What is primary intraocular lymphoma?
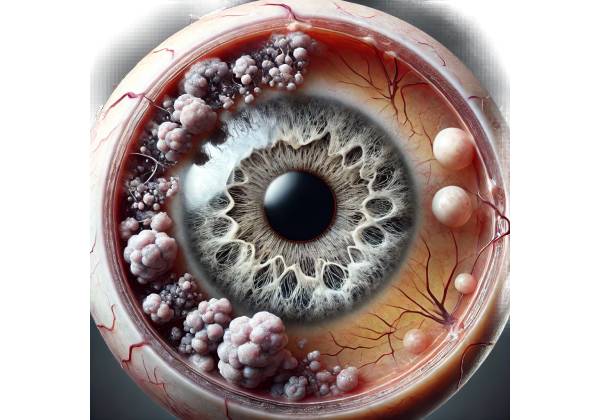
Primary intraocular lymphoma (PIOL) is a rare, malignant cancer that develops within the eye. It is a subtype of primary central nervous system lymphoma (PCNSL) that usually affects the retina, vitreous, and occasionally the optic nerve. PIOL is primarily a B-cell non-Hodgkin lymphoma, but T-cell lymphomas can occur, albeit infrequently.
PIOL is defined by the proliferation of malignant lymphoid cells in the eye, which causes a variety of ocular symptoms and complications. The disease frequently mimics other inflammatory eye conditions, such as uveitis, making diagnosis difficult and often delayed. Understanding the complexities of PIOL, including pathophysiology, risk factors, symptoms, and epidemiology, is critical for early detection and treatment.
Pathophysiology
The pathophysiology of PIOL is characterized by the infiltration of malignant lymphocytes into ocular tissues. These lymphocytes typically originate in the central nervous system (CNS) and spread to the eye via the optic nerve, though the exact mechanisms are unknown. The retina is the most common site of infiltration, closely followed by the vitreous humor. The optic nerve head and choroid are less common sites of involvement.
PIOL cells are typically of the B-cell lineage, expressing CD20, CD79a, and PAX5. They have clonal immunoglobulin gene rearrangements, which are detectable using molecular diagnostic techniques. In rare cases, PIOL can be T-cell derived, resulting in a different set of markers and clinical behavior.
The interaction between malignant lymphocytes and the ocular environment causes the release of various cytokines and inflammatory mediators. This causes chronic inflammation and tissue damage, which exacerbates the disease’s clinical manifestations.
Epidemiology
PIOL is an extremely rare condition, accounting for less than 1% of all ocular malignancies and only 1-2% of primary CNS lymphomas. It primarily affects adults, with the peak incidence occurring between the ages of 50 and 70. There is no significant gender bias, though some studies indicate a slight male advantage.
Because of its association with PCNSL, PIOL is common in immunocompromised people, such as those with acquired immunodeficiency syndrome (AIDS) and organ transplant recipients. However, it can also develop in immunocompetent patients, demonstrating that immune status is not the only determinant of disease occurrence.
Risk Factors
Several risk factors for PIOL have been identified, though these are not unique to this condition:
- Immunosuppression: Conditions that weaken the immune system, such as HIV/AIDS, organ transplantation, and long-term immunosuppressive drug use, raise the risk of developing PIOL.
- Age: The risk of PIOL increases with age, especially in people over 50.
- Genetic Predisposition: Although not fully understood, certain genetic mutations and familial predispositions may contribute to the development of PIOL.
- Chronic Inflammation: Prolonged ocular inflammation, such as chronic uveitis, has been proposed as a risk factor, but the exact relationship is unknown.
Clinical Presentation
The clinical presentation of PIOL is highly variable and often nonspecific, leading to frequent misdiagnosis as other ocular inflammatory conditions. Common symptoms include:
- Blurred Vision: One of the most common symptoms is blurred vision, which can be caused by vitreous haze, retinal involvement, or optic nerve infiltration.
- Floaters: Patients frequently report seeing floaters, which are small dark spots or shapes that move across their visual field. Cellular debris and inflammatory cells in the vitreous humor contribute to these symptoms.
