A posterior subcapsular cataract (PSC) is a type of cataract that develops at the back of the lens, immediately in front of the posterior capsule. This specific location has a significant impact on vision, often more than other types of cataracts. PSCs typically appear as a cloudy or opaque area that blocks the path of light to the retina, resulting in blurred vision, glare, and difficulty seeing in bright light or reading. PSCs, unlike other cataracts, can progress quickly, impairing vision in as little as a few months.
Posterior subcapsular cataracts are frequently associated with risk factors such as prolonged corticosteroid use, diabetes, trauma, or a history of radiotherapy. They are also more common in younger people than other types of cataracts. PSC symptoms frequently include a disproportionate impact on near vision compared to distance vision, increased sensitivity to bright lights, and difficulty performing activities that require fine visual detail.
A comprehensive eye examination, including slit-lamp biomicroscopy, allows the ophthalmologist to see the back of the lens where the cataract forms. Recognizing PSC’s distinct characteristics and rapid progression is critical for timely and effective management, so both patients and healthcare providers must be aware of and understand this condition.
Posterior Subcapsular Cataract Care Strategies
Because there are no medical treatments that can reverse or halt cataract formation, the primary goal of managing posterior subcapsular cataracts is to improve vision through surgical intervention. Cataract surgery is a highly effective and common procedure that involves removing the cloudy lens and replacing it with an artificial intraocular lens (IOL).
Phacoemulsification is the standard surgical procedure for cataract removal. This procedure uses ultrasonic vibrations to emulsify the cataractous lens, which is then aspirated from the eye via a small incision. When compared to older methods, phacoemulsification offers faster recovery, smaller incisions, and fewer surgical complications. Once the cataract has been removed, an artificial intraocular lens is inserted to restore vision. These lenses come in a variety of styles, including monofocal, multifocal, and toric lenses, each designed to meet specific visual needs and preferences.
For patients with PSC, the choice of intraocular lens is critical. While multifocal lenses reduce the need for glasses, they may exacerbate glare and halos, which are already prevalent in PSC. As a result, monofocal lenses, which provide clear vision at a single distance, are frequently chosen to ensure optimal postoperative visual outcomes with minimal visual disturbances.
In cases where PSC is detected early and vision impairment is minimal, non-surgical treatment may include regular monitoring and updating eyeglass prescriptions to temporarily improve vision. However, due to the rapid progression of PSC, surgery is frequently required sooner than with other types of cataracts.
Preoperative evaluation and patient counseling are critical components of the treatment regimen. Patients should be informed about the risks and benefits of cataract surgery, the various types of IOLs available, and realistic postoperative vision expectations. Postoperative care includes anti-inflammatory and antibiotic eye drops to prevent infection and inflammation, as well as regular follow-up visits to monitor healing and visual outcomes.
Overall, while surgical treatment for PSC is highly effective, the condition’s rapid progression necessitates early intervention to avoid significant vision loss and maintain quality of life.
Innovative Treatment Options for Posterior Subcapsular Cataracts
The field of posterior subcapsular cataract treatment has made significant progress, thanks to advances in surgical techniques, intraocular lens technology, and postoperative care. These cutting-edge developments are transforming PSC management by improving visual outcomes and increasing patient satisfaction.
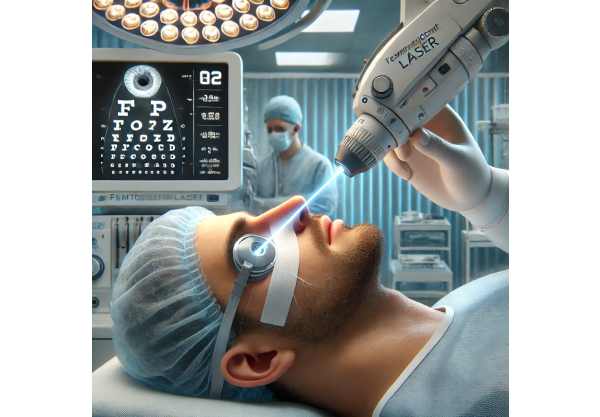
Femtosecond Laser Assisted Cataract Surgery (FLACS)
Femtosecond laser-assisted cataract surgery (FLACS) marks a significant advancement in cataract surgery. This cutting-edge technology employs a femtosecond laser to perform critical steps in the cataract procedure with unparalleled precision and accuracy. FLACS can make corneal incisions, perform capsulorhexis (the removal of the anterior lens capsule), and fragment the lens, which reduces the need for ultrasonic energy during phacoemulsification. This reduces surgical trauma and inflammation, resulting in faster recovery and better visual outcomes.
