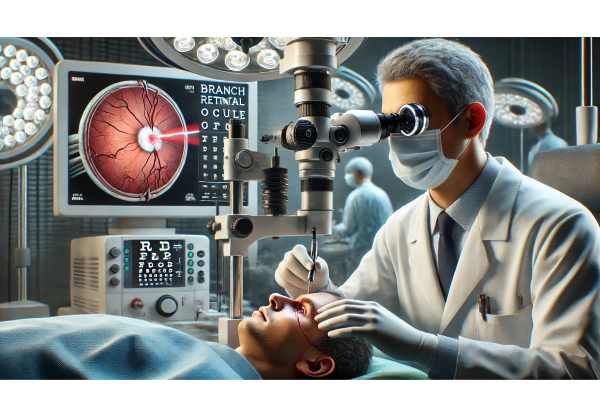
Branch retinal artery occlusion (BRAO) is a sudden, sight-threatening event caused by a blockage in one of the small arteries supplying the retina. Although rare, its impact on vision and the potential underlying health risks make it a true ophthalmic emergency. Prompt recognition, systemic evaluation, and targeted management are critical for preserving sight and preventing future vascular events. In this comprehensive guide, we’ll journey through the essential facets of BRAO—from the latest in diagnosis, to conventional and surgical interventions, and the exciting horizon of research and technology. Whether you’re a patient, caregiver, or clinician, this resource is designed to inform and empower.
Table of Contents
- Understanding BRAO: Causes and Risk Patterns
- Medical and Pharmacological Therapies for BRAO
- Surgical and Interventional Management Strategies
- Cutting-Edge Innovations and Diagnostic Progress
- Clinical Trials and Emerging Directions
- Frequently Asked Questions
Understanding BRAO: Causes and Risk Patterns
Branch retinal artery occlusion occurs when a blockage—most often an embolus, such as a cholesterol plaque or blood clot—interrupts blood flow in one of the smaller retinal arteries. This blockage deprives retinal tissue of oxygen, resulting in sudden, painless vision loss, usually affecting only part of the visual field.
Pathophysiology and Risk Factors
- Emboli: Most BRAO cases stem from emboli originating in the carotid arteries or heart.
- Atherosclerosis: Chronic vessel disease increases the risk, especially in older adults.
- Cardiovascular risk factors: Hypertension, diabetes, hyperlipidemia, smoking, atrial fibrillation, and coronary artery disease all heighten risk.
- Systemic diseases: Conditions like giant cell arteritis, vasculitis, or clotting disorders may also contribute.
Prevalence and Epidemiology
- BRAO is less common than central retinal artery occlusion (CRAO), but still accounts for a significant number of acute retinal vascular events.
- Most often seen in people over 60, with a slight male predominance.
- Incidence is estimated at 5–15 per 100,000 people annually, but this may be underreported due to subclinical cases.
Clinical Features
- Sudden, painless loss of vision or a dark “curtain” in part of the visual field.
- Sometimes preceded by episodes of transient vision loss (amaurosis fugax).
- Associated with visible whitening of the retina along the affected arterial branch on exam.
Practical Advice:
Anyone experiencing sudden, unexplained vision loss should seek emergency eye care immediately. Quick action improves outcomes and may help identify other life-threatening vascular conditions.
Medical and Pharmacological Therapies for BRAO
There is no universally accepted, proven therapy to reverse vision loss after BRAO, but early interventions aim to restore retinal blood flow, minimize damage, and address systemic risks.
Immediate (Acute) Management
- Ocular Massage: Gentle pressure on the closed eye may dislodge an embolus.
- Reduction of Intraocular Pressure (IOP):
- Medications like acetazolamide or topical pressure-lowering drops.
- Anterior chamber paracentesis (fluid removal) may be considered in emergent settings.
- Breathing into a Paper Bag: Increases carbon dioxide and may dilate retinal arteries.
Systemic Assessment and Risk Reduction
- Antiplatelet agents: Low-dose aspirin or other antithrombotics to prevent further embolic events.
- Cardiac and Carotid Workup:
- Echocardiogram, carotid Doppler, and cardiac rhythm monitoring to detect embolic sources.
- Blood Pressure and Cholesterol Control:
- Managing hypertension and hyperlipidemia is critical for future stroke and vascular event prevention.
- Glucose Management:
- Tight control in diabetic patients reduces further vascular complications.
Pharmacological Therapies Under Study
- Thrombolytics: Limited evidence for intra-arterial or intravenous clot-dissolving drugs, mostly experimental and used in select, time-sensitive cases.
- Neuroprotective agents: Still investigational but under study for retinal ischemia.
Practical Advice:
After an acute BRAO, patients should have a full systemic vascular workup. Strictly follow your doctor’s instructions about blood pressure, cholesterol, and lifestyle modifications to minimize future risk.
Surgical and Interventional Management Strategies
While most management of BRAO is medical, certain interventional and surgical approaches are being explored, particularly in severe or refractory cases.
Key Interventional Approaches
- Anterior Chamber Paracentesis:
- Performed to rapidly reduce IOP in acute settings. This procedure is only effective if done within a few hours of onset and carries some risks.
- Retinal Artery Cannulation and Thrombolysis:
- A highly specialized, experimental micro-surgical technique to directly inject clot-dissolving agents into the blocked artery. Currently limited to research settings.
