What is homocystinuria?
Homocystinuria is a rare inherited metabolic disorder marked by an excess of homocysteine in the blood and urine. This condition is caused by a deficiency in one of several enzymes involved in the methionine metabolism. Ectopia lentis, or lens dislocation, is a significant complication of homocystinuria in which the eye’s lens becomes displaced. If not treated properly, this ocular manifestation can cause significant visual impairment. Understanding the underlying causes and effects of homocystinuria is critical for timely diagnosis and treatment.
Comprehensive Investigation of Homocystinuria.
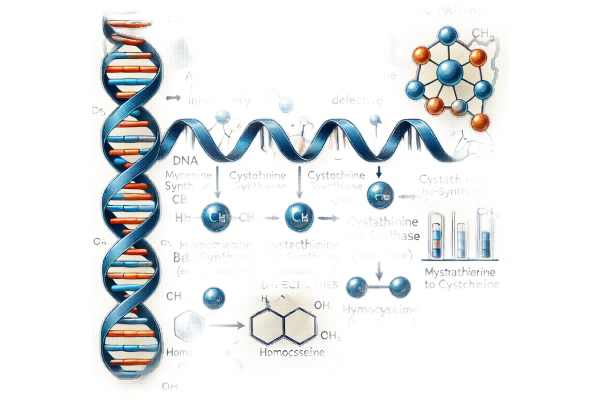
Homocystinuria is an autosomal recessive disorder characterized by a deficiency in the enzyme cystathionine beta-synthase (CBS), which is required for the conversion of homocysteine to cystathionine. Other rarer forms of the disease are caused by enzyme deficiencies in methionine synthase or methylenetetrahydrofolate reductase (MTHFR). The absence of these enzymes causes an accumulation of homocysteine and its metabolites, which can be harmful to various tissues.
Genetic Basis
Homocystinuria is inherited in an autosomal recessive pattern, which means that affected people receive two copies of the defective gene, one from each parent. Mutations in the CBS gene are the most common cause of homocystinuria. These mutations can cause complete or partial loss of enzyme activity, resulting in varying disease severity.
Pathophysiology
Elevated levels of homocysteine and its derivative, homocystine, cause a variety of clinical symptoms due to their effects on connective tissue, the cardiovascular system, and the central nervous system. Excess homocysteine can disrupt collagen cross-linking, which is required for the structural integrity of connective tissues. This interference can cause abnormalities in bones, skin, and eyes.
Ocular manifestations
Ectopia lentis, or lens dislocation, is a defining feature of homocystinuria. The lens is typically displaced downward and inward, as opposed to the upward and outward displacement seen in Marfan syndrome, which is also associated with lens dislocation.
- Lens Dislocation: Dislocating the lens can cause significant visual disturbances. If the lens obstructs the visual axis, patients may experience blurred or double vision, as well as sudden loss of vision. The dislocated lens can also cause refractive errors such as myopia (nearsightedness) and astigmatism.
- Other Ocular Features: Patients with homocystinuria may also have glaucoma (high intraocular pressure), retinal detachment, or optic atrophy. These complications increase the risk of visual impairment.
Systematic Manifestations
In addition to ocular symptoms, homocystinuria affects several organ systems:
- Skeletal Abnormalities: Patients frequently have a tall, thin build with long limbs and fingers (arachnodactyly), which is similar to Marfan syndrome. Other skeletal manifestations include osteoporosis, scoliosis, and pectus excavatum (a sunken chest).
- Cardiovascular Complications: High levels of homocysteine are a risk factor for thromboembolic events like deep vein thrombosis, pulmonary embolism, and stroke. These cardiovascular issues are a major cause of morbidity and mortality in people with homocystinuria.
- Neurological Issues: Untreated patients often have intellectual disability, developmental delays, and psychiatric disorders like anxiety and depression. Seizures and movement disorders may also occur.
- Other Features: Patients may have fair skin and hair due to impaired melanin synthesis, as well as frequent fractures as a result of osteoporosis.
Diagnosis and Differential Diagnosis
Homocystinuria is typically diagnosed using a combination of clinical, biochemical, and genetic tests. It is critical to distinguish homocystinuria from other conditions with similar symptoms, such as Marfan syndrome and connective tissue disorders.
