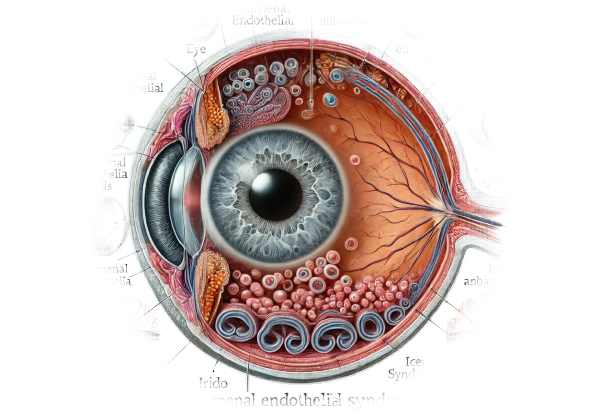
What is Irido-Corneal Endothelial Syndrome?
Irido Corneal Endothelial Syndrome (ICE Syndrome) is a rare ocular disorder that causes abnormal proliferation and migration of endothelial cells from the cornea to the iris. This syndrome causes a variety of clinical manifestations, including corneal edema, iris atrophy, and secondary glaucoma. ICE Syndrome usually affects just one eye and is more common in middle-aged women. The exact cause of the condition is unknown, but it is thought to be related to viral infections or genetics. Early detection and careful management are critical for preventing vision loss and managing related complications.
Detailed Investigation of Irido Corneal Endothelial Syndrome
Irido Corneal Endothelial Syndrome (ICE Syndrome) is a unique ocular disorder characterized by a variety of clinical signs caused by abnormal corneal endothelial cell behavior. Understanding ICE Syndrome necessitates a thorough examination of its pathophysiology, clinical manifestations, types, complications, and effects on patients.
Pathophysiology
The primary abnormality in ICE Syndrome is endothelial cell proliferation and migration from the cornea to the iris and anterior chamber angle. These endothelial cells behave like epithelial cells, forming membrane-like structures that obstruct normal aqueous humor outflow, resulting in elevated intraocular pressure (IOP) and secondary glaucoma. The precise cause of this cellular transformation is unclear, but several theories have been proposed:
- Viral Hypothesis: Some studies link herpes simplex virus (HSV) infection with ICE Syndrome. Viral particles may cause endothelial cell changes, resulting in the syndrome’s defining characteristics.
- Genetic Predisposition: While no clear genetic pattern exists, some familial cases indicate a genetic component. Additional research is required to identify specific genetic markers.
Clinical Manifestations
ICE Syndrome encompasses a wide range of symptoms and signs that can differ significantly between patients. The syndrome is broadly divided into three clinical variants, each with distinct features:
- Chandler Syndrome: The most common variant, Chandler Syndrome is defined by mild corneal edema and a “beaten metal” appearance of the corneal endothelium. Patients with corneal changes usually have blurred vision and halos around lights.
- Essential Iris Atrophy: This variant has severe iris atrophy and holes or tears in the iris stroma. Patients may have corectopia (pupil displacement) or polycoria (multiple pupils). Endothelial membranes frequently close the anterior chamber angle, resulting in glaucoma.
- Cogan-Reese Syndrome: Also known as iris nevus syndrome, this variant is characterized by nodular or diffuse pigmented lesions on the iris surface. Endothelial cell proliferation causes these nodules, which can result in significant anterior chamber angle obstruction and glaucoma.
Complications
Complications of ICE Syndrome are primarily related to corneal and intraocular pressure changes.
- Corneal Edema: Prolonged corneal edema can cause chronic discomfort, photophobia, and severe visual impairment. In severe cases, corneal transplantation may be necessary.
- Secondary Glaucoma: The most serious complication is secondary glaucoma, which occurs when abnormal endothelial cells block the trabecular meshwork. Elevated IOP can cause optic nerve damage and irreversible vision loss if not treated promptly.
- Iris Changes: Iris atrophy and the formation of ectopic pupil locations can cause aesthetic issues and additional visual disturbances.
Diagnostics
To distinguish ICE Syndrome from other similar ocular conditions, a clinical exam and diagnostic tests are required. The key diagnostic criteria are:
- Slit-Lamp Examination: Identifies typical corneal endothelial changes, such as a beaten metal appearance, and determines the extent of iris atrophy and abnormal pupil positions.
- Gonioscopy: Measures the anterior chamber angle to detect membrane formation or angle closure.
- Specular Microscopy: Produces detailed images of the corneal endothelium, highlighting abnormal cell morphology.