- Eye Pain: Although uncommon, some patients may experience mild to moderate eye pain or discomfort.
- Photophobia: Retinal involvement and inflammation can cause sensitivity to light as well.
- Redness and Swelling: Inflammation of the eye can cause visible redness and swelling, though this is more common in uveitis than PIOL.
Differential Diagnosis
Because of its nonspecific symptoms, PIOL is frequently mistaken for other ocular conditions, particularly uveitis. Differential diagnosis includes:
- Uveitis: The most common initial misdiagnosis, uveitis is an inflammation of the uveal tract that causes symptoms like blurred vision, floaters, and photophobia.
- Retinal Detachment: Patients with PIOL may present with symptoms similar to retinal detachment, such as sudden vision loss and floaters.
- Endophthalmitis: This is an inflammation of the internal eye structures caused by infection. The presence of intraocular inflammation in the PIOL may resemble endophthalmitis.
- Age-Related Macular Degeneration (AMD): In older patients, the visual disturbances caused by PIOL may be mistaken for AMD, a common degenerative condition affecting the retina.
- Diabetic Retinopathy: Diabetic patients with visual symptoms may be misdiagnosed with diabetic retinopathy, a diabetes-related complication that affects the retinal blood vessels.
Complications
If left untreated, PIOL can cause serious complications, including:
- Vision Loss: The gradual infiltration of malignant cells and chronic inflammation can cause irreversible damage to retinal structures, resulting in significant vision loss or blindness.
- Central Nervous System Involvement: As a type of PCNSL, PIOL frequently spreads to the CNS. This can cause headaches, cognitive changes, and motor deficits.
- Secondary Glaucoma: Increased intraocular pressure due to inflammation or tumor infiltration can cause secondary glaucoma, which damages the optic nerve and causes vision loss.
- Cataract Formation: Chronic inflammation and the use of corticosteroids for treatment can speed up cataract formation, further impairing vision.
- Optic Neuropathy: Malignant cells can directly infiltrate the optic nerve, causing visual field defects and vision loss.
Prognosis
The prognosis for PIOL is dependent on several factors, including the extent of ocular and CNS involvement, the patient’s immune status, and treatment response. Historically, the prognosis has been poor, with median survival times ranging from months to years. However, advances in diagnostic techniques and treatment options have resulted in better outcomes for many patients.
Early diagnosis and treatment are critical for improving the prognosis of PIOL. Multidisciplinary management involving ophthalmologists, oncologists, and neurologists is frequently required to address the disease’s complexities and potential spread to the CNS.
Diagnostic methods
The diagnosis of primary intraocular lymphoma (PIOL) is difficult due to its nonspecific symptoms and similarities to other ocular inflammatory conditions. Accurate and timely diagnosis is critical for effective treatment and a good prognosis. Several diagnostic methods are used to confirm the presence of PIOL.
Clinical Examination
A comprehensive clinical examination by an ophthalmologist is the first step in diagnosing PIOL. This includes:
- Slit-Lamp Biomicroscopy: This examination provides detailed visualization of the eye’s anterior segment, which aids in the identification of cellular infiltration, vitreous haze, and other inflammatory signs.
- Fundus Examination: The fundus examination uses ophthalmoscopy to examine the eye’s posterior segment, which includes the retina and optic nerve. This aids in the detection of retinal infiltrates, hemorrhages, and other abnormalities indicative of PIOL.
Imaging Studies
Imaging studies play an important role in the diagnosis and evaluation of PIOL.
- Optical Coherence Tomography (OCT): OCT produces high-resolution cross-sectional images of the retina, enabling the detection of structural changes, retinal thickening, and subretinal fluid. It is especially useful for detecting retinal involvement in PIOLs.
- Fluorescein Angiography (FA) involves injecting a fluorescent dye into the bloodstream and photographing the retinal vasculature. This aids in detecting abnormal blood vessels, leakage, and other retinal changes associated with PIOL.
- Magnetic Resonance Imaging (MRI): An MRI of the brain and orbits is required to determine the extent of CNS involvement. It aids in detecting optic nerve infiltration, brain lesions, and other signs of PCNSL.
