What is intermediate uveitis?
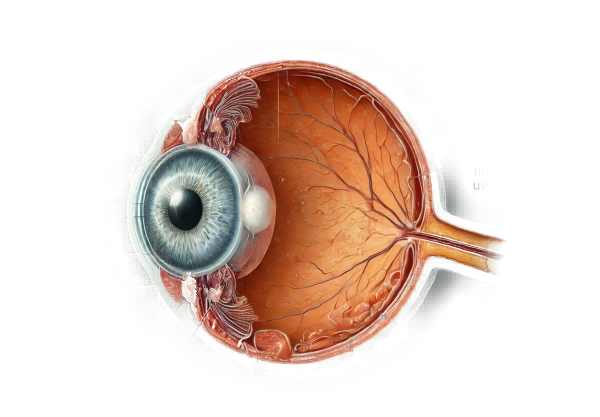
Intermediate uveitis is a type of uveitis that causes inflammation primarily in the vitreous humor and peripheral retina, both of which are located in the eye’s middle layer. Unlike anterior uveitis, which affects the front of the eye, intermediate uveitis affects the posterior segment, resulting in symptoms such as floaters and blurred vision. Although this condition can affect people of any age, it is most commonly diagnosed in young adults. The inflammation can be idiopathic or associated with systemic diseases such as multiple sclerosis or sarcoidosis, making early diagnosis and treatment critical to preventing vision loss.
In-Depth Look at Intermediate Uveitis
Intermediate uveitis, also known as pars planitis when no systemic disease is present, is a subset of uveitis that requires a thorough understanding because it has the potential to significantly impair visual function. This condition presents unique diagnostic and management challenges, owing to its involvement of the vitreous and peripheral retinas, as well as its often gradual onset.
Etiology and Pathogenesis
Intermediate uveitis can occur on its own or as a result of systemic diseases. The idiopathic form is commonly known as pars planitis, whereas secondary forms are associated with systemic conditions such as:
- Multiple Sclerosis (MS): A significant proportion of intermediate uveitis cases are linked to MS. The presence of uveitis can precede the diagnosis of MS, emphasizing the significance of neurological evaluation in affected patients.
- Sarcoidosis: This granulomatous disease can affect the eyes, resulting in intermediate uveitis. Early diagnosis of sarcoidosis is critical for effective management of both ocular and systemic manifestations.
- Infectious Agents: Although uncommon, infections like Lyme disease, syphilis, and tuberculosis can cause intermediate uveitis. Identifying the infectious cause is critical for effective treatment.
- Other Autoimmune Diseases: Inflammatory bowel disease (IBD), juvenile idiopathic arthritis (JIA), and Behçet’s disease can all be associated with intermediate uveitis, necessitating a thorough systemic evaluation.
Clinical Manifestations
Intermediate uveitis typically manifests with gradual onset of symptoms. The most common complaints are:
- Floaters: Patients frequently report seeing small, moving spots or strands in their vision due to inflammatory cells and debris in the vitreous humor.
- Blurred Vision: Caused by vitreous haze, cystoid macular edema (CME), or the presence of snowbanks and snowballs (inflammatory aggregates) in the peripheral retina.
- Mild Ocular Discomfort: Unlike anterior uveitis, intermediate uveitis rarely causes significant pain or redness, which can lead to a delay in diagnosis.
Pathophysiology
The inflammation in intermediate uveitis primarily affects the vitreous humor and the retina. The underlying mechanisms include:
- Immune Response: Activation of the immune system causes inflammatory cells such as lymphocytes, macrophages, and plasma cells to infiltrate the vitreous cavity.
- Cytokine Production: Pro-inflammatory cytokines like TNF-alpha and interleukins play an important role in maintaining inflammation. These cytokines are targets for new treatments aimed at reducing ocular inflammation.
- Structural Changes: Chronic inflammation can cause vitreous condensation, the formation of epiretinal membranes, and peripheral retinal neovascularization. These changes cause visual disturbances and complications.
Complications
If left untreated, intermediate uveitis can cause a number of sight-threatening complications:
- Cystoid Macular Edema (CME) is the leading cause of visual impairment in intermediate uveitis. It occurs when fluid accumulates in the macula, the central part of the retina responsible for sharp vision.
- Retinal Detachment: Tractional retinal detachment is caused by chronic inflammation, in which the retina is pulled away from its supporting tissue.