- Clinical Evaluation: A thorough clinical examination may reveal distinguishing features such as lens dislocation, skeletal abnormalities, and other systemic signs.
- Biochemical Testing: Elevated levels of homocysteine in the blood and urine suggest homocystinuria. Methionine levels can also be measured, as they are typically elevated in patients with CBS deficiency.
- Genetic Testing: Confirmatory testing identifies mutations in the CBS gene or other genes linked to homocystinuria. Carrier testing and prenatal diagnosis are both possible with genetic testing.
Management and Prognosis
Patients with homocystinuria benefit greatly from early diagnosis and appropriate treatment. Treatment strategies revolve around lowering homocysteine levels through dietary changes, vitamin supplementation, and, in some cases, enzyme replacement therapy.
- Dietary Management: A low-methionine diet supplemented with cysteine is commonly recommended. This diet reduces the substrate load for homocysteine formation.
- Vitamin Supplementation: High doses of pyridoxine (vitamin B6) can help with some cases of CBS deficiency, especially in patients who respond to B6. Folate and vitamin B12 supplements are also used to aid in the remethylation pathway of homocysteine metabolism.
- Betaine Therapy: Betaine can reduce homocysteine levels by promoting its conversion to methionine. This treatment is especially effective for patients who do not respond to pyridoxine.
- Regular Monitoring: Continuous monitoring of homocysteine levels, as well as regular ophthalmologic, cardiovascular, and neurological assessments, is critical for managing and mitigating the disease’s complications.
Diagnostic methods
Homocystinuria is accurately diagnosed using a combination of clinical, biochemical, and genetic tests. Early and accurate diagnosis is critical for successful treatment and avoiding complications.
Clinical Evaluation
A thorough clinical examination is the first step in diagnosing homocystinuria. Key components are:
- History and Physical Exam: A detailed patient history, including any family history of similar symptoms or consanguinity. The physical examination focuses on identifying distinguishing characteristics such as lens dislocation, skeletal abnormalities, and signs of thromboembolic events.
Biochemical Testing
Biochemical tests are critical for diagnosing homocystinuria.
- Plasma Homocysteine Levels: Homocystinuria is characterized by elevated plasma homocysteine levels. Fasting total homocysteine levels are commonly measured, with levels above 15 µmol/L considered elevated.
- Analysis Of Plasma Amino Acids Elevated methionine levels support a diagnosis of CBS deficiency. High-performance liquid chromatography (HPLC) is one method for analyzing amino acids.
- Urinary Homocysteine: Increased homocysteine excretion in urine (homocystinuria) can be detected qualitatively or quantitatively.
Genetic Testing
Genetic testing provides a definitive diagnosis and helps identify specific mutations.
- Gene Sequencing: The CBS gene is commonly sequenced to identify pathogenic mutations. Other genes, such as MTHFR and MTR, may be sequenced if CBS mutations are not discovered.
- ** Newborn Screening**: Some regions include homocystinuria in newborn screening programs, which use tandem mass spectrometry to detect elevated methionine and homocysteine levels in dried blood spots.
Imaging and Ophthalmological Examination
Ophthalmologic examination is necessary for detecting lens dislocation and other ocular manifestations.
- Slit-Lamp Examination: An ophthalmologist can detect ectopia lentis and evaluate other potential eye complications like glaucoma or retinal detachment.
- Imagery Studies: Additional imaging, such as echocardiography and bone densitometry, may be required to determine cardiovascular and skeletal involvement.
Treatment
The treatment of homocystinuria focuses on lowering blood homocysteine levels in order to prevent complications and improve overall health. Early diagnosis and intervention are critical for successful condition management.
Standard Treatment Options:
- Dietary Management: A low-methionine diet supplemented with cysteine is commonly recommended. This diet lowers the substrate for homocysteine production. Patients should avoid high-protein foods and instead consume special medical formulas designed to provide adequate nutrition without excessive methionine.
