What is Hordeolum?
Hordeolum, also known as a stye, is an acute infection or inflammation of the oil glands in the eyelid that causes a painful, red lump near the edge of the eye. This condition is caused by a bacterial infection, usually Staphylococcus aureus. Hordeola can affect the Zeis or Moll glands externally or the meibomian glands internally. While most styes are self-limiting, they can cause significant discomfort and, in some cases, lead to complications if not treated properly.
Detailed Look at Hordeolum
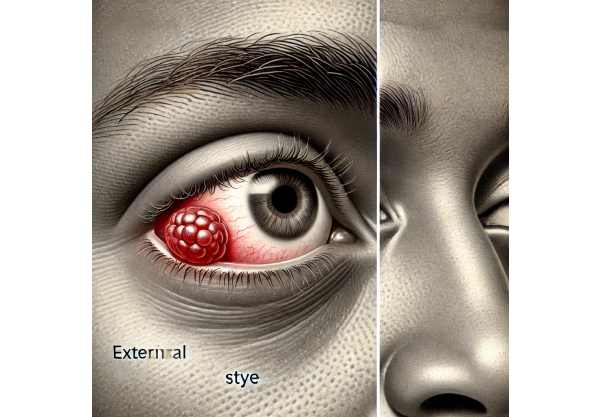
Hordeolum, also known as stye, is a localized infection or inflammation of the sebaceous glands on the eyelids. This condition is identified by a painful, swollen, red bump on the eyelid that resembles a small pimple or boil. Hordeola are classified into two types: external and internal, depending on the location of the affected gland.
Types of Hordeolum
- External Hordeolum: This type affects the Zeis or Moll glands, which are found at the base of the eyelashes. An external hordeolum is a small, red, tender swelling on the eyelid margin, often with a visible yellow spot in the center that indicates the presence of pus.
- Internal Hordeolum: This type affects the meibomian glands located within the tarsal plate of the eyelid. An internal hordeolum appears as a more diffuse swelling of the eyelid; while the lump may not be as visible as an external hordeolum, it can be palpated and is typically more painful.
Pathophysiology
Hordeolum pathogenesis is typically associated with bacterial infection, most commonly caused by Staphylococcus aureus. The infection may be caused by an obstruction in the gland’s duct, resulting in the accumulation of secretions that promote bacterial growth. This causes an inflammatory response characterized by redness, swelling, heat, and pain.
Risk Factors
Several factors can predispose people to develop hordeola.
- Poor Eyelid Hygiene: Failure to clean the eyelid margins thoroughly can result in the accumulation of debris and bacteria.
- Contact Lens Use: Improper handling and hygiene of contact lenses can lead to infection.
- Blepharitis: Chronic inflammation of the eyelid margins can lead to hordeola.
- Rosacea: This skin condition is linked to meibomian gland dysfunction, which increases the risk of developing styes.
- Immunosuppression: Conditions or medications that weaken the immune system can make you more susceptible to infections.
Clinical Manifestations
Hordeolum exhibits a distinct set of symptoms:
- Localized Pain: The affected area is usually sensitive to touch.
- Swelling and Redness: The eyelid swells, turns red, and warms up.
- Visible Lump: A palpable lump is frequently present, with the external hordeola forming a more visible bump on the eyelid margin.
- Tearing and Photophobia: You may experience increased tearing and sensitivity to light.
- Foreign Body Sensation: Patients frequently report a sensation in their eye.
Complications
While most hordeola resolve spontaneously, complications may occur if the infection spreads or is not adequately treated.
- Chalazion: A chronic, non-infectious granuloma can develop if an internal hordeolum does not resolve, resulting in a painless lump.
- Preseptal Cellulitis: The infection can spread to the surrounding tissues of the eyelid, resulting in increased redness, swelling, and pain.
- Recurrence: Hordeola are common, especially in people who have underlying conditions such as blepharitis or rosacea.
Differential Diagnosis
Hordeolum must be distinguished from other comparable eyelid conditions:
- Chalazion: Unlike hordeolum, chalazion is a chronic, painless granuloma caused by the blockage of a meibomian gland that is not infected.
- Dacryocystitis: Inflammation of the lacrimal sac can cause swelling in the inner corner of the eye, but it is usually accompanied by tearing and discharge.
- Preseptal Cellulitis: This condition causes diffuse eyelid swelling and redness that is not limited to a single gland.
- Eyelid Tumors: Benign or malignant tumors can appear as eyelid lumps, necessitating additional testing to rule out cancer.
Prognosis
Hordeolum has an excellent prognosis, with the majority of cases resolving spontaneously or with minimal intervention. However, recurrences are common, and people with underlying conditions like blepharitis or rosacea may have multiple episodes. Proper eyelid hygiene and management of predisposing factors can help to reduce the number of recurrences.
Diagnostic Approaches for Hordeolum
Hordeolum is primarily diagnosed clinically, using characteristic symptoms and physical examination findings. However, specific diagnostic methods can be used to confirm the diagnosis and rule out other possibilities.
Clinical Examination
A thorough clinical examination by an ophthalmologist or optometrist includes the following:
- Visual Inspection: Examine the eyelid to identify the distinctive red, swollen lump. External hordeola are usually visible along the eyelid margin, whereas internal hordeola may necessitate eversion of the eyelid for examination.
- Palpation: Gently palpate the eyelid to determine tenderness and the presence of a firm lump.
