Gonococcal conjunctivitis is a rapidly progressing eye infection caused by Neisseria gonorrhoeae, a bacterium more commonly linked to sexually transmitted infections. This condition can lead to severe corneal damage and potential vision loss if not addressed urgently. Though most cases are seen in newborns and sexually active adults, anyone exposed to contaminated fluids is at risk. Early diagnosis, prompt medical intervention, and awareness of new advances are critical to successful outcomes. In this guide, we comprehensively explore conventional treatments, surgical interventions, and the latest emerging innovations in managing gonococcal conjunctivitis for both acute and recurrent cases.
Table of Contents
- Understanding Gonococcal Conjunctivitis and Epidemiology
- Mainstream Medical and Drug Approaches
- Surgical and Interventional Solutions
- Cutting-Edge Advancements and Innovative Therapies
- Clinical Trials and Future Outlook
- Frequently Asked Questions
- Disclaimer
Understanding Gonococcal Conjunctivitis and Epidemiology
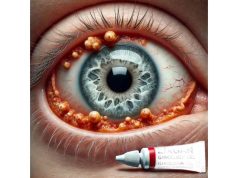
Gonococcal conjunctivitis is a severe, purulent (pus-producing) bacterial infection of the eye. It is caused by the bacterium Neisseria gonorrhoeae, which is primarily transmitted through direct contact with infected genital secretions. While often associated with neonates (ophthalmia neonatorum), adults can acquire the infection through hand-to-eye contact, particularly if there is underlying urogenital gonorrhea.
Pathophysiology and Clinical Features
- N. gonorrhoeae can invade intact conjunctival epithelium, making infection aggressive.
- Presents with rapid-onset redness, intense swelling, profuse yellow-green discharge, and marked eyelid swelling.
- Severe cases can progress to corneal ulceration, perforation, and irreversible vision loss within hours to days if untreated.
Prevalence and At-Risk Groups
- Incidence is higher in developing countries due to limited perinatal care and screening.
- Neonates acquire infection during passage through an infected birth canal.
- Adults: increased risk with high-risk sexual behaviors, lack of hygiene, and unprotected sexual contact.
- Emerging resistance patterns are shifting prevalence and challenging conventional management.
Risk Factors
- Unprotected sexual intercourse, multiple partners, history of sexually transmitted infections.
- Absence of prophylactic ocular care in newborns.
- Immunocompromised states and poor personal hygiene.
Complications
- Corneal ulceration and scarring.
- Endophthalmitis (deep eye infection).
- Systemic dissemination, particularly in infants.
Prevention Strategies
- Perinatal screening for gonorrhea and prompt maternal treatment.
- Universal application of ocular prophylaxis in newborns.
- Sexual health education, barrier protection, and prompt STI treatment.
Practical Advice:
- If you or your child experiences sudden, profuse eye discharge with swelling, seek medical help without delay.
Mainstream Medical and Drug Approaches
The mainstay of treatment for gonococcal conjunctivitis is rapid initiation of systemic and topical antibiotics, as delay can lead to irreversible eye damage. Hospitalization is often necessary to ensure effective treatment, monitoring, and prevention of complications.
Immediate Steps
- Urgent ophthalmological evaluation.
- Isolation of the affected individual to prevent spread.
Antibiotic Therapy
- Systemic Therapy
- First-line: Intravenous or intramuscular third-generation cephalosporins (typically ceftriaxone).
- Adults: 1g ceftriaxone IV or IM daily for 3-7 days.
- Neonates: Dosage adjusted based on age and weight.
- Oral azithromycin is often added to address possible chlamydial co-infection.
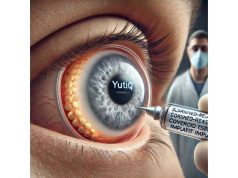
- Topical Therapy
- Intensive irrigation of the eye with saline to clear discharge.
- Topical antibiotic eye drops or ointments (fluoroquinolones or aminoglycosides) as adjunct.
- Supportive Measures
- Pain control: cold compresses, lubricating drops.
- Eye patching is discouraged due to risk of anaerobic growth.
Monitoring
- Daily ophthalmic examination to monitor for corneal involvement.
- Hospital admission for severe cases, infants, or noncompliance risk.
Patient Counseling
- Abstain from sexual activity until treatment completion and negative test-of-cure.
- Screen and treat sexual partners simultaneously.
- Reinforce personal hygiene—wash hands before and after touching eyes.
Special Considerations
- Resistant strains may require alternative or combination regimens.
- Pregnant or breastfeeding patients may need adjusted therapy.
Practical Advice:
- Do not self-treat with leftover antibiotics or delay care—progression can be rapid.
Surgical and Interventional Solutions
Surgical management is rarely first-line but may be necessary when complications arise, especially if corneal perforation or deep-seated infection develops.
Indications for Surgical Intervention
- Corneal ulceration with risk of perforation.
- Actual corneal perforation.
- Severe eyelid or conjunctival necrosis.
- Abscess formation or endophthalmitis.
Common Procedures
- Corneal Gluing or Patching
- For small corneal perforations, tissue adhesives or patch grafts may temporarily restore integrity.
- Amniotic Membrane Transplantation
- Used to promote healing and reduce inflammation in severe conjunctival/corneal disease.
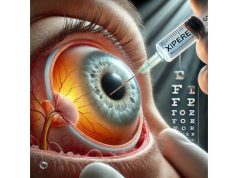
- Corneal Transplantation (Keratoplasty)
- Indicated for large corneal defects or when visual rehabilitation is possible after acute infection control.