- Vitamin Supplementation: High doses of pyridoxine (vitamin B6) are effective in some patients with CBS deficiency, especially those who respond to pyridoxine. Vitamin B6 improves the residual activity of the CBS enzyme. Furthermore, folate and vitamin B12 supplementation promotes the remethylation pathway of homocysteine metabolism, which helps to lower homocysteine levels.
- Betaine Therapy: Betaine acts as a methyl donor, promoting the conversion of homocysteine to methionine and thus lowering homocysteine levels. This treatment is especially helpful for patients who do not respond to pyridoxine supplements.
- Regular Monitoring and Supportive Care: Continuous monitoring of homocysteine levels is required to ensure treatment efficacy and adjust therapy as needed. Regular ophthalmologic exams, cardiovascular evaluations, and neurological assessments are critical for managing and detecting complications early.
Innovative and Emerging Therapies: 1. Gene Therapy Advances in gene therapy offer hope for more effective treatment of homocystinuria. Researchers are working to develop techniques to correct the genetic mutations that cause the disorder, which could provide a long-term solution by restoring normal enzyme function.
- Enzyme Replacement Therapy: Enzyme replacement therapy, like other treatments for metabolic disorders, aims to replace missing or deficient enzymes, restoring metabolic pathways to normal. This method is still in the experimental stage for homocystinuria.
- New Pharmacological Agents: Researchers are looking into new drugs that can better regulate homocysteine metabolism. These agents seek to increase the activity of residual enzymes or facilitate alternative metabolic pathways in order to reduce homocysteine accumulation.
- CRISPR-Cas9 Technology: Gene editing technologies such as CRISPR-Cas9 have the potential to directly correct genetic mutations in patients with homocystinuria. While still experimental, these approaches may provide a permanent cure by precisely targeting and repairing defective genes.
Multidisciplinary Approach
Geneticists, dietitians, ophthalmologists, cardiologists, and neurologists must all collaborate to manage homocystinuria effectively. Coordinated care allows for comprehensive management of the condition and its complications.
By combining dietary management, vitamin supplementation, innovative therapies, and regular monitoring, healthcare providers can significantly improve outcomes for patients with homocystinuria, lowering the risk of complications and improving quality of life.
Tips to Avoid Homocystinuria-Related Lens Dislocation: 1. Genetic Counseling Individuals with a family history of homocystinuria should seek genetic counseling to better understand their risk and consider genetic testing. Early detection enables timely intervention and management.
- Early Diagnosis and Treatment: Prompt diagnosis via newborn screening or early clinical evaluation can result in early treatment, lowering the risk of complications like lens dislocation.
- Adherence to Dietary Management: A low-methionine diet prescribed by a dietitian can effectively manage homocysteine levels. Regular consultations with a nutritionist are required to ensure nutritional adequacy.
- Regular Monitoring of Homocysteine Levels: Lifelong monitoring of homocysteine levels is critical for adjusting treatment plans and avoiding complications. Patients should undergo regular blood tests to monitor their progress.
- Consistent Vitamin and Supplement Intake: Following prescribed vitamin supplementation, particularly pyridoxine, folate, and vitamin B12, is critical for managing homocystinuria and avoiding related complications.
- Routine Ophthalmologic Exams: Regular eye exams can detect early signs of lens dislocation and other ocular problems. Early intervention can help to prevent significant visual impairment.
- Cardiovascular Health Monitoring: Regular cardiovascular screenings are required to detect thromboembolic events, which are common in homocystinuria. Preventive measures and treatments can be used as needed.
- Neurological and Developmental Support: Monitoring for neurological complications and providing developmental support can aid in the management and mitigation of the cognitive and psychiatric effects of homocystinuria.
Individuals at risk for homocystinuria and related lens dislocation can manage their condition and avoid serious complications by adhering to these best practices.
Trusted Resources
Books
- “Metabolic and Genetic Eye Disorders: A Diagnostic Guide” by Derek Y. Kunimoto and Narsing A. Rao
- “Inherited Metabolic Diseases: A Clinical Approach” by Georg F. Hoffmann, Johannes Zschocke, and William L. Nyhan
- “Pediatric Ophthalmology, Neuro-Ophthalmology, Genetics” by Birgit Lorenz and Catherine A. B. Jackson