Cytological and histopathological analysis
Definitive diagnosis of PIOL frequently requires cytological and histopathological analysis of ocular fluids and tissues.
- Vitreous Biopsy: A vitrectomy procedure is used to collect a sample of vitreous humor. The presence of malignant lymphocytes in the sample is then determined. Identifying specific cell markers is possible using immunohistochemistry and flow cytometry.
- Chorioretinal Biopsy In some cases, a biopsy of the chorioretinal tissue may be required. This invasive procedure entails taking a small tissue sample for histopathological analysis to confirm the diagnosis.
Molecular and Genetic Testing
Advanced molecular and genetic testing techniques have increased the accuracy of PIOL diagnosis:
- Polymerase Chain Reaction (PCR): PCR can detect clonal immunoglobulin gene rearrangements in vitreous or retinal tissue samples. This aids in determining the monoclonality of the lymphoid cells.
- Next-Generation Sequencing (NGS): NGS reveals detailed genetic information about malignant cells, such as mutations and gene rearrangements. This data can help guide targeted therapies and improve diagnostic accuracy.
Cerebral Spinal Fluid (CSF) Analysis
Given the link between PIOL and PCNSL, CSF analysis is frequently used to assess CNS involvement:
- Lumbar Puncture: A lumbar puncture is used to extract cerebrospinal fluid for analysis. The CSF is examined for malignant cells, protein levels, and other signs of lymphomatous involvement. CSF analysis is especially useful when PIOL appears to have spread to the CNS.
Ancillary Testing
Additional tests may be performed to confirm the diagnosis and assess the patient’s overall health:
- Blood Tests: Blood tests, such as complete blood count (CBC), liver function tests, and HIV testing, can reveal important information about a patient’s overall health and immune status.
- Immunohistochemistry: This technique involves staining tissue samples with antibodies that bind to specific antigens found on malignant cells. It aids in determining the type of lymphoma and distinguishing it from other ocular disorders.
Diagnostic Challenges
Because of its rarity and clinical presentation, PIOL can be difficult to diagnose. Several factors contribute to these challenges.
- Nonspecific Symptoms: PIOL symptoms such as blurred vision, floaters, and eye pain are common to many other ocular conditions, resulting in frequent misdiagnosis.
- Slow Progression: PIOL typically progresses slowly, and symptoms can fluctuate, complicating the diagnosis.
- Invasive Procedures: Definitive diagnosis frequently necessitates invasive procedures, such as vitreous biopsy or chorioretinal biopsy, which are risky and may not always produce conclusive findings.
- Overlap with Other Conditions: PIOL can coexist with other ocular conditions, such as uveitis or age-related macular degeneration, making it difficult to determine whether the lymphoma is the primary cause of symptoms.
Despite these obstacles, advances in diagnostic techniques, particularly molecular and genetic testing, have greatly improved the ability to accurately diagnose PIOL. Early and accurate diagnosis is critical for effective treatment and a favorable prognosis.
The Importance of Multidisciplinary Approach
A multidisciplinary approach involving ophthalmologists, oncologists, neurologists, and pathologists is required for accurate diagnosis and treatment of PIOL. Collaboration among specialists ensures a thorough evaluation, accurate diagnosis, and appropriate treatment plan.
Primary Intraocular Lymphoma Management
Primary intraocular lymphoma (PIOL) requires a multidisciplinary approach that includes ophthalmologists, oncologists, and neurologists. The primary treatment goals are to control the ocular disease, avoid central nervous system (CNS) involvement, and improve overall survival. Management strategies are tailored to each patient based on the severity of the disease, general health status, and response to therapy. The main treatment options are systemic chemotherapy, local ocular treatments, and radiation therapy.
Systematic Chemotherapy
Systemic chemotherapy is frequently the foundation of PIOL treatment, particularly when there is concurrent CNS involvement or a high risk of CNS dissemination. Commonly used chemotherapeutic agents include:
- Methotrexate: High-dose methotrexate is commonly used because of its ability to cross the blood-brain barrier and reach therapeutic concentrations in the eye and CNS. It is frequently administered intravenously or intrathecally (directly into cerebrospinal fluid).
