell-laden gels, the rate of cone photoreceptor loss appears significantly slower compared to control groups. Histological examinations show that transplanted cells remain viable in the subretinal space, forming tight connections with the host tissue.
- Function Preservation: Functional tests, such as electroretinograms, indicate that treated subjects retain stronger cone responses. This implies that the intervention does more than just keep cones structurally intact; it preserves aspects of their functional capacity.
- Reduced Inflammatory Markers: Tissue analyses in animal models often reveal reduced markers of inflammation and cell stress in treated areas, suggesting that the therapeutic gel provides a localized anti-inflammatory effect conducive to photoreceptor health.
This preclinical evidence forms the backbone of the therapy’s rationale, supporting the translation of these findings into human clinical trials.
Early Clinical Trials and Observational Studies
Several early-phase clinical trials have been or are currently being conducted in specialized ophthalmology centers worldwide. These studies generally aim to:
- Evaluate Safety: Tracking adverse events or any harmful immune responses that might arise after injecting a foreign material into the subretinal space. Initial reports are favorable, with few serious complications and minimal indications of rejection or severe inflammation.
- Determine Optimal Dosing: Researchers test different concentrations of cells and different gel volumes to pinpoint the combination that confers maximum cone protection with minimal risks.
- Measure Functional Outcomes: Patients undergo an array of tests—visual acuity exams, visual field assessments, and advanced imaging—to gauge improvements in contrast sensitivity, reading speed, or color perception.
Though results are preliminary, some participants have experienced noticeable stabilization of their central vision, while others report subtle but meaningful enhancements in low-light and color discrimination. Not all subjects show dramatic improvements, but the slowing or halting of disease progression itself stands as a substantial achievement for many patients otherwise expecting continual vision decline.
Ongoing Research Directions
The evolving nature of regenerative medicine ensures that InGel Cell Therapy remains an active area of exploration. Key avenues of investigation include:
- Gene-Modified Cells: Scientists are experimenting with genetically modified stem cells to deliver targeted molecular therapies that counteract mutations involved in RP. When integrated within the InGel scaffold, these specialized cells could further enhance photoreceptor resilience.
- Combination Therapies: There is growing interest in combining InGel therapies with gene therapies or specialized pharmacological agents. Some labs hypothesize that small-molecule drugs could amplify the effect of cell transplantation by inhibiting degenerative pathways.
- Advanced Imaging and Biomarkers: Researchers are refining imaging techniques to detect subtle changes in cone health earlier. Novel biomarkers for cone survival, inflammation, or metabolic stress may help clinicians tailor treatments to each patient’s unique retinal environment.
- Long-Term Safety Studies: While short- and mid-term safety data appear promising, ongoing trials focus on establishing the therapy’s performance over extended periods. This includes monitoring for potential late-onset complications, as well as quantifying how much of the therapy’s benefits persist years after a single administration.
The Global Collaborative Effort
A distinguishing feature of current research is the international scope of collaboration. Institutions across North America, Europe, and Asia pool data, optimize protocols, and refine best practices. This global network accelerates the pace of discovery and helps standardize outcome measures. By harmonizing research methods and sharing data across regulatory boundaries, investigators can better evaluate which protocols hold the most promise and which may require redesign.
The collective intelligence gained from these studies ultimately brings InGel Cell Therapy closer to mainstream clinical use. Encouraging findings signal that the approach can meaningfully aid in cone preservation—a critical advantage for patients needing central vision for daily tasks. Researchers remain mindful, however, that progress in regenerative therapies typically proceeds at a careful, measured pace, balancing hope with caution. Continued scientific rigor and collaboration are essential in cementing InGel Cell Therapy’s role as a reliable treatment for Retinitis Pigmentosa.
Assessing Efficacy, Safety, and Key Outcomes
For individuals experiencing vision loss from Retinitis Pigmentosa, the promise of any new therapy hinges on demonstrable efficacy and a robust safety profile. InGel Cell Therapy sets itself apart by specifically targeting cone cells—the photoreceptors critical for central, color, and high-resolution vision. Evaluating how well it safeguards these cells and the potential side effects it may pose is central to understanding its future role in standard clinical practice.
Core Measures of Efficacy
A range of clinical assessments helps gauge the effectiveness of InGel therapy in halting or slowing RP progression. While not every patient will experience the same degree of improvement, the following indicators are essential for determining therapeutic success:
- Visual Field Stability
- Traditional therapies often aim to protect peripheral vision first. However, cone photoreceptors, located primarily in the central portion of the retina, require specialized support to maintain tasks like reading, face recognition, and driving.
- A stable or slowly expanding central visual field in treated patients is a valuable sign that InGel therapy can bolster cone health. While some participants exhibit only a reduction in the rate of vision loss, others display subtle gains in clarity or color discrimination.
