Keratoconus is a progressive eye condition characterized by the thinning and bulging of the cornea, causing it to develop a cone-like shape instead of maintaining its normal dome. This abnormal curvature leads to irregular astigmatism and significant vision impairment that often cannot be adequately corrected with conventional eyeglasses. While mild cases can sometimes be managed with custom contact lenses, more advanced stages may demand surgical intervention to curb further corneal distortion and preserve remaining vision quality.
In recent years, Intracorneal Ring Segments (ICRS) have become a key option for individuals seeking improved corneal stability and better visual acuity. By inserting small, semi-circular rings into the peripheral cornea, ophthalmologists can modify its shape and help distribute refractive forces more uniformly. This approach has gained international recognition for its ability to reinforce thinning corneas and restore a degree of normality in cases of mild to moderate keratoconus, giving patients renewed hope for stronger, more stable eyesight.
Understanding How Intracorneal Ring Segments Improve Vision
Intracorneal Ring Segments, often crafted from specialized biocompatible materials such as PMMA (polymethyl methacrylate), are meticulously placed into the mid-peripheral cornea to reshape its curvature and reduce the cone’s steepness. Keratoconus stems from a biomechanical weakness in the corneal tissue, leading to progressive thinning and bulging, particularly around the central or paracentral region. With the introduction of ICRS, the cornea gains a form of structural support, mitigating the most pronounced distortions.
A Closer Look at the Keratoconus Progression
Keratoconus can begin during adolescence or early adulthood and often advances slowly over time. Initial signs include minor blurring of vision and increased sensitivity to light, which can worsen as the cornea becomes thinner and more conical. The resulting irregular astigmatism remains challenging to correct with standard eyeglasses; many patients turn to specially fitted contact lenses or hybrid lens designs. However, in moderate stages, even advanced lens technology may fail to offer stable or comfortable vision, especially if the corneal cone becomes highly pronounced.
Genetics, eye rubbing, and other factors such as oxidative stress have been linked to the development and progression of keratoconus. Collagen cross-linking (CXL) is another standard therapy aimed at stopping or slowing the disease, although it does not always adequately rectify corneal shape anomalies if the cone is already well-developed. This is where ICRS can fill the gap: by physically altering the cornea’s contour, it often decreases the steepness at the apex of the cone and reduces the degree of irregular astigmatism.
Reshaping the Cornea: The Role of Ring Segments
Intracorneal Ring Segments are essentially thin, crescent-shaped rings that come in various thicknesses, lengths, and arcs. Placed in channels at about 70-80% corneal depth, these rings help flatten and regularize the cornea. The principle rests on biomechanical redistribution of corneal tissue: as the ring exerts an outward, peripheral “push,” the most elevated region of the cornea tends to become less steep.
- Peripheral Support: Insertion of the segments into the mid-peripheral cornea provides a structured support system. This mild “brace” effect can alleviate some of the distortive forces pulling the cornea into a cone shape.
- Adjustability: Ophthalmic surgeons can choose from different ring sizes, thicknesses, and configurations, tailoring them to a patient’s unique corneal topography and keratoconus stage. Some systems even allow removal or exchange of the segments if the patient’s condition changes over time.
- Improved Optical Quality: Flattening the most protruding area of the cornea can reduce irregular astigmatism, which may allow some patients to return to simpler vision correction tools like eyeglasses or softer contact lenses—significantly enhancing daily comfort and convenience.
Combining ICRS with Other Therapies
In addition to reshaping the cornea, Intracorneal Ring Segments can be combined with other treatments to optimize patient outcomes. Collagen cross-linking (CXL), for example, strengthens the molecular bonds in the cornea, potentially slowing or stopping keratoconus progression. For patients with mild or moderate keratoconus, surgeons may perform cross-linking before or after ICRS insertion, depending on which approach best suits the individual’s particular condition and corneal thickness measurements.