FLACS is especially useful for PSC patients due to its precision. The laser can create a perfectly centered and sized capsulorhexis, allowing for optimal positioning of the intraocular lens, which is critical for achieving the best visual results. Furthermore, the laser’s ability to soften and fragment the dense posterior subcapsular cataract lowers the risk of complications while increasing the overall safety and efficacy of the surgery.
Premium Intraocular Lenses
The development of premium intraocular lenses (IOLs) has transformed cataract surgery, giving patients better visual performance and reducing their reliance on glasses. These IOLs include multifocal, extended depth of focus (EDOF), and toric lenses, each with unique advantages.
Multifocal IOLs are intended to provide clear vision at a variety of distances, reducing the need for glasses following surgery. However, due to glare and halos in PSC patients, EDOF lenses are often preferred. EDOF lenses increase the range of clear vision, allowing for good intermediate and distance vision with minimal visual disturbances. This is especially useful for PSC patients, who are more susceptible to glare and halos.
Toric IOLs treat astigmatism, a common refractive error that can impair visual outcomes. Toric lenses can significantly improve uncorrected visual acuity for PSC patients with astigmatism, increasing overall surgical satisfaction.
Advanced Visualization and Guidance Systems
Intraoperative visualization and guidance systems have greatly improved the accuracy and safety of cataract surgery. Technologies like intraoperative aberrometry and digital imaging systems give surgeons real-time feedback, allowing them to make precise adjustments during the procedure.
Intraoperative aberrometry determines the refractive power of the eye during surgery, allowing for precise selection and positioning of the intraocular lens. This is especially important for PSC patients, as precise IOL placement is critical for the best visual outcomes. Digital imaging systems, such as optical coherence tomography (OCT) built into surgical microscopes, provide detailed, real-time visualization of the eye’s structures, allowing surgeons to perform complex maneuvers with confidence.
Improved postoperative care
Postoperative care is an important part of successful cataract surgery, and advances in this field are improving patient outcomes and satisfaction. Sustained-release drug delivery systems, such as intracanalicular inserts, regulate the release of anti-inflammatory and antibiotic medications, reducing the need for frequent eye drops and improving patient compliance.
Additionally, anti-VEGF (vascular endothelial growth factor) agents are being investigated in postoperative care to reduce the risk of cystoid macular edema (CME), a potential complication of cataract surgery. Early research suggests that these agents can effectively prevent CME, resulting in a smoother recovery and improved visual outcomes.
Artificial Intelligence, Machine Learning
Artificial intelligence (AI) and machine learning are becoming more widely used in ophthalmology, including cataract surgery. AI algorithms can analyze large datasets to predict surgical outcomes, optimize IOL selection, and help detect complications. These technologies improve the surgeon’s ability to provide personalized and precise treatment, resulting in better overall patient care.
Machine learning models can also help with preoperative planning by predicting the best IOL power and type for each patient based on their unique characteristics. This personalized approach ensures that each patient receives the best possible IOL, maximizing visual outcomes and satisfaction.
Telemedicine & Remote Monitoring
The COVID-19 pandemic has accelerated the adoption of telemedicine and remote monitoring technologies, creating new opportunities for post-operative care and patient follow-up. Telemedicine platforms enable virtual consultations, allowing patients to receive expert care in the comfort of their own homes. This is especially useful for PSC patients, who may need frequent follow-up visits.
Remote monitoring tools, such as smartphone apps and wearable devices, can track postoperative outcomes, medication adherence, and symptom development in real time. These technologies provide valuable data to healthcare providers, allowing for timely interventions and personalized care plans.
Future Prospects: Gene Therapy and Regenerative Medicine
Looking ahead, gene therapy and regenerative medicine have promising applications in the treatment of cataracts, including PSC. Researchers are investigating the possibility of using gene therapy to prevent or reverse cataract formation by targeting the molecular pathways that cause lens opacification. Early research in animal models has yielded promising results, paving the way for future clinical trials.
Regenerative medicine approaches, such as using stem cells to regenerate the lens, are also under investigation. These techniques aim to restore the clarity and function of the natural lens, potentially providing a cure for cataracts without the use of artificial lenses. While still in the experimental stage, these advancements represent a significant step toward the future of cataract treatment.