- Rituximab: This monoclonal antibody targets CD20-positive B-cells and is frequently used in conjunction with other chemotherapeutic agents. It can be given intravenously or as intravitreal injections (directly into the eye).
- Cytarabine: This antimetabolite is effective in treating CNS lymphomas and can be combined with methotrexate to increase efficacy.
- Temozolomide: Temozolomide is an oral alkylating agent used to treat CNS lymphomas and PIOL in combination with other chemotherapeutic agents.
Combination chemotherapy regimens, such as the MATRix regimen (methotrexate, cytarabine, thiotepa, and rituximab), are commonly used to improve outcomes.
Local Ocular Treatments
Local treatments seek to directly target the intraocular lymphoma while minimizing systemic toxicity. Treatments include:
- Intravitreal Injections: Direct injections of chemotherapeutic agents into the vitreous humor, such as methotrexate, rituximab, or cytarabine, result in high local drug concentrations while minimizing systemic exposure. This approach is especially beneficial for patients with isolated ocular disease or as an adjunct to systemic therapy.
- Ocular Radiation Therapy: External beam radiation therapy (EBRT) or plaque brachytherapy can be used to treat the affected eye. EBRT uses radiation from an outside source, whereas plaque brachytherapy involves placing a radioactive source near the tumor. These methods are effective at controlling local disease, but they come with the risk of radiation-induced side effects such as cataract formation and radiation retinopathy.
Radiation Therapy
Whole-brain radiation therapy (WBRT) is frequently considered for patients with CNS involvement or a high risk of CNS spread. WBRT can effectively control CNS lymphoma and prevent its spread. However, it is associated with significant neurotoxicity, particularly in older patients, and is typically reserved for situations where chemotherapy alone is insufficient.
Emerging Therapies
Advances in molecular and genetic understanding of PIOL have resulted in the development of targeted therapies and immunotherapy. This includes:
- Bruton’s Tyrosine Kinase (BTK) Inhibitors: Ibrutinib and other agents that target BTK, a critical enzyme in B-cell receptor signaling, have shown promise in the treatment of B-cell lymphomas, including PIOL.
- Chimeric Antigen Receptor (CAR) T-Cell Therapy: This novel approach entails modifying a patient’s T-cells to express receptors that specifically target lymphomas. CAR T-cell therapy has demonstrated efficacy in treating a variety of B-cell malignancies and is being studied for PIOL.
- Immune Checkpoint Inhibitors: Drugs that inhibit immune checkpoints, such as PD-1/PD-L1 inhibitors, can boost the body’s immune response to lymphomas. These agents are being investigated for potential use in PIOL management.
Supportive Care
Supportive care is critical for reducing treatment-related side effects and improving the patient’s quality of life. This includes:
- Corticosteroids: Steroids are commonly used to alleviate ocular inflammation and symptoms. They can be given topically, orally, or as periocular injections.
- Ocular Lubricants: Artificial tears and lubricating ointments can help relieve dryness and irritation caused by ocular inflammation and radiation therapy.
- Pain Management: Effective pain management, including the use of analgesics and anti-inflammatory medications, is critical for patient comfort.
Trusted Resources and Support
Books
- “Ocular Lymphoma” by Bertil Damato and Arun D. Singh: This comprehensive book provides detailed information on the diagnosis, treatment, and management of ocular lymphomas, including primary intraocular lymphoma.
- “Intraocular Lymphoma: Diagnosis and Treatment” by Justine R. Smith and H. Nida Sen: This book offers a thorough overview of intraocular lymphomas, focusing on clinical presentation, diagnostic methods, and therapeutic strategies.
Organizations
- American Academy of Ophthalmology (AAO): The AAO provides resources, guidelines, and continuing education for ophthalmologists and patients dealing with various eye conditions, including PIOL. AAO Website
- Lymphoma Research Foundation (LRF): The LRF offers comprehensive information on lymphoma research, patient support, and educational resources. They provide specific information on ocular and CNS lymphomas. LRF Website