Furthermore, some patients benefit from topography-guided photorefractive keratectomy (PRK) or laser treatments. However, these are more frequently considered after cross-linking has stabilized the cornea. When effectively sequenced, combining CXL with ICRS often produces more stable and predictable outcomes than either therapy alone. This comprehensive approach seeks to not only halt disease progression but also restore a smoother corneal profile for improved functional vision.
Ideal Candidates and Limitations
Although Intracorneal Ring Segments can provide notable benefits, they may not be suitable for every keratoconus patient. The ideal candidates often have:
- Mild to Moderate Keratoconus: Severe corneal thinning or scarring might limit the cornea’s ability to accommodate the ring channels.
- Stable or Slowly Progressing Disease: Rapidly advancing keratoconus might require a more immediate intervention such as urgent collagen cross-linking.
- Adequate Corneal Thickness: Because ring segments are placed at a specific corneal depth, extremely thin corneas in advanced disease stages may not support the implants without added risks.
Despite these benefits, ICRS does not cure keratoconus or eliminate the underlying tissue weakness. In some cases, it simply delays the need for corneal transplantation by improving the optical characteristics of the cornea. If keratoconus continues to advance even with ring segments in place, other surgeries such as deep anterior lamellar keratoplasty (DALK) or a full-thickness corneal transplant may eventually be required.
Guidelines and Procedures for Implementing ICRS
Intracorneal Ring Segment implantation follows a precise protocol that starts with thorough patient evaluation and progresses through channel creation, segment insertion, and careful follow-up care. By adhering to strict guidelines at every step, eye surgeons aim to optimize both the immediate correction of corneal shape and the long-term health of the eye.
Preoperative Evaluations and Diagnostic Measures
Any surgical plan for keratoconus depends heavily on detailed corneal assessments, which help determine suitability for ICRS and guide selection of the segment design. Key diagnostic tools and evaluations typically include:
- Corneal Topography: This imaging test maps the curvature of the cornea, highlighting areas of steepening or thinning. Topography is central to deciding the ring thickness, arc length, and placement for the greatest improvement.
- Pachymetry: This measures the corneal thickness at various points. Adequate thickness is critical to ensure a safe channel depth for ring insertion.
- Visual Acuity and Refraction Tests: A baseline measurement of the patient’s current refractive status allows comparisons postoperatively to gauge how effectively the therapy corrects the astigmatism.
- Eye Health Assessment: Beyond keratoconus, surgeons also check for other ocular conditions such as cataracts, glaucoma, or corneal scarring. These factors can influence surgical choices, outcomes, and healing timelines.
During the preoperative consultation, doctors review a patient’s medical history, especially noting any collagen or connective tissue disorders that might exacerbate corneal instability. If the patient’s keratoconus is rapidly progressing, the surgical team might incorporate or prioritize collagen cross-linking to halt further deterioration before placing the segments.
Creating the Channels for Ring Placement
The surgical process involves forming channels in the cornea where the Intracorneal Ring Segments will reside. Surgeons typically use one of two methods:
- Mechanical Dissection: In earlier systems, surgeons utilized blades to craft channels at a predetermined depth. Though effective, this method can be more prone to variations in depth and diameter.
- Femtosecond Laser: Most modern techniques use ultrafast lasers to create highly precise tunnels with minimal disturbance to surrounding tissue. Laser-guided incisions can be customized to exact dimensions, offering better predictability and safety.
During channel creation, the surgeon must ensure a sufficient corneal depth to accommodate the segments without risking perforation. The location of the incisions is carefully planned according to topography, aiming to flatten the steepest corneal areas where the cone is most pronounced. Successful channel creation sets the stage for an accurate and stable ring segment insertion.