- Ultrasound Biomicroscopy: Visualizes structural changes in the anterior segment, including the iris and angle.
Differential Diagnosis
ICE Syndrome is difficult to distinguish from other conditions that cause similar symptoms, such as:
- Fuchs Endothelial Dystrophy: Unlike ICE Syndrome, this condition affects both eyes and does not usually cause iris changes.
- Anterior Uveitis: Uveitis can cause corneal edema and increased IOP, but it is more commonly associated with inflammation and pain than with ICE Syndrome.
- Primary Angle-Closure Glaucoma: This condition has elevated IOP and angle closure but lacks the endothelial and iris changes found in ICE Syndrome.
Epidemiology
ICE Syndrome is extremely rare, with an estimated prevalence of 1 in 100,000 individuals. It primarily affects women in their third to fifth decades of life and is usually unilateral. The rarity of the syndrome and its variable presentation can result in delayed diagnosis, emphasizing the importance of healthcare provider awareness.
Effects on Quality of Life
ICE Syndrome’s progressive nature, as well as its potential complications, can have a significant impact on patients’ quality of life. Chronic corneal edema and glaucoma can cause persistent visual disturbances and discomfort, limiting daily activities and overall well-being. Furthermore, aesthetic changes caused by iris abnormalities can lead to psychological distress.
Diagnosing Techniques for ICE Syndrome
A detailed clinical evaluation and the use of specialized diagnostic tools to confirm the presence of characteristic endothelial and iris changes are required to diagnose Irido Corneal Endothelial Syndrome (ICE Syndrome).
Clinical Evaluation
A thorough clinical evaluation is the foundation for diagnosing ICE Syndrome. Key components are:
- Patient History: Provide a detailed patient history to identify symptoms such as visual disturbances, eye discomfort, and any history of ocular or systemic conditions.
- Slit-Lamp Examination: This is required for detecting corneal endothelial changes, such as the “beaten metal” appearance, as well as determining the extent of iris atrophy, corectopia, and other iris abnormalities.
Imaging Techniques
Advanced imaging techniques offer detailed views of the corneal endothelium, iris, and anterior chamber angle, which aid in the diagnosis of ICE Syndrome.
- Specular Microscopy: This technique produces high-resolution images of the corneal endothelium, allowing for the analysis of cell morphology and density. It can reveal the abnormal endothelial cell patterns associated with ICE Syndrome.
- Gonioscopy: Gonioscopy examines the anterior chamber angle and aids in the detection of endothelial membranes, which can cause angle closure and secondary glaucoma.
- Ultrasound Biomicroscopy (UBM): UBM generates detailed cross-sectional images of the anterior segment structures, such as the cornea, iris, and angle. It is especially useful for observing structural changes and determining the extent of membrane formation.
Lab Tests
Although laboratory tests are not required in most cases, they can help rule out other conditions and support the diagnosis.
- Polymerase Chain Reaction (PCR): PCR testing of aqueous humor samples can detect viral DNA, lending support to the viral hypothesis in herpes simplex virus cases.
- Fluorescein Angiography: This imaging technique can detect abnormal vascularization in the iris, which may be present in some types of ICE Syndrome.
Differential Diagnosis
Distinguishing ICE Syndrome from other ocular conditions with similar symptoms is critical for accurate diagnosis and treatment. Differential diagnosis includes:
- Fuchs Endothelial Dystrophy: This condition primarily affects the corneal endothelium, but it usually affects both eyes and lacks the iris changes found in ICE Syndrome.
- Anterior Uveitis: Uveitis symptoms include inflammation, pain, and photophobia, which are less common in ICE Syndrome. Uveitis is also characterized by increased anterior chamber inflammation and keratic precipitates.
- Primary Angle-Closure Glaucoma: Unlike ICE Syndrome, primary angle-closure glaucoma does not cause distinctive endothelial changes or iris abnormalities. Peripheral anterior synechiae and elevated intraocular pressure are more common.
Treatment Options for ICE Syndrome
To avoid glaucoma complications, treating Irido Corneal Endothelial Syndrome (ICE Syndrome) requires a multifaceted approach that includes addressing underlying endothelial abnormalities, managing corneal edema, and controlling intraocular pressure. Treatment plans are tailored to the individual clinical manifestations and severity of each case.
Medical Management
- Topical Medications: Topical treatments are frequently the first line of treatment for corneal edema and secondary glaucoma.
