Retinoblastoma is a rare, malignant tumor of the retina that primarily affects young children under the age of five. It develops from retinal cells, which are expected to mature into light-sensing cells. This cancer, which is known to develop as a result of genetic mutations, can affect either one or both eyes (unilateral or bilateral). The primary genetic cause is a mutation in the RB1 gene, which controls cell division. When this gene is altered, it can cause uncontrolled cell growth, resulting in a tumor.
Retinoblastoma accounts for approximately 2-4% of all childhood cancers, with an incidence rate of one in every 15,000 to 20,000 live births. Early detection is critical for successful treatment and can often be accomplished through a simple eye examination that reveals a white reflex, known as leukocoria, in the pupil. This abnormal reflection is often the first thing parents or pediatricians notice, and it can appear in photographs taken with a flash.
The prognosis for retinoblastoma has significantly improved over the years, with survival rates exceeding 95% in developed countries thanks to early detection and advanced treatment options. However, the outcomes may be less favorable in low-resource settings where access to timely medical care is limited. Despite high survival rates, successfully managing retinoblastoma necessitates a multidisciplinary approach to preserve vision and prevent metastasis. Understanding the disease’s genetic basis and clinical presentation is critical for early intervention and effective management.
Standard Retinoblastoma Care and Treatment
Retinoblastoma management necessitates a multifaceted approach that takes into account the tumor’s size, location, extent of spread, and the child’s overall health. Standard treatment methods seek to eliminate the tumor, preserve the eye and vision whenever possible, and reduce long-term side effects. The mainstays of retinoblastoma treatment are chemotherapy, focal therapies, radiation therapy, and enucleation.
- Chemotherapy: Systemic chemotherapy is frequently the first line of treatment for retinoblastoma, particularly when the tumor is too large for local treatment alone. Chemotherapy can shrink the tumor, making it more responsive to focal therapies. Vincristine, etoposide, and carboplatin are some of the most commonly used chemotherapy agents. Intra-arterial chemotherapy, which delivers drugs directly into the ophthalmic artery, has also shown promise in terms of more effectively targeting the tumor while causing fewer systemic side effects.
- Focal Therapies: Laser photocoagulation, cryotherapy, and thermotherapy are examples of therapies used to destroy smaller tumors or treat residual tumor cells after chemotherapy.
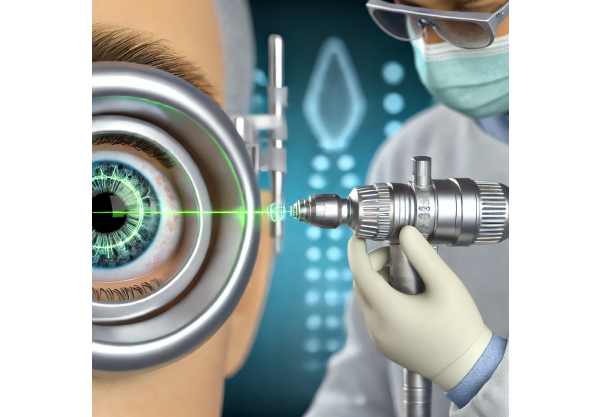
- Laser Photocoagulation: Laser beams coagulate and destroy the tumor’s blood supply.
- Cryotherapy: The tumor cells are frozen using a cryoprobe.
- Thermotherapy: The use of heat, typically delivered via an infrared laser, to kill cancer cells.
- Radiation Therapy: External beam radiation therapy (EBRT) was once a popular treatment for retinoblastoma, but it is no longer widely used due to long-term side effects, such as an increased risk of secondary cancers. Brachytherapy, a type of localized radiation in which radioactive plaques are placed near the tumour, is sometimes used to treat more resistant or recurring tumours.
- Enucleation: Surgical removal of the eye is considered when the tumor is large, vision cannot be preserved, or the cancer is likely to spread. This procedure ensures complete tumor removal, giving patients the best chance of survival in advanced cases. Prosthetic eyes can be fitted after enucleation to restore a normal appearance.
- Genetic Counseling and Testing: Because retinoblastoma is hereditary, affected families require genetic counseling and testing. Identifying RB1 gene mutations aids in risk assessment, early detection among siblings, and future family planning.
- Follow-Up and Supportive Care: Continuous follow-up is required to monitor for tumor recurrence, manage any treatment-related side effects, and address psychosocial concerns. Supportive care, such as vision rehabilitation and psychological support, can significantly improve the quality of life for retinoblastoma survivors.
Innovative Retinoblastoma Treatment Options
In recent years, there have been significant advances in the treatment of retinoblastoma, with novel approaches aimed at improving survival rates, preserving vision, and reducing treatment-related side effects. These cutting-edge innovations cover a wide range of topics, including genetic therapies, advanced drug delivery systems, novel focal treatments, and immunotherapy.
Genetic Therapy: Precision Medicine for Retinoblastoma
Understanding the genetic basis of retinoblastoma has laid the groundwork for precision medicine approaches. Genetic therapies aim to target the specific mutations that cause tumor development, allowing for more effective and personalized treatments.
One of the most promising avenues in genetic therapy is the use of gene editing technologies such as CRISPR-Cas9. This technology allows for precise DNA modifications, which could potentially correct the RB1 gene mutations that cause retinoblastoma. Preclinical research has demonstrated the viability of using CRISPR to repair genetic defects in retinal cells, paving the way for future clinical applications.
Another novel approach is gene replacement therapy, which delivers a functional copy of the RB1 gene to retinal cells via viral vectors. This method seeks to restore normal cell cycle control while preventing tumor development. While still in the experimental stages, gene replacement therapy shows great promise for treating hereditary retinoblastoma at its source.
Advanced Drug Delivery Systems to Improve Chemotherapy Efficacy
Traditional systemic chemotherapy for retinoblastoma can cause serious side effects due to the high doses required to reach the eye. Recent advances in drug delivery systems aim to increase chemotherapy efficacy while reducing systemic toxicity.
Intra-arterial chemotherapy (IAC) has transformed retinoblastoma treatment by delivering chemotherapeutic agents directly into the ophthalmic artery, which supplies the eye. This targeted approach allows higher drug concentrations to reach the tumor, increasing efficacy while reducing systemic side effects. Clinical trials have demonstrated high success rates with IAC, particularly for advanced unilateral retinoblastoma.
Intravitreal chemotherapy is another cutting-edge technique that involves injecting drugs directly into the vitreous humor of the eye. This method is especially useful for treating vitreous seeding, which occurs when cancer cells spread throughout the eye’s vitreous cavity. Melphalan or topotecan injections into the eye have shown promising results in controlling intraocular tumor spread while preserving vision.
Nanotechnology-based drug delivery systems are also under investigation for retinoblastoma treatment. Nanoparticles can be engineered to transport chemotherapeutic agents directly to tumor cells, increasing drug uptake and efficacy. These systems have the potential to provide controlled and sustained drug release, thereby improving treatment outcomes.
New Focal Treatments: Precision Targeting of Tumor Cells
Innovations in focal treatments improve the precision and efficacy of retinoblastoma therapies. These treatments aim to target and destroy tumor cells while preserving healthy retinal tissue.
High-intensity focused ultrasound (HIFU) is a new technology that employs focused ultrasound waves to generate heat and kill tumor cells. HIFU provides a non-invasive alternative to traditional focal therapies, with the potential for precise targeting while causing minimal damage to surrounding tissues. Preclinical studies have yielded promising results, and clinical trials are currently underway to determine its efficacy in retinoblastoma patients.
Photodynamic therapy (PDT) is another novel focal treatment that employs light-activated compounds to kill cancer cells. In PDT, a photosensitizing agent is injected into the bloodstream and selectively absorbed by tumor cells. When exposed to a specific wavelength of light, the agent generates reactive oxygen species, which kill cancer cells. PDT has the advantage of being highly selective, which lowers the risk of damage to healthy retinal cells.
Immunotherapy: Leveraging the Immune System
Immunotherapy is a groundbreaking approach to cancer treatment that uses the body’s immune system to target and destroy cancer cells. Recent advances in immunotherapy show promise for treating retinoblastoma, especially in cases where traditional therapies have failed.
Chimeric antigen receptor (CAR) T-cell therapy is a type of immunotherapy that involves modifying a patient’s T-cells to express tumor antigen-specific receptors. These engineered T-cells can then identify and eliminate cancer cells. Preclinical studies have shown that CAR T-cell therapy can target retinoblastoma cells, and clinical trials are planned to assess its safety and efficacy in children with retinoblastoma.
Checkpoint inhibitors are another type of immunotherapy drug that helps the immune system identify and attack cancer cells. These drugs work by inhibiting proteins that prevent immune cells from attacking tumors. While checkpoint inhibitors have been successful in treating other cancers, their use in retinoblastoma is still in the early stages of research.
Personalized Medicine: Tailored Treatment for Individual Patients
Personalized medicine entails tailoring treatment to the unique genetic and molecular profile of each patient’s tumor. Advances in genomic sequencing and molecular diagnostics are making it possible to identify specific genetic mutations and biomarkers associated with retinoblastoma, paving the way for more precise and targeted treatments.
Liquid biopsy is a non-invasive diagnostic tool for detecting circulating tumor DNA (ctDNA) in the blood. Liquid biopsies can provide real-time information about the tumor’s genetic makeup, which can help guide treatment decisions and monitor response to therapy. This technology is a less invasive alternative to traditional biopsies, with the potential to detect early signs of treatment resistance or relapse.






