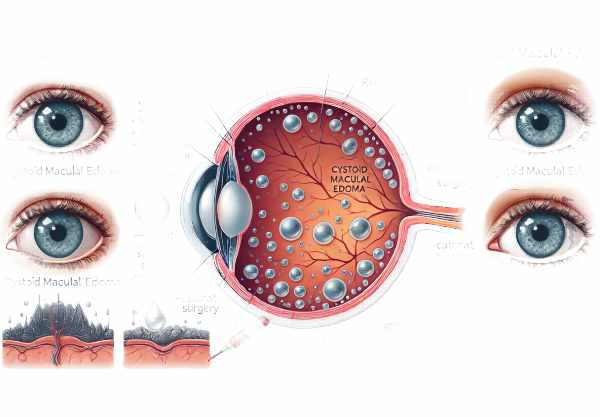
What is Cystoid Macular Edema?
Cystoid macular edema (CME) is a condition in which fluid accumulates in the macula, the central part of the retina responsible for detailed vision. This fluid accumulates in cyst-like spaces, causing swelling and distortion of the macula, potentially impairing central vision. CME is linked to a variety of ocular and systemic conditions, including diabetic retinopathy, retinal vein occlusion, uveitis, and complications from cataract surgery. Fluid disrupts the normal retinal architecture, resulting in symptoms such as blurred vision, decreased visual acuity, and difficulty performing tasks that require fine detail. Understanding CME is critical for early detection and effective treatment to avoid permanent vision loss.
Cystoid Macular Edema Insights
Cystoid macular edema (CME) is a complex condition with many underlying causes, pathophysiological mechanisms, and clinical implications. To fully understand the complexities of CME, it is necessary to investigate its pathophysiology, associated risk factors, epidemiology, clinical manifestations, and potential complications.
Pathophysiology
The pathophysiology of CME involves the disruption of the blood-retina barrier, which causes fluid to leak into the macular region. This leakage causes cystoid spaces to form in the retina. Several mechanisms may contribute to this process:
- Inflammation: Inflammatory mediators like prostaglandins and cytokines play an important role in disrupting the blood-retina barrier. Conditions such as uveitis and post-surgical inflammation (particularly following cataract surgery) can cause the release of these mediators, resulting in fluid accumulation in the macular.
- Vascular Leakage: Vascular endothelial growth factor (VEGF) is a powerful regulator of vascular permeability. Elevated levels of VEGF in conditions such as diabetic retinopathy and retinal vein occlusion cause increased vascular permeability and fluid leakage into the macula.
- Mechanical Factors: Structural changes in the retina, such as epiretinal membranes or vitreomacular traction, can cause CME by physically distorting the macula and disrupting normal fluid dynamics.
Risk Factors
Several factors raise the likelihood of developing CME, including:
- Diabetes Mellitus: Diabetic retinopathy is a major cause of CME. Chronic hyperglycemia causes microvascular damage and increases VEGF production, resulting in macular edema.
- Retinal Vein Occlusion: Blockage of the retinal veins results in increased hydrostatic pressure and fluid leakage into the macula.
- Ocular Surgery: Cataract surgery, especially complicated procedures, is a common cause of CME due to postoperative inflammation.
- Uveitis: Inflammatory conditions in the eye can cause the release of inflammatory mediators, which contribute to CME.
- Age-related Macular Degeneration (AMD): The neovascular type of AMD can cause leakage and fluid accumulation in the macula.
Epidemiology
CME is a fairly common condition, especially in patients with underlying risk factors like diabetes and retinal vascular disorders. Post-surgical CME is also common, with different rates depending on the type of surgery and patient population. Diabetic macular edema, a type of CME, affects a large number of diabetic patients and is the leading cause of vision loss in this population.
Clinical Manifestations
The primary symptom of CME is a gradual decrease in central vision. Patients frequently report blurred or distorted vision, making it difficult to perform fine detail tasks like reading or recognizing faces. Other symptoms may include:
- Metamorphopsia is a visual distortion in which straight lines appear wavy or bent.
- Micropsia: Objects can appear smaller than they are.
- Scotomas: Small areas of visual field loss may develop in the central vision.
Potential Complications
If left untreated, CME can cause permanent structural damage to the retina and significant, irreversible vision loss. Chronic CME can cause cystic spaces in the retina, resulting in retinal thinning and atrophy. Furthermore, persistent macular edema can predispose patients to the formation of epiretinal membranes and macular holes, complicating the clinical picture and making treatment more difficult.
Effects on Quality of Life
CME has a significant impact on a patient’s quality of life. CME-related central vision loss and visual distortions can disrupt daily activities such as reading, driving, and face recognition. This can lead to a loss of independence and a higher risk of depression and anxiety. As a result, timely recognition and management of CME are critical for maintaining quality of life and avoiding long-term visual impairment.
Preventive Measures for CME
- Control Blood Sugar Levels: – It is critical for diabetic patients to keep their blood sugar levels stable. Regular monitoring and adherence to prescribed medications can help prevent diabetic retinopathy, which is a major cause of CME.
- Manage Blood Pressure: – Hypertension can worsen conditions like retinal vein occlusion. Regularly monitoring and controlling blood pressure lowers the risk of vascular complications, which can lead to CME.
- Regular eye exams are crucial, especially for those with risk factors like diabetes, hypertension, or previous ocular surgery. Early detection of retinal changes can stop the progression of CME.
- Follow post-surgical care instructions and follow-up appointments to prevent CME.
- Anti-Inflammatory Medications: Use prescribed anti-inflammatory medications to control inflammation and reduce the risk of CME in individuals with inflammatory conditions like uveitis.