- Conjunctival or Eyelid Debridement
- Surgical removal of necrotic tissue to limit spread of infection.
- Evisceration or Enucleation
- Reserved for uncontrollable infection with endophthalmitis, as a last resort to protect life.
Postoperative Care
- Continuation of intensive antibiotics and anti-inflammatories.
- Meticulous monitoring for graft survival or recurrent infection.
- Low-vision aids or rehabilitation support, if necessary.
Patient and Family Support
- Early psychological counseling for vision loss or eye removal.
- Encouragement and support for adaptation and recovery.
Practical Advice:
- Adherence to prescribed antibiotics after surgery is essential for healing and prevention of reinfection.
Cutting-Edge Advancements and Innovative Therapies
Recent years have seen notable advances in both diagnostics and therapeutics for gonococcal conjunctivitis, prompted by the challenge of emerging antimicrobial resistance and demand for rapid, vision-saving care.
Diagnostic Innovations
- PCR and Molecular Testing: Enables swift, accurate detection of N. gonorrhoeae and identification of resistance genes.
- Point-of-Care Rapid Testing: Allows immediate diagnosis in clinics, birthing centers, and remote settings.
Novel Antimicrobial Strategies
- New Generation Cephalosporins: Agents with greater potency against resistant strains are under development.
- Adjunctive Antimicrobial Peptides: Experimental agents targeting bacteria without promoting resistance.
- Bacteriophage Therapy: Investigational use of viruses that selectively kill N. gonorrhoeae.
Biomaterials and Ocular Surface Repair
- Bioengineered Corneal Scaffolds: For faster healing in corneal ulceration.
- Growth Factor Eye Drops: Enhances regeneration after deep infection.
Digital Health and Remote Care
- Teleophthalmology: Facilitates rapid triage and specialist access in underserved areas.
- Mobile Apps: Support adherence to medication schedules and prompt follow-up.
Infection Control Innovations
- Contact Tracing Technology: Digital tools help identify and notify sexual contacts for testing and treatment.
- Automated Irrigation Devices: Enhance safety and thoroughness of conjunctival lavage in clinics.
Practical Advice:
- Patients should ask providers about new therapies and clinical trial options, especially for resistant or recurrent cases.
Clinical Trials and Future Outlook
Ongoing research is shaping the future of gonococcal conjunctivitis care, with a strong focus on overcoming antibiotic resistance and reducing vision loss worldwide.
Areas of Active Investigation
- Next-Generation Antibiotics: Trials of new cephalosporins, carbapenems, and combinations to counter resistance.
- Topical Bacteriophage Formulations: Evaluating safety and effectiveness in drug-resistant cases.
- Genetic Screening: Identifying markers for high-risk or recurrent infection.
- Vaccination Strategies: Early-stage research into vaccines to prevent N. gonorrhoeae infection.
Emerging Trends
- Integration of rapid molecular diagnostics into all hospital birthing centers.
- Personalized antibiotic regimens based on resistance profiling.
- Expanded use of telemedicine in eye infection triage, particularly in resource-limited areas.
Global Health Initiatives
- Universal perinatal screening and ocular prophylaxis.
- Public health campaigns to reduce stigma and encourage prompt care-seeking.
- International collaborations for surveillance of antibiotic resistance trends.
Vision for the Future
- Zero vision loss from gonococcal conjunctivitis through rapid, targeted, and personalized care.
- Accessible, affordable diagnostic and treatment innovations worldwide.
Staying Engaged
- Patients and families are encouraged to participate in registries, clinical trials, and awareness programs for ongoing support.
Frequently Asked Questions
What is gonococcal conjunctivitis and how is it different from other eye infections?
Gonococcal conjunctivitis is a severe bacterial eye infection caused by Neisseria gonorrhoeae. Unlike other forms, it progresses rapidly, causes profuse discharge, and can lead to vision loss if untreated.
How is gonococcal conjunctivitis treated?
Treatment involves immediate intravenous antibiotics (usually ceftriaxone), intensive eye irrigation, and topical antibiotics. Hospital admission is often required to monitor and prevent complications.
What are the signs and symptoms of gonococcal conjunctivitis?
Key signs include rapid onset of redness, swelling, and thick pus-like discharge from the eyes. In severe cases, pain, blurred vision, and corneal involvement may occur.
Can adults get gonococcal conjunctivitis?
Yes. While common in newborns, adults can contract it through hand-to-eye transmission from genital secretions, especially in those with high-risk sexual behaviors.
Is gonococcal conjunctivitis contagious?
Yes. It can spread through direct contact with infected secretions. Prompt treatment and hygiene are crucial to prevent transmission.
How can gonococcal conjunctivitis be prevented?
Prevention includes safe sexual practices, screening and treating pregnant women, and applying antibiotic ointment to newborns’ eyes at birth.
What should I do if I suspect I have gonococcal conjunctivitis?
Seek emergency medical care. Do not attempt self-treatment, as delays can result in permanent vision loss.
Disclaimer
This article is intended for educational purposes only and should not be used as a substitute for direct professional medical advice. If you or your child have symptoms suggestive of eye infection, consult a healthcare provider immediately. Please share this article on Facebook, X (formerly Twitter), or your preferred platform, and follow us on social media. Your support helps us continue creating trusted, up-to-date eye health content.