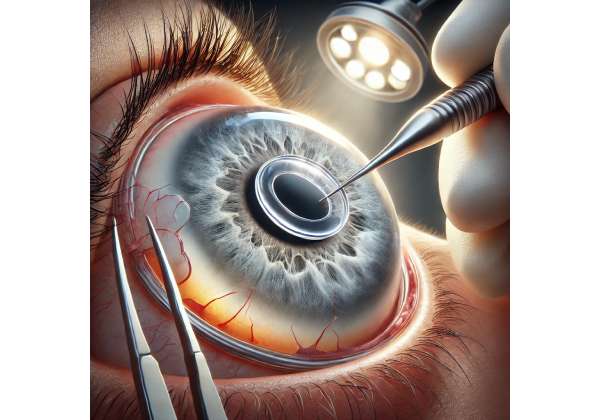
Placing the Intracorneal Ring Segments
Once channels are ready, the surgeon gently inserts the preselected segment or segments (typically two arcs in a symmetrical or asymmetrical configuration) into the corneal stroma. Each ring is positioned so that it applies a slight outward force on the local tissue. Although the procedure may differ slightly depending on the brand of the ring or the surgical center’s protocols, common points include:
- Sterile Environment and Anesthesia: Most surgeries are performed under sterile conditions, with local anesthesia or anesthetic eye drops. Patients remain awake but comfortable throughout.
- Precision and Alignment: The rings must be oriented precisely along the desired axis. Some systems offer additional markers or radial incisions to enhance alignment.
- Minimal Sutures: Depending on the technique, a small stitch or special adhesive may be required to close the channel incision. Alternatively, some channels are self-sealing.
After ring insertion, surgeons often apply antibiotic or anti-inflammatory eye drops to reduce the risk of infection and enhance healing. Patients usually rest briefly before returning home on the same day, provided there are no immediate complications.
Postoperative Care and Follow-Up
Recovery from ICRS implantation can be relatively quick, but patients need consistent monitoring to ensure proper healing and to gauge the therapy’s impact on visual acuity. Typical postoperative guidelines may include:
- Protective Eyewear and Activity Restrictions: Initially, patients should avoid rubbing their eyes, heavy lifting, or high-impact sports that could disrupt the newly placed segments.
- Medication Regimens: Prescription eye drops, such as antibiotic and corticosteroid formulations, can help curb inflammation and ward off infection.
- Scheduled Check-Ups: Follow-up visits may occur one day after surgery, one week later, and then monthly or quarterly for up to a year. During these appointments, doctors evaluate the placement of the rings, measure corneal topography, and review improvements in visual acuity.
- Possible Segment Adjustments: In some cases, if outcomes are suboptimal, the surgeon might choose to remove or exchange one or both segments. The system’s modular nature allows for customization as the patient’s condition evolves.
Postoperative improvements often begin within days or weeks, though it can take several months for the cornea to completely stabilize. Regular updates to refraction and contact lens measurements ensure that patients optimize their overall visual correction strategy. For many individuals, the final prescription for glasses or specialized lenses will not be finalized until the cornea has fully adapted to the presence of ICRS.
Up-to-Date Clinical Findings and Investigations
As Intracorneal Ring Segments gain traction worldwide, a growing body of research seeks to refine surgical techniques, enhance patient outcomes, and broaden our understanding of keratoconus management. Investigations range from controlled trials comparing different ring systems to long-term studies tracking corneal integrity and quality of life among implant recipients.
Comparative Studies of Different Ring Systems
Several manufacturers produce distinct ICRS designs, including Intacs®, Ferrara Rings, and Keraring®, each with various thicknesses and arc lengths. Comparative studies often assess metrics such as:
- Improvement in Best-Corrected Visual Acuity (BCVA): In many trials, patients receive a ring in one eye and a different brand or thickness in the other. Researchers then track changes in visual acuity over periods ranging from six months to two years.
- Reduction in Corneal Steepness: Topography-based indices, like the maximum keratometry (Kmax) value, help quantify how effectively each ring configuration flattens the cone.
- Patient Comfort and Satisfaction: Beyond visual outcomes, researchers evaluate how comfortable the implants are under daily conditions. Reduced glare, halos, and contact lens tolerance are frequently monitored.
Some trials indicate that Ferrara Rings may show a stronger flattening effect for cones located in certain corneal quadrants, while others find that Intacs® yield more uniform improvements in a broader range of keratoconus types. The consensus, however, remains that matching the ring design to the individual’s corneal shape and severity leads to the most consistent results.