- Healthy Lifestyle Choices: – Maintaining a healthy lifestyle, such as eating a balanced diet with antioxidants, exercising regularly, and quitting smoking, can improve eye health and lower the risk of CME.
- Use Protective Eyewear: – Wearing appropriate eyewear can protect the eyes from trauma and UV exposure, reducing the risk of CME.
- Monitor Vision Changes: – Be aware of any vision changes, including blurriness, distortion, or difficulty focusing. Promptly reporting these symptoms to an eye care professional can result in earlier intervention and better outcomes.
- Educate on Symptoms: Educating at-risk populations about CME symptoms can prompt early consultation with eye care professionals, resulting in timely diagnosis and treatment.
- Effectively manage comorbid conditions, such as cardiovascular disease and systemic inflammatory disorders, to reduce the risk of CME.
Diagnostic methods
To accurately detect and monitor cystoid macular edema (CME), a combination of clinical examination and advanced imaging techniques is required.
Clinical Examination
- Visual Acuity Test: This test uses an eye chart to determine the sharpness of a patient’s vision. Patients with CME frequently exhibit a decline in central visual acuity.
- Amsler Grid: – Detects visual distortions like wavy lines or blank spots, which indicate macular involvement.
Imaging Techniques
- Optical Coherence Tomography (OCT):
- OCT is considered the gold standard for diagnosing CME. This non-invasive imaging technique produces high-resolution cross-sectional images of the retina, allowing for precise visualization of the cystoid spaces and macular thickness. Both initial diagnosis and treatment response monitoring rely heavily on OCT.
- fluorescein angiography (FA):
FA entails injecting a fluorescent dye into the bloodstream and taking a series of retinal photographs. It aids in the identification of leakage and capillary non-perfusion, both of which are common in conditions that lead to CME. FA is especially useful in distinguishing CME from other macular diseases. - Indocyanine Green Angiogram (ICGA):
- ICGA is similar to FA, but it uses indocyanine green dye. It is useful for visualizing deeper choroidal circulation and detecting vascular abnormalities that contribute to CME.
- Fundus Photography: – Color fundus photography captures a detailed image of the retina and can detect macular edema. It is useful for establishing baselines and tracking changes over time.
Electrophysiological tests
- Electroretinography (ERG) measures the retina’s electrical responses to light stimuli. It can provide information on retinal function and aid in the identification of generalized retinal dysfunction that may be associated with CME.
Innovative Diagnostic Techniques
- OCT Angiogram (OCTA):
- OCTA is a more advanced form of OCT that visualizes blood flow in the retina and choroid without the use of dye. It produces detailed images of the retinal and choroidal vasculature, allowing for the evaluation of capillary perfusion and areas of non-perfusion associated with CME.
- Adaptive Optics (AO): AO is a cutting-edge technology that produces ultra-high-resolution images of the retina. It enables the visualization of individual photoreceptors and fine retinal structures, providing insights into the microstructural changes caused by CME.
Lab Tests
- Blood Tests: – Comprehensive blood tests can detect systemic conditions like diabetes, hypertension, or inflammatory diseases that can lead to CME. Specific tests may include HbA1c for diabetes management, lipid profiles, and inflammatory markers.
Managing Cystoid Macular Edema
- Anti-inflammatory Medications: – Corticosteroids: Corticosteroids are commonly used to reduce inflammation caused by CME. They can be given as eye drops, oral medications, or intravitreal injections. Intravitreal injections are especially effective at delivering high doses of the drug directly to the site of inflammation.
Nonsteroidal Anti-inflammatory Drugs (NSAIDs) Topical NSAIDs are commonly used after surgery to prevent and treat CME by inhibiting the production of inflammatory mediators. - Anti-VEGF Therapy: Intravitreal injections of bevacizumab, ranibizumab, and aflibercept can reduce vascular permeability and fluid leakage. These treatments are especially effective in CME with diabetic retinopathy and retinal vein occlusion.
- Laser Photocoagulation: – Focal or grid laser photocoagulation can be used to treat retinal leakage in conditions such as diabetic macular edema. The laser causes burns, which seal leaking blood vessels and reduce fluid accumulation in the macula.
Innovative and Emerging Therapies
- Intravitreal Steroid Implants: Sustained-release steroid implants like Ozurdex and Iluvien offer long-term inflammation control. These implants gradually release the drug over several months, reducing the number of injections and improving patient compliance.
- Neuroprotective Agents: These emerging therapies aim to protect retinal neurons from damage caused by chronic CME. Neuroprotective agents, such as brimonidine and others under investigation, are being studied for their ability to preserve vision.
- Gene Therapy: – Although still in the experimental stage, gene therapy shows promise for treating underlying genetic conditions that cause CME. This approach, which corrects genetic defects, aims to provide a long-term solution to retinal disease.
- Micropulse Laser Therapy: – Micropulse laser therapy uses short, repetitive pulses to minimize thermal damage to the retina and effectively treat CME. This technique is gaining popularity due to its safety and effectiveness.
Long-Term Management.
- Regular Monitoring: Continuous follow-up with OCT and other diagnostic tools is necessary to monitor treatment response and adjust therapy as needed.
- Combination Therapies: – Combining treatment modalities, such as anti-VEGF agents with corticosteroids or laser therapy, can improve therapeutic response and address multiple pathways in CME.
Trusted Resources
Books
- “Retina” by Stephen J. Ryan
- “The Retina Atlas” by Lawrence A. Yannuzzi
- “Medical Retina” by Frank G. Holz and Richard F. Spaide






