Branch retinal vein occlusion (BRVO) is a significant cause of sudden vision loss, affecting individuals worldwide and often linked to underlying vascular risk factors. When a branch of the retinal vein becomes blocked, blood flow is disrupted, resulting in retinal swelling, hemorrhage, and sometimes permanent visual impairment. Prompt, informed management can protect and even restore sight for many. This comprehensive guide explores the epidemiology, conventional and advanced treatments, interventional strategies, and cutting-edge research in BRVO—empowering patients, caregivers, and clinicians to make informed, proactive decisions for vision and vascular health.
Table of Contents
- Introduction to BRVO: Risk and Epidemiology
- Standard Medical and Pharmacologic Care
- Surgical and Interventional Solutions
- New Technologies and Therapeutic Frontiers
- Clinical Trials and Future Directions
- Frequently Asked Questions
Introduction to BRVO: Risk and Epidemiology
Branch retinal vein occlusion is a blockage of one of the small veins in the retina, the light-sensitive layer at the back of the eye. Unlike central retinal vein occlusion (CRVO), which affects the main vein, BRVO is confined to a specific section of the retina, often resulting in sectoral visual loss.
How Does BRVO Occur?
- Pathophysiology:
The blockage usually happens where an artery and vein cross. A hardened artery may compress the vein, causing turbulent blood flow, clotting, and eventual occlusion. - Risk Factors:
- Age: Most patients are over 50.
- Hypertension: The most significant risk factor.
- Diabetes Mellitus: Increases the risk by damaging blood vessels.
- High Cholesterol: Promotes atherosclerosis.
- Smoking: Damages vascular endothelium.
- Glaucoma: Raised eye pressure increases risk.
- Prevalence:
BRVO is more common than CRVO, with an estimated prevalence of 0.5% in adults over 40.
Clinical Signs
- Symptoms: Sudden, painless vision loss in part of the visual field.
- Findings: Retinal hemorrhages, swelling (macular edema), and sometimes abnormal blood vessel growth (neovascularization).
Practical Advice:
Routine eye exams are crucial for early detection of BRVO, especially if you have hypertension, diabetes, or other vascular risk factors. Notify your doctor of any sudden changes in vision.
Standard Medical and Pharmacologic Care
The primary goals in BRVO management are to treat complications (such as macular edema and neovascularization), minimize further vision loss, and address systemic risk factors to prevent recurrence or involvement of the other eye.
Immediate and Ongoing Medical Therapies
- Observation: Some patients with mild BRVO and no macular edema may recover vision without intervention. Close monitoring is essential.
- Control of Systemic Risk Factors:
- Lower blood pressure
- Optimize blood sugar
- Manage cholesterol
- Cease smoking
Pharmacologic Interventions
- Intravitreal Anti-VEGF Injections:
- Medications such as ranibizumab, aflibercept, and bevacizumab inhibit vascular endothelial growth factor (VEGF), reducing macular edema and improving vision in most patients.
- Typical schedule: monthly injections, then gradually extended based on response.
- Steroid Injections or Implants:
- Intravitreal corticosteroids (e.g., dexamethasone implant) are alternatives, especially if anti-VEGF therapy is not effective or not tolerated.
- Risks include cataract progression and elevated intraocular pressure.
Adjunctive Therapies
- Laser Photocoagulation:
- Grid laser is considered for macular edema unresponsive to injections or in certain resource-limited settings.
- Sectoral laser is used to prevent neovascularization in eyes with widespread retinal nonperfusion.
Home and Lifestyle Measures
- Monitor vision with an Amsler grid at home.
- Maintain regular follow-up appointments.
- Adopt a heart-healthy diet and regular physical activity.
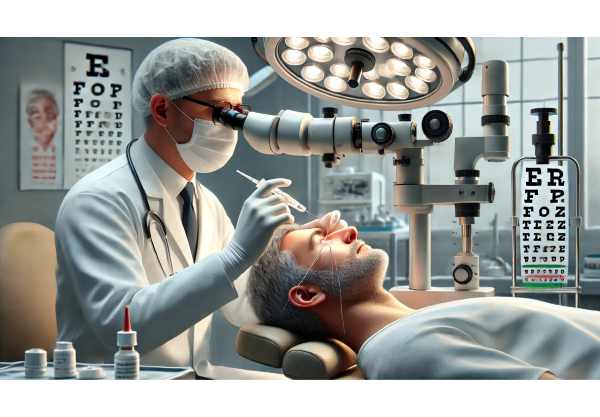
Surgical and Interventional Solutions
Surgical management for BRVO is less common than pharmacologic care but is sometimes considered for specific complications or refractory cases.
Laser-Based Interventions
- Grid/Focal Laser Photocoagulation:
- Effective for chronic macular edema, particularly if there is evidence of leaking microaneurysms.