- Changes in Visual Acuity
- Though improvements in acuity remain modest in most reported cases, maintaining current levels for longer than expected is still beneficial. Even a slight uptick in acuity can translate to tangible improvements in daily living, such as reading larger print or recognizing faces at closer distances.
- Functional Light Sensitivity
- Because cones govern bright-light vision and color perception, tests that measure photopic (daylight) function provide critical insights. Participants sometimes report enhanced contrast sensitivity or better adaptation to different lighting conditions, suggesting that transplanted cells may release factors that revitalize existing cones.
- Quality of Life Metrics
- Beyond purely clinical indices, patient feedback on everyday tasks—like reading text on digital devices, distinguishing colors in clothing, or navigating new environments—offers a qualitative measure of success. Even mild improvements can rejuvenate a patient’s sense of independence and emotional well-being.
Understanding Safety and Potential Side Effects
Safety remains paramount in any intervention that involves introducing biological materials into the human body. While the overarching data so far indicates a low risk of severe complications, several factors warrant close monitoring:
- Immunological Reactions
- Introducing cells into the eye can elicit immune responses, particularly if the cells originate from donors. To date, occurrences of significant rejection or inflammation are uncommon, but mild immune reactions have been documented. Clinicians often mitigate these risks with short-term immunosuppressive regimens.
- Infection and Inflammation
- Ocular infections can threaten any surgical procedure. Therefore, strict adherence to sterile protocols is required. InGel therapy, delivered via subretinal injection, necessitates scrupulous preoperative and postoperative hygiene.
- Gel Displacement and Retinal Detachment
- If the gel migrates from its intended location, it could potentially disrupt retinal function or increase the risk of detachment. Experienced surgical teams employ precise injection techniques and meticulous follow-up imaging to reduce these complications.
- Intraocular Pressure Fluctuations
- Surgeries involving fluid injections can temporarily alter intraocular pressure (IOP). While most changes in IOP settle spontaneously, patients with pre-existing glaucoma or ocular hypertension may need additional monitoring.
Factors Influencing Variability in Outcomes
Not every patient with Retinitis Pigmentosa responds identically to InGel Cell Therapy. Several variables contribute to the range of observed outcomes:
- Stage of Disease: Patients with predominantly intact cone function may benefit more robustly from the therapy than those in very advanced stages of RP, where cone cells are profoundly diminished.
- Underlying Genetic Mutations: RP arises from mutations in over 60 genes. The exact mutation can influence how well cone cells respond to external interventions, affecting the therapy’s efficacy.
- Patient Age and Health Status: Younger patients typically display higher cellular regenerative capacity and may experience better outcomes. Similarly, a lack of comorbidities—such as diabetes or autoimmune disorders—can facilitate improved healing and cell acceptance.
- Adjunct Therapies: Individuals who also adopt dietary changes, vitamin supplementation, or other therapies (e.g., gene therapy, specialized drugs) might see amplified benefits when compared to those who rely solely on InGel therapy.
Moving Towards Standardization
As research evolves, standardizing how outcomes are measured will be essential. This approach allows clinicians to draw clearer comparisons between different trials or protocols, paving the way for establishing best practices. Collaborative networks are working to develop shared guidelines on dosing, cell preparation, and postoperative care to ensure that results from various research centers are both consistent and comparable.
Such consistency in methodology will ultimately help regulators and professional ophthalmic bodies determine whether InGel Cell Therapy can be recommended as a first-line or adjunct treatment for RP. Although many questions remain—particularly regarding long-term durability—the accumulating data points toward a potent new avenue for preserving the precious central vision that people with RP rely on.
Cost Considerations and Therapy Price
InGel Cell Therapy for Retinitis Pigmentosa is a specialized and resource-intensive intervention, so costs vary. Fees typically range from around \$15,000 to \$30,000, depending on the therapy center, type of cells, and the complexity of any additional treatments required. Several factors, such as diagnostic evaluations and postoperative follow-up sessions, may affect the total expense. Financial support programs and payment plans are sometimes available, and some patients explore insurance coverage, though it may be limited. Seeking consultations from multiple clinics can help determine the right balance of expertise, cost, and individual patient needs.
Disclaimer:
This article is for informational purposes only and does not substitute professional medical advice. Always consult a qualified healthcare provider for personalized guidance and to discuss any questions regarding medical conditions or treatment options.
We encourage you to share this article with friends, family, or anyone who may benefit from learning about InGel Cell Therapy. You can use our Facebook and X (formerly Twitter) share buttons or your preferred social platforms. By spreading the word, you can help more people stay informed about this promising approach to preserving vision in Retinitis Pigmentosa.