- Glaucoma: Chronic inflammation or corticosteroid therapy can cause an increase in intraocular pressure, which can damage the optic nerve.
- Cataracts: Prolonged use of corticosteroids, a common treatment for uveitis, can result in the development of cataracts, further impairing vision.
Epidemiology
The incidence and prevalence of intermediate uveitis vary around the world, owing to genetic and environmental factors. It accounts for 15–20% of all uveitis cases. The condition primarily affects young adults, with a slight female predominance. Geographic differences are evident, with certain regions reporting stronger associations with specific systemic diseases, such as MS in North America and Europe and sarcoidosis in African and Scandinavian populations.
Effects on Quality of Life
Intermediate uveitis can have a significant impact on a patient’s quality of life due to its chronic nature and risk of vision loss. Patients may have difficulty performing daily activities, become dependent on long-term medication, and experience psychological stress as a result of the risk of permanent vision impairment. Comprehensive care involving ophthalmologists, rheumatologists, and neurologists is essential for treating both the ocular and systemic aspects of the disease.
Diagnosing Techniques for Intermediate Uveitis
Intermediate uveitis diagnosis necessitates a comprehensive and systematic approach that includes clinical examination, advanced imaging techniques, and laboratory investigations.
Clinical Examination
A thorough clinical examination is the foundation for diagnosing intermediate uveitis. Key components are:
- Visual Acuity Test: This test evaluates the effect of uveitis on the patient’s vision, serving as a baseline for tracking disease progression and treatment efficacy.
- Slit-Lamp Biomicroscopy: This examination provides a detailed view of the anterior segment and vitreous humor, revealing inflammatory cells, vitreous haze, and keratic precipitates. It also helps to rule out anterior uveitis.
- Indirect Ophthalmoscopy: This examination is necessary for evaluating the peripheral retina and vitreous, and it can reveal snowbanks, snowballs, and peripheral retinal neovascularization, all of which are signs of intermediate uveitis.
Imaging Techniques
Advanced imaging techniques play an important role in diagnosing and monitoring intermediate uveitis.
- Optical Coherence Tomography (OCT): OCT generates high-resolution cross-sectional images of the retina, which can detect cystoid macular edema (CME), epiretinal membranes, and other structural changes. It is invaluable for assessing treatment response and early detection of complications.
- Fluorescein Angiography (FA) is a technique for visualizing the retinal vasculature and detecting capillary leakage, retinal vasculitis, and neovascularization. This imaging technique assists in distinguishing intermediate uveitis from other retinal vascular diseases.
- Ultrasound Biomicroscopy (UBM) is especially useful when there is significant vitreous haze or media opacities that prevent detailed fundus examination. It captures detailed images of the ciliary body and peripheral retinas.
Lab Investigations
Laboratory tests are important for identifying underlying systemic diseases and infectious causes.
- Blood Tests: A complete blood count (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) levels indicate systemic inflammation. Clinical suspicion guides the use of specific serological tests, such as angiotensin-converting enzyme (ACE) levels for sarcoidosis and Lyme serology.
- Imaging Studies: Systemic imaging tests, such as chest X-rays or CT scans, can aid in the diagnosis of granulomatous diseases such as Sarcoidosis. When multiple sclerosis is suspected, an MRI of the brain and spine is recommended, which will reveal demyelinating lesions characteristic of MS.
- Infectious Disease Testing: Testing for infectious agents such as tuberculosis (QuantiFERON-TB Gold), syphilis (RPR, FTA-ABS), and other relevant pathogens is critical when an infectious etiology is suspected.
Intermediate Uveitis Treatment
Treating intermediate uveitis requires a multifaceted approach that includes reducing inflammation, managing complications, and addressing any underlying systemic diseases that may be present. The primary goals are to reduce inflammation, prevent tissue damage, and maintain vision.
Corticosteroids
Corticosteroids are the primary treatment for intermediate uveitis due to their potent anti-inflammatory properties. They can be administered in a variety of ways:
- Topical steroids: Primarily used to treat anterior segment inflammation, but less effective for intermediate uveitis.
- Periocular Steroid Injections: Performed around the eye to deliver high doses of steroids directly to the site of inflammation.
- Systemic Steroids: Oral corticosteroids, such as prednisone, are used in more severe cases but must be closely monitored due to potential systemic side effects.