- Hypertonic Saline Drops: These drops reduce corneal edema by removing excess fluid from the cornea.
- Antiglaucoma Medications: Eye drops containing beta-blockers (e.g., timolol), prostaglandin analogs (e.g., latanoprost), alpha agonists (e.g., brimonidine), and carbonic anhydrase inhibitors (e.g., dorzolamide) are used to reduce intraocular pressure.
- Oral Medications: When topical treatments are insufficient, oral carbonic anhydrase inhibitors (e.g., acetazolamide) can be used to lower intraocular pressure even further.
Surgical Interventions
- Laser Therapy: Selective laser trabeculoplasty (SLT) or argon laser trabeculoplasty (ALT) can be used to improve aqueous outflow in patients with ICE Syndrome-related glaucoma.
- Filtering Surgery: Patients with refractory glaucoma should consider trabeculectomy or tube shunt surgery. These procedures provide an alternative pathway for aqueous humor drainage, lowering intraocular pressure.
- Endothelial Keratoplasty: For patients with severe corneal edema and endothelial decompensation, endothelial keratoplasty (e.g., Descemet’s stripping automated endothelial keratoplasty, DSAEK, or Descemet membrane endothelial keratoplasty, DMEK) is an effective surgical option. This procedure replaces the diseased endothelium with healthy donor tissue, resulting in improved cornea clarity and vision.
Innovative and Emerging Therapies
- Minimally Invasive Glaucoma Surgery (MIGS): MIGS procedures, such as the iStent or Trabectome, provide less invasive options for managing glaucoma, with shorter recovery times and fewer complications than traditional surgeries.
- Corneal Transplantation: Penetrating keratoplasty (full-thickness corneal transplant) is reserved for severe cases of corneal decompensation that do not respond to endothelial keratoplasty. It improves vision significantly, but it also increases the risk of graft rejection and complications.
- Gene Therapy: Although still in the experimental stage, gene therapy aims to correct genetic abnormalities that cause endothelial cell dysfunction. Early research in this area shows potential for future treatment strategies.
- Advanced Imaging and Monitoring: Advances in imaging techniques, such as anterior segment optical coherence tomography (AS-OCT) and confocal microscopy, enable more accurate monitoring of disease progression and response to treatment. These technologies enable detailed visualization of the corneal endothelium and anterior chamber structures, assisting in the early detection of complications and the optimization of treatment strategies.
Supportive Care
- Contact Lenses: In patients with chronic epithelial breakdown, therapeutic contact lenses can help manage corneal edema and improve comfort.
- Regular Monitoring: Frequent follow-up visits with an ophthalmologist are essential for tracking disease progression, adjusting treatment regimens, and avoiding complications like glaucoma-related optic nerve damage.
Healthcare providers can effectively manage ICE Syndrome by combining medical, surgical, and innovative approaches, preserving vision and improving patients’ quality of life.
Effective Ways to Treat and Prevent Irido Corneal Endothelial Syndrome
- Regular Eye Exams: Early detection through routine eye exams can result in prompt diagnosis and treatment, potentially avoiding serious complications.
- Manage Underlying Conditions: Managing systemic conditions like hypertension and diabetes can lower the risk of secondary glaucoma associated with ICE Syndrome.
- Protect Your Eyes: Wearing protective eyewear during activities that may cause eye trauma helps to prevent injuries that could aggravate endothelial cell abnormalities.
- Avoid Ocular Infections: Good hygiene and prompt treatment of any eye infections can help prevent complications that worsen ICE Syndrome.
- Follow Treatment Plans: Adhering to prescribed treatment regimens and attending regular follow-up appointments is critical for managing intraocular pressure and corneal health.
- Monitor for Symptoms: Being aware of changes in vision, such as increased blurriness, halos around lights, or eye discomfort, allows for timely intervention if symptoms worsen.
- Healthy Lifestyle: Leading a healthy lifestyle that includes a balanced diet, regular exercise, and quitting smoking improves overall eye health and lowers the risk of glaucoma.
- Educate Yourself: Staying informed about ICE Syndrome and its treatment can help patients take an active role in their care and seek timely medical advice.
- Apply Prescribed Eye Drops Correctly: Proper use of prescribed eye drops ensures maximum efficacy in controlling intraocular pressure and corneal edema.
- Seek Specialist Care: Consulting with corneal and glaucoma specialists ensures access to the most recent diagnostic and therapeutic advances, which improves patient outcomes with ICE Syndrome.
Trusted Resources
Books
- “Cornea” by Jay H. Krachmer, