Actinic keratosis (AK) is a common skin condition caused by years of sun exposure, resulting in rough, scaly patches that may develop into squamous cell carcinoma if left untreated. Affecting millions worldwide, AK is often seen as a warning sign, offering a crucial window for early intervention and skin cancer prevention. While most lesions are harmless, effective management is vital for long-term skin health. This comprehensive guide explores the core principles, proven therapies, surgical techniques, cutting-edge advances, and what patients can expect for the future of actinic keratosis treatment.
Table of Contents
- Fundamentals and Patterns of Occurrence
- Mainstay Medical Therapies and Topical Options
- Procedural and Surgical Approaches
- New Technologies and Innovative Treatments
- Future Directions and Clinical Research
- Frequently Asked Questions
Fundamentals and Patterns of Occurrence
Actinic keratosis, also called solar keratosis, develops when repeated exposure to ultraviolet (UV) light damages skin cells. Over time, this damage leads to changes in the outermost layer of the skin—producing rough, crusty, or scaly lesions. These patches, often found on sun-exposed areas such as the face, scalp, ears, hands, and forearms, can range in color from flesh-toned to reddish-brown.
How does actinic keratosis develop?
The main culprit is cumulative sun exposure, especially in fair-skinned individuals who burn easily. The damage accumulates over years and, in some cases, decades. The resulting atypical skin cells may eventually progress to squamous cell carcinoma, a form of skin cancer.
Prevalence and demographics:
- AK is highly prevalent in older adults, particularly those over age 50 or with a history of significant sun exposure.
- Rates are highest among people with light skin, light eyes, and hair.
- Outdoor workers, athletes, and individuals living in sunny climates face increased risk.
Key risk factors include:
- Chronic sun or tanning bed exposure
- Fair skin, freckles, or light hair
- History of sunburns
- Weakened immune system (e.g., organ transplant recipients)
- Advanced age
Practical advice:
- Examine your skin regularly, focusing on sun-exposed areas. Early detection is critical—see a dermatologist if you notice new or changing spots.
- Wear broad-spectrum sunscreen daily and protective clothing to help prevent AK and future complications.
Mainstay Medical Therapies and Topical Options
Non-surgical treatment forms the foundation of actinic keratosis management, particularly for widespread or multiple lesions. Medical therapies are designed to target abnormal skin cells, encourage healthy regeneration, and prevent progression to skin cancer.
Topical medications commonly used:
- 5-Fluorouracil (5-FU):
- A chemotherapy cream that destroys atypical cells by blocking DNA synthesis.
- Used once or twice daily for 2–4 weeks, leading to visible redness and crusting as lesions resolve.
- Best for treating larger areas with many lesions (“field therapy”).
- Imiquimod:
- A cream that stimulates the immune system to attack abnormal cells.
- Typically applied two to three times per week for several weeks.
- May cause local irritation, redness, and swelling, which is a sign that it’s working.
- Diclofenac Sodium Gel:
- A non-steroidal anti-inflammatory medication applied twice daily for 2–3 months.
- Milder side effects, making it a popular option for sensitive skin.
- Ingenol Mebutate:
- A gel formerly used for AK, acting both by cell death and immune stimulation.
- Use has declined due to safety concerns, but some countries still use it under strict medical supervision.
Other topical approaches:
- Retinoids (like tretinoin) may be used as adjunctive therapy.
- Combination regimens (e.g., 5-FU plus calcipotriene) are under investigation to increase effectiveness.
Practical living tips:
- Follow your dermatologist’s instructions closely. Use gloves or wash hands after applying topical medications.
- Expect redness, peeling, and temporary discomfort during therapy—this is usually a sign the medication is effective.
- Sun protection remains essential even during treatment to prevent new lesions.
Field therapy versus lesion-directed therapy:
- Field therapy is recommended for multiple, ill-defined, or recurring patches.
- Individual lesion therapy (see next section) may be preferred for isolated, well-defined spots.
Procedural and Surgical Approaches
When actinic keratoses are isolated, thickened, or unresponsive to topical treatment, in-office procedures provide fast, effective results. These interventions focus on removing visible lesions and minimizing scarring.
Common procedural options:
- Cryotherapy (Cryosurgery):
- The most widely used procedure—liquid nitrogen is applied to freeze and destroy abnormal skin cells.
- Causes blistering and crusting, followed by natural skin healing over 1–2 weeks.
- Especially effective for single or few lesions.
- Curettage and Desiccation:
- A sharp instrument (curette) scrapes away the lesion, and heat or chemical agents control bleeding and destroy remaining abnormal cells.
- Often combined with local anesthesia; results in a small wound that heals over time.
- Laser Therapy:
- Ablative lasers (CO2 or Er\:YAG) vaporize the top layers of skin, removing AK lesions and rejuvenating the skin.
- Suitable for multiple or difficult-to-treat areas, but may require downtime.
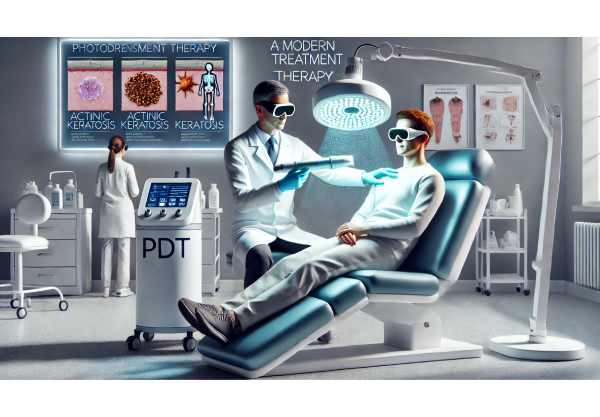
- Photodynamic Therapy (PDT):
- Involves applying a photosensitizing agent (aminolevulinic acid) to the skin, then activating it with a specific light wavelength.