- Intravitreal Steroid Implants: Long-acting implants, such as the fluocinolone acetonide implant (Retisert) and the dexamethasone implant (Ozurdex), provide continuous drug delivery and are especially useful in chronic or refractory cases.
Immunosuppressive Agents
Immunosuppressive agents are frequently prescribed for patients who do not respond well to corticosteroids or require long-term therapy.
- Methotrexate is a common first-line immunosuppressant for uveitis.
- Azathioprine is another commonly used immunosuppressant medication.
- Mycophenolate Mofetil: An effective anti-inflammatory with a low risk of side effects.
- Cyclophosphamide is reserved for severe, refractory cases due to its potent immunosuppressive properties.
Biological Agents
Biologic therapies have revolutionized the treatment of refractory uveitis by targeting specific immune pathways:
- TNF-alpha Inhibitors: Infliximab and adalimumab are two commonly used biologics for intermediate uveitis, especially in patients with underlying systemic inflammatory diseases.
- Interleukin Inhibitors: Tocilizumab, which targets the IL-6 pathway, shows promise in treating refractory cases.
Other Therapies
- Antimicrobial Therapy: Once an infectious cause has been identified, proper antimicrobial treatment is required. This includes antibiotics for bacterial infections, antivirals for viral infections, and antiparasitic medications for parasitic infections.
- Anti-VEGF Therapy: To treat complications such as neovascularization, anti-VEGF agents such as bevacizumab can be injected into the vitreous.
Emerging Therapies
Research is ongoing into new treatments for intermediate uveitis, including:
- Gene Therapy: Experimental approaches aim to deliver therapeutic genes directly into ocular tissues in order to modulate the immune response.
- JAK Inhibitors: These small molecules inhibit Janus kinase pathways, which are involved in inflammatory processes, providing a new treatment option for refractory uveitis.
- Stem Cell Therapy: Research into using stem cells to regenerate damaged ocular tissues and restore vision.
Healthcare providers can effectively control inflammation, prevent complications, and improve outcomes for patients with intermediate uveitis by tailoring treatment to their specific needs and utilizing the most recent advances in uveitis management.
Effective Ways to Improve and Prevent Intermediate Uveitis
- Regular Eye Examinations: Routine eye exams can detect early signs of uveitis and other ocular conditions, allowing for timely treatment.
- Prompt Treatment of Systemic Diseases: Manage underlying systemic conditions such as multiple sclerosis, sarcoidosis, and inflammatory bowel disease to avoid associated uveitis.
- Vaccinations: Keep vaccinations up to date to reduce the risk of infections that can cause uveitis, such as influenza and herpes zoster vaccines.
- Good Hygiene Practices: Keep proper hygiene, including regular hand washing, to avoid infectious causes of uveitis.
- Avoidance of Eye Trauma: Wear protective eyewear during risky activities to protect the eyes from injuries that may cause inflammation.
- Healthy Lifestyle: A well-balanced diet, regular exercise, and quitting smoking can improve overall health and lower the risk of inflammatory diseases.
- Stress Management: Because chronic stress can exacerbate autoimmune conditions, practices like mindfulness, meditation, and getting enough sleep are beneficial.
- Safe Contact Lens Use: To avoid infections, practice proper contact lens hygiene, such as cleaning them regularly and not wearing them overnight.
- Awareness of Symptoms: Inform patients about the symptoms of uveitis (floaters, blurred vision, and eye discomfort) so that they can seek immediate medical attention if they occur.
- Regular Monitoring: For patients with known risk factors or a history of uveitis, regular monitoring and early treatment can help prevent recurrence and complications.
Individuals who follow these preventive measures and take a proactive approach to eye health can significantly reduce their risk of developing intermediate uveitis and its complications.
Trusted Resources
Books
- “Uveitis: Fundamentals and Clinical Practice” by Robert B. Nussenblatt and Scott M. Whitcup
- “Ocular Inflammatory Disease” by Jack J. Kanski and Carlos Pavesio
- “Intraocular Inflammation: Uveitis and Ocular Immunology” by Manfred Zierhut, Hans-Georg Rammensee, and Joachim W. Meyer
Online Resources
- American Academy of Ophthalmology (AAO): www.aao.org
- National Eye Institute (NEI): www.nei.nih.gov
- Uveitis Information Group: www.uveitis.net
- Ocular Immunology and Uveitis Foundation: www.uveitis.org
- Mayo Clinic: www.mayoclinic.org