Long-Term Stability and Preservation of Corneal Tissue
One of the primary goals in keratoconus therapy is to prolong the functioning life of the cornea and postpone or avoid the need for a corneal transplant. Longitudinal studies have followed patients for over five years post-ICRS insertion, with many maintaining stable vision and corneal shape.
- Collagen Cross-Linking (CXL) Synergy: Preliminary evidence suggests that combining cross-linking with ring segment implantation yields superior long-term outcomes compared to using either method alone. Cross-linking halts the progression, while ICRS refines corneal shape.
- Minimally Invasive Nature: Because ICRS implantation spares most corneal tissue, patients who later require a corneal transplant can still undergo the procedure without significant scarring or complications from the previous surgery.
Patient-Reported Quality of Life Outcomes
Beyond clinical measurements, patient satisfaction surveys provide insight into the daily impact of ICRS. Many individuals report:
- Enhanced Self-Reliance: Reduced dependence on rigid or specially fitted contact lenses can be liberating, particularly for patients who struggled with comfort and dryness.
- Improved Night Vision: Lower levels of distortion from the cone often translate to fewer glares and halos around lights at night.
- Greater Freedom in Activities: Some patients are better able to engage in sports or outdoor hobbies with minimal corrective devices, alleviating constant worry about lens dislodgement or corneal abrasions.
These positive reports underscore the importance of broadening access to ICRS as an alternative to more invasive surgeries, especially for those caught in the early to moderate stages of keratoconus progression. Nonetheless, experts acknowledge that while many patients benefit, success rates vary widely based on individual corneal anatomy and the stage of disease.
Emerging Technologies and Future Directions
As surgical lasers and biomaterials evolve, so do the strategies for corneal reinforcement. Novel developments include:
- New Ring Shapes and Composite Materials: Innovations in geometry, such as trapezoid or wedge-shaped segments, may yield even better control over corneal flattening. Bioinspired polymer blends also promise enhanced compatibility and minimized corneal inflammation.
- Combination with Customized Laser Ablation: In advanced research centers, there is ongoing exploration of topography-guided surface ablation procedures after ring placement to refine the cornea further. This dual approach may significantly enhance final visual acuity.
- AI-Driven Patient Selection: Big data analytics and artificial intelligence are being used to predict which keratoconus patients are most likely to respond well to ICRS, thereby reducing the trial-and-error aspect of ring selection and placement.
By systematically collecting long-term data and embracing innovations, eye surgeons and researchers are continually refining their ability to stabilize keratoconus while preserving as much of the patient’s natural cornea as possible. This push toward evidence-based refinements means that future generations of ICRS could become an even more standard procedure, potentially diminishing the need for corneal transplant in a significant portion of keratoconus cases.
Assessing Reliability, Risk Factors, and Overall Efficacy
For any keratoconus intervention, it is crucial to weigh the likelihood of stable, improved vision against potential complications. Intracorneal Ring Segments have a relatively strong safety record when performed by experienced ophthalmic surgeons. Yet, as with all procedures, success depends on patient selection, disease stage, precise surgical technique, and vigilant follow-up care.
Evaluating the Success of the Procedure
Clinical success metrics are usually centered around improvements in visual acuity, reduction in keratometric values (curvature measurements), and enhanced corneal regularity. Though specific results differ, many studies report:
- Moderate to Significant Vision Gains: A considerable percentage of patients experience at least one to two lines of improvement on the Snellen visual acuity chart. This gain might be even more pronounced with specialized contact lenses, which often fit better following the procedure.
- Stability Over Time: When combined with collagen cross-linking, ring segment placement has demonstrated durable results, offering a stable corneal shape for several years.
- Improved Tolerance for Other Corrections: Even if the cone is not fully flattened, better corneal symmetry may allow for softer lens options or simpler rigid gas-permeable designs, leading to higher comfort and daily convenience.