- This selectively destroys precancerous cells with minimal impact on healthy tissue.
- Can treat larger skin areas and offers cosmetic benefits.
- Surgical Excision:
- Rarely needed for AK unless there is suspicion of invasive cancer.
- Ensures complete removal with clear margins, followed by closure with stitches.
Practical guidance for procedures:
- Most treatments are done in-office with minimal discomfort and short recovery.
- Protect treated areas from the sun during healing.
- Scarring and pigment changes are rare but possible—discuss these risks with your provider.
Minimally invasive and home-based approaches:
- Some patients with many lesions or high risk may combine therapies for optimal effect.
- Emerging home devices are under study but not yet standard.
New Technologies and Innovative Treatments
The field of actinic keratosis management is rapidly evolving, with novel therapies and high-tech approaches offering hope for improved outcomes, comfort, and cosmetic results.
Recent and emerging innovations:
- Daylight Photodynamic Therapy (Daylight PDT):
- Uses natural sunlight to activate the photosensitizer, offering a gentler, less painful alternative to traditional PDT.
- Increasingly popular in Europe and Australia; being evaluated in the U.S. and other countries.
- Nanoformulated and Liposomal Topicals:
- Advanced drug delivery systems aim to improve penetration, efficacy, and reduce side effects of topical medications.
- Fractional Laser-Assisted Drug Delivery:
- Combining fractional laser with topical therapies enhances drug absorption and lesion clearance.
- May allow for shorter, less intense treatment courses.
- AI-Assisted Diagnosis and Treatment Monitoring:
- Artificial intelligence is making headway in identifying suspicious lesions using smartphone images and dermoscopy.
- Early studies show AI systems can aid in diagnosis and treatment selection.
- Gene and Molecular Targeted Therapies:
- Research is underway to identify and block key molecular pathways that drive AK progression, potentially leading to personalized therapies.
- Home-Based Treatment Innovations:
- Remote monitoring, teledermatology, and “smart” apps allow patients to track skin changes and share progress with clinicians.
Advice for staying ahead:
- Ask your dermatologist about new treatment options if you have resistant, extensive, or recurring AK.
- Participate in research or registries to gain early access to innovative therapies.
Future Directions and Clinical Research
As our understanding of actinic keratosis deepens, researchers are uncovering fresh strategies for prevention, earlier detection, and more effective treatment.
Current and upcoming research focuses:
- Ongoing and Future Clinical Trials:
- Trials are investigating new topical medications, improved formulations of existing drugs, and combinations for increased effectiveness with fewer side effects.
- Comparative studies of standard versus innovative treatments are underway to determine the best long-term outcomes.
- Genomic and Proteomic Studies:
- Mapping genetic and protein changes in AK may reveal early markers for cancer risk and guide targeted therapies.
- Chemoprevention:
- Scientists are evaluating oral and topical agents (like nicotinamide) to prevent the development of new AK lesions in high-risk groups.
- Telemedicine Expansion:
- Virtual consultations, AI-driven skin checks, and home-based monitoring are making specialist care more accessible.
- Long-Term Outcome Research:
- Tracking patients over years helps determine which therapies best reduce risk of skin cancer and maintain skin health.
What’s on the horizon?
- Personalized medicine approaches using genetic profiling
- Enhanced AI-based diagnosis for earlier intervention
- Less invasive, more comfortable treatments for large or sensitive skin areas
Getting involved:
- Consider enrolling in clinical trials if current therapies are not meeting your needs.
- Stay connected with dermatology experts and reputable online resources for updates.
Frequently Asked Questions
What is the best treatment for actinic keratosis?
The best treatment depends on lesion number, size, location, and patient preference. Options include topical medications (like 5-fluorouracil), cryotherapy, photodynamic therapy, and laser treatments. Your dermatologist can recommend the most suitable approach.
Is actinic keratosis a type of skin cancer?
Actinic keratosis is not cancer but is considered precancerous. Left untreated, some lesions may progress to squamous cell carcinoma, making early treatment and regular monitoring important.
How can I prevent actinic keratosis?
Prevention centers on sun protection—use broad-spectrum sunscreen, wear protective clothing, avoid peak sun hours, and never use tanning beds. Early detection and prompt treatment reduce long-term risks.
Are home remedies effective for actinic keratosis?
No home remedies are proven to treat actinic keratosis effectively. Professional medical treatments are needed to safely remove lesions and reduce cancer risk.
Does actinic keratosis always need treatment?
Yes, most dermatologists recommend treating all actinic keratosis lesions to lower the risk of progression to skin cancer. Some thin lesions may resolve spontaneously, but monitoring and professional guidance are advised.
What does actinic keratosis look like?
AK usually appears as rough, scaly, or crusty patches on sun-exposed skin, often pink, red, or brown. Lesions may be flat or raised and sometimes feel tender to the touch.
Disclaimer:
This article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a dermatologist or healthcare provider for advice specific to your situation.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your favorite social network. Your support allows us to keep producing reliable, expert-driven skin health content. Follow us on social media for more tips and updates—thank you for being part of our community!