- Scatter Laser (Panretinal Photocoagulation):
- Used for neovascularization, reducing the risk of vitreous hemorrhage and neovascular glaucoma.
Surgical Approaches
- Pars Plana Vitrectomy:
- Indicated in rare cases with persistent vitreous hemorrhage or tractional retinal detachment.
- May be considered for chronic, nonresolving macular edema with significant vitreomacular traction.
Emerging Interventional Techniques
- Radial Optic Neurotomy and Sheathotomy:
- Experimental microsurgical procedures aimed at relieving venous compression. Results remain variable and unproven.
Risks and Considerations
- Surgical intervention carries risk and is generally reserved for severe complications.
- Discuss all potential benefits and risks with your retinal specialist before proceeding.
Practical Advice:
If you’re facing potential surgery, ask about the goals, expected outcomes, and alternative options. Second opinions are valuable for surgical decisions.
New Technologies and Therapeutic Frontiers
Ophthalmic research continues to explore innovative treatments and diagnostic advancements for BRVO, offering renewed hope for vision restoration and complication prevention.
Diagnostic Advances
- Optical Coherence Tomography Angiography (OCTA):
- Enables detailed, non-invasive visualization of retinal blood vessels and ischemia.
- AI-Powered Diagnostics:
- Artificial intelligence models analyze retinal images, improving early detection and risk stratification.
Therapeutic Breakthroughs
- Next-Generation Anti-VEGF Agents:
- Extended-duration formulations and biosimilars are under development, aiming to reduce injection frequency.
- Gene Therapy:
- Investigational treatments target underlying causes of retinal edema or vascular proliferation.
- Implantable Drug Delivery Systems:
- Long-acting reservoirs and biodegradable implants for steady medication release, reducing patient burden.
Telemedicine and Remote Monitoring
- Smartphone-based visual field tests and home-based OCT devices help monitor for complications and reduce the need for frequent office visits.
Practical Advice:
Ask your provider about new clinical tools and whether emerging technologies are appropriate for your case. Stay engaged in your care through digital health solutions when available.
Clinical Trials and Future Directions
Continued research into BRVO management is vital for further improving outcomes and expanding treatment options.
Ongoing Clinical Trials
- Comparative Efficacy of Anti-VEGF Agents:
- Trials are assessing head-to-head outcomes, extended dosing intervals, and safety of newer agents.
- Steroid-Sparing Approaches:
- Exploring alternatives for patients intolerant of steroids or at risk for complications.
- Novel Laser and Surgical Techniques:
- Innovative laser patterns and minimally invasive procedures are being tested to optimize outcomes and reduce side effects.
Future Directions
- Personalized Medicine:
- Genetic and biomarker studies may allow for individualized therapy in the near future.
- Prevention Strategies:
- Integration of cardiovascular risk reduction and public health screening to prevent initial or recurrent BRVO.
- Regenerative Medicine:
- Investigations into retinal cell regeneration and repair may eventually restore lost vision.
Participation in Research
- Patients may consider enrolling in clinical trials, which can provide access to the latest treatments and contribute to advancing care.
Practical Advice:
Stay informed about research opportunities and discuss participation in trials with your provider. Long-term follow-up and risk factor management are essential for the best possible outcome.
Frequently Asked Questions
What causes branch retinal vein occlusion?
BRVO is typically caused by a blockage where a retinal artery compresses a vein, often due to atherosclerosis, high blood pressure, diabetes, or blood clotting disorders.
How is branch retinal vein occlusion treated?
Treatment focuses on reducing macular edema and preventing complications. Intravitreal anti-VEGF injections, corticosteroid injections or implants, and laser therapy are the mainstays. Controlling underlying vascular risk factors is essential.
Can vision recover after BRVO?
Many patients regain some vision, especially with prompt anti-VEGF or steroid therapy. Some may experience permanent vision changes, depending on the severity and duration before treatment.
Is surgery needed for BRVO?
Surgery is rarely needed for BRVO. It may be considered for complications like non-resolving vitreous hemorrhage or tractional retinal detachment.
How can BRVO be prevented?
Managing blood pressure, diabetes, cholesterol, and not smoking can help prevent BRVO. Regular eye exams are crucial for early detection and intervention.
What are the symptoms of branch retinal vein occlusion?
BRVO typically presents as sudden, painless vision loss or blurred vision in part of one eye, often with associated retinal hemorrhages and swelling.
Disclaimer:
This article is for educational purposes only and should not be taken as a substitute for professional medical advice. Always consult a qualified healthcare provider for diagnosis and individualized treatment.
If you found this guide helpful, please consider sharing it on Facebook, X (formerly Twitter), or your favorite social platform. Your support helps us bring more trusted eye health content to the community—thank you!