- Slit-Lamp Examination: A slit-lamp biomicroscope allows for a thorough examination of the eyelid, eyelashes, and ocular surface, which aids in determining the type and extent of the hordeolum.
Differential Diagnosis
To ensure an accurate diagnosis, distinguish hordeolum from other similar conditions.
- Chalazion: Characterized by its chronic, painless nature. Unlike hordeola, which is acutely tender, chalazia are firm and typically not tender.
- Dacryocystitis: Swelling in the inner corner of the eye, often accompanied by tearing and discharge. Palpation of the lacrimal sac may reveal purulent material.
- Preseptal Cellulitis is distinguished by diffuse eyelid swelling and redness in the absence of a localized lump. Systemic symptoms such as fever may also exist.
Additional Tests
In most cases, additional tests are not required to diagnose hordeolum. However, if the condition recurs frequently or does not respond to treatment, additional investigation may be required:
- Culture and Sensitivity: Swabbing the area for bacterial culture can aid in determining the causative organism and guiding antibiotic therapy in persistent or recurring cases.
- Imagery Studies: In rare cases where deeper tissue involvement or atypical presentation is suspected, imaging studies such as ultrasound or MRI may be used to determine the severity of the infection.
Hordeolum Treatment Methods
Hordeolum treatment focuses primarily on symptom relief, infection resolution, and complication prevention. Most hordeolum cases resolve on their own within a week or two, but there are several treatment options available to help speed up recovery and alleviate discomfort.
Standard Treatment Options
- Warm Compresses: Applying a warm compress to the affected eyelid for 10-15 minutes, three to four times per day, promotes drainage and relieves pain and swelling. The warmth causes the stye to come to a head and drain naturally.
- Eyelid Hygiene: Proper eyelid hygiene is essential. Gently cleaning the eyelid margins with a mild, non-irritating soap or baby shampoo diluted in water can aid in debris removal and gland blockage prevention.
- Topical Antibiotics: If there is a significant bacterial infection or risk of spread, topical antibiotic ointments like erythromycin or bacitracin may be recommended. These ointments are applied directly to the affected area to help reduce bacterial growth.
- Oral Antibiotics: In cases of severe infection, recurrent hordeola, or associated cellulitis, oral antibiotics such as doxycycline or cephalexin may be required to control the infection and avoid complications.
- Pain Relief: Over-the-counter pain relievers like acetaminophen or ibuprofen can help with discomfort and inflammation.
- Incision and Drainage: If a hordeolum does not improve with conservative treatment and becomes a chronic problem, an ophthalmologist may perform a minor surgical procedure to lance and drain the stye. This procedure is typically performed with local anesthesia and provides immediate relief.
Innovative and Emerging Therapies
1) Laser Therapy: According to recent research, low-level laser therapy (LLLT) may help reduce inflammation and accelerate healing in cases of hordeolum. This non-invasive treatment directs light at specific wavelengths to the infected area, promoting tissue repair.
- Heat Therapy Devices: Newer, specialized devices for home use apply consistent and controlled heat to the eyelids. These devices may be more efficient and convenient than traditional warm compresses.
- Photodynamic Therapy: This novel approach uses a photosensitizing agent activated by light exposure to target and destroy bacterial cells, thereby reducing infection and inflammation.
- Botulinum Toxin Injections: Although still under study, botulinum toxin injections near the affected gland have shown promise in reducing chronic inflammation and preventing recurrences in some cases.
Healthcare providers can effectively manage hordeolum by using these treatment options, which provide symptom relief and prevent complications. Ongoing research into innovative therapies holds the promise of even more effective and convenient treatment options in the future.
Best Practices to Avoid Hordeolum
- Maintain Proper Eyelid Hygiene: Clean your eyelids on a regular basis with a mild, non-irritating cleanser or water-diluted baby shampoo. This helps to remove debris and bacteria that may clog the oil glands.
- Avoid Touching Your Eyes: Do not touch or rub your eyes with unwashed hands, as this can transfer bacteria to the eyelids and increase the risk of infection.
- Proper Contact Lens Care: Always wash your hands before handling contact lenses and follow the recommended cleaning and storage instructions. To avoid bacterial contamination, replace your lenses and cases on a regular basis.
- Remove Makeup Before Sleeping: Make sure all eye makeup, including mascara and eyeliner, is completely removed before going to bed. Using expired or shared makeup increases the risk of infection, so avoid these practices.
- Manage Blepharitis: If you have blepharitis, follow your doctor’s advice on how to manage this chronic condition, as it can increase your risk of developing hordeola.
- Use Warm Compresses Regularly: Applying warm compresses to the eyelids on a regular basis, even if you don’t have a stye, can help keep the oil glands working properly and prevent blockages.
- Boost Your Immune System: Lead a healthy lifestyle by eating a well-balanced diet, exercising regularly, and getting enough sleep. A strong immune system can help your body combat infections more effectively.
- Never Share Personal Items: Do not share towels, washcloths, or other personal items that come into contact with your face or eyes. This can help prevent the spread of bacteria and lower the risk of developing hordeola.
Following these preventive measures can significantly reduce your risk of developing hordeola and keep your eyes healthy.
Trusted Resources
Books
- “Ophthalmology: Expert Consult” by Myron Yanoff and Jay S. Duker
- “The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease” by Adam T. Gerstenblith and Laura Enyedi
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski and Brad Bowling