Recognizing Potential Complications
Although complications are relatively rare, patients should be informed about possible adverse events:
- Infection and Inflammation: As with any intraocular or corneal surgery, there is a risk of microbial contamination or excessive inflammatory response. Strict sterility protocols and antibiotics help mitigate these hazards.
- Ring Extrusion or Erosion: In cases where the channels are too shallow or the cornea is exceedingly thin, the segments might shift or extrude over time. This can lead to discomfort, scarring, or corneal abrasions, necessitating ring adjustment or removal.
- Over- or Under-Correction: If the segments are not aligned perfectly, or if the patient’s corneal shape changes postoperatively, the final curvature may not yield the anticipated visual improvement. A subsequent procedure may be required to adjust the ring thickness or position.
- Halos and Glare: Some patients, especially those with rings placed centrally or close to the visual axis, could experience halos or glare under low-light conditions. This phenomenon usually diminishes as the eye adapts.
Despite these risks, serious sight-threatening complications remain infrequent when performed by skilled surgeons. The risk profile of ICRS is significantly lower than that of full-thickness corneal transplants, which can be a critical factor for patients weighing different surgical options.
Factors Influencing Treatment Outcomes
The variability in individual keratoconus presentations means that no single formula guarantees a successful outcome. Instead, multiple elements affect how well a patient responds to ICRS:
- Cone Location: Cones can form in central, paracentral, or peripheral regions of the cornea, necessitating varying ring types and placements.
- Disease Severity: More advanced keratoconus may have thinner areas not amenable to ring placement, or it might require combining ICRS with corneal cross-linking to halt progression.
- Healing Capacity: Underlying health conditions, ocular surface disease, or autoimmune disorders can impact tissue healing and corneal remodeling post-surgery.
- Surgical Precision: Use of femtosecond lasers to create channels, careful measurement of segment thickness, and accurate alignment contribute to high rates of success.
By thoroughly evaluating these factors, surgeons can more effectively tailor the procedure to individual patient profiles. For instance, those with inferiorly decentered cones may benefit from a single segment placed in the steep area, whereas symmetrical cones might warrant two segments for balanced flattening. A methodical approach translates to higher patient satisfaction and fewer corrective procedures down the line.
Integrating ICRS into a Broader Treatment Strategy
Intracorneal Ring Segments are often just one component of a multifaceted keratoconus management plan. Patients might also require:
- Pre- or Postoperative Collagen Cross-Linking: To secure corneal stability and hinder ongoing deformation.
- Customized Contact Lenses: Even after a successful implantation, many individuals rely on specialty lenses for optimal visual clarity.
- Lifestyle Adjustments: Reducing chronic eye rubbing, managing allergies, and using lubricating drops can reduce mechanical stress on the cornea.
- Regular Monitoring: Yearly check-ups to track corneal topography and overall ocular health ensure any sign of disease progression is addressed promptly.
Ultimately, ICRS represents a powerful option for patients in need of corneal reshaping but who are not yet candidates for transplant. Its success highlights the importance of tailored interventions: by combining advanced diagnostic technologies, skilled surgical approaches, and a proactive follow-up plan, clinicians can significantly improve outcomes for those with keratoconus.
Cost Factors and Financial Planning
Costs for Intracorneal Ring Segment implantation can vary widely. In many clinics, total expenses range from \$3,000 to \$6,000 per eye, though premium services or additional therapies like collagen cross-linking might increase the overall price. Some providers offer financing plans or work with insurance providers if coverage applies. Patients seeking lower costs sometimes explore medical tourism, comparing rates across international centers. Always prioritize surgeon expertise and quality of care when making decisions, as both are essential to a safe and successful outcome.
Disclaimer:
This article is for informational purposes only and is not intended as a substitute for medical advice. Always consult a qualified eye care professional for a thorough evaluation of your condition and individualized treatment recommendations.
We encourage you to share this article with anyone who might benefit from learning about Intracorneal Ring Segments for keratoconus. Use our convenient Facebook or X (formerly Twitter) share buttons, or any social media platform you prefer. By spreading the word, you can help others find the solutions they need for more stable and reliable vision.