Laser Therapies
- Nd\:YAG Laser Embolysis:
- Used in rare cases to break up visible emboli in the retinal arteries, with some reported success.
- Risks include retinal hemorrhage and damage, so this is not routine care.
Surgical Management of Complications
- Vitrectomy:
- May be considered if BRAO is complicated by retinal neovascularization or vitreous hemorrhage.
- Panretinal Photocoagulation:
- Laser treatment to prevent further complications in eyes at high risk for neovascularization.
Risks and Considerations
- Many interventions are only effective if performed within hours of symptom onset.
- The potential for complications means these approaches are used with caution and only in selected cases.
Practical Advice:
Discuss the risks and benefits of any proposed surgical or interventional procedure thoroughly with your eye specialist, especially considering the short time window for effective therapy.
Cutting-Edge Innovations and Diagnostic Progress
Recent years have brought new technologies to the forefront, offering hope for earlier detection and more effective management of BRAO and its systemic implications.
Advances in Diagnostics
- Optical Coherence Tomography Angiography (OCTA):
- Non-invasive imaging that maps retinal blood flow in exquisite detail, helping identify and monitor occlusions.
- AI and Machine Learning:
- Deep learning algorithms now assist in detecting subtle retinal changes and stratifying patient risk for future vascular events.
- Comprehensive Systemic Screening:
- Multidisciplinary “stroke teams” are now more involved in care, recognizing the eye as a window into systemic vascular health.
Therapeutic Innovations
- Intra-arterial Thrombolysis:
- Refinement of techniques and drug delivery methods continues, with new trials underway.
- Neuroprotection and Regeneration:
- Stem cell therapies, neuroprotective agents, and retinal implants are being explored for future vision rescue and rehabilitation.
Integration of Telemedicine
- Rapid triage and remote ophthalmic imaging support urgent diagnosis and management, especially in rural or underserved areas.
Practical Advice:
Ask your care team about the latest diagnostic tools—advanced imaging can clarify your situation and guide therapy. For ongoing monitoring, consider digital platforms and telemedicine as part of your long-term care plan.
Clinical Trials and Emerging Directions
Ongoing and planned clinical trials are paving the way for major advances in both treatment and prevention of BRAO, with a focus on acute rescue therapies and long-term vascular risk reduction.
Current Clinical Trials
- Thrombolytic Therapy Trials:
- Studies are assessing the safety and efficacy of clot-busting drugs administered systemically or directly into the retinal arteries.
- Neuroprotection Trials:
- Agents that may shield retinal nerve tissue from ischemic injury are under investigation.
- Artificial Intelligence for Early Detection:
- Algorithms are being tested for population screening and acute triage.
Future Directions
- Personalized Medicine:
- Integrating genetic, systemic, and ocular data to predict and prevent BRAO in high-risk individuals.
- Regenerative Medicine:
- Stem cell and retinal implant research continues, aiming to restore vision lost to ischemia.
- Multispecialty Care Models:
- Closer collaboration between ophthalmology, neurology, and cardiology to prevent systemic complications after an ocular vascular event.
How Patients Can Get Involved
- Explore participation in clinical trials if eligible.
- Engage with patient advocacy groups for the latest updates and support.
Practical Advice:
Stay proactive: regular follow-up and lifestyle changes reduce your risk of future events. Ask your doctor about new research that may fit your unique situation.
Frequently Asked Questions
What is the main cause of branch retinal artery occlusion?
BRAO is most commonly caused by an embolus, such as a cholesterol plaque or blood clot, that blocks blood flow in a small retinal artery. Risk factors include atherosclerosis, high blood pressure, diabetes, and heart disease.
How is branch retinal artery occlusion treated?
There’s no single proven treatment, but immediate interventions include ocular massage and lowering eye pressure. Long-term, management focuses on systemic risk factors and monitoring for complications. Experimental therapies may be available in clinical trials.
What are the symptoms of BRAO?
The hallmark symptom is sudden, painless loss of vision or a partial visual field defect—often described as a “curtain” blocking part of the view. Some may notice episodes of transient vision loss beforehand.
Can vision recover after BRAO?
Some people experience partial improvement in vision, especially if treatment is started quickly, but most have some degree of permanent visual field loss. Prompt care offers the best chance for visual recovery.
What is the long-term prognosis after BRAO?
While some vision may return, most people have lasting visual field loss. Systemic vascular evaluation and management are crucial, as BRAO is a warning sign for increased risk of heart attack or stroke.
Is surgery needed for BRAO?
Surgery is rarely needed and only considered in select, severe cases or for managing complications. Most care is medical and focused on systemic risk reduction.
How can I prevent BRAO or a recurrence?
Control blood pressure, cholesterol, and blood sugar, avoid smoking, and follow your doctor’s advice for heart and vascular health. Early detection and prompt treatment of vascular risk factors are essential.
Disclaimer:
This article is for informational purposes only and should not be taken as medical advice. Always consult your healthcare professional for personal recommendations and treatment.
If you found this guide valuable, please share it with your friends and followers on Facebook, X (formerly Twitter), or any social media platform. Your support helps us continue to bring trusted health information to those who need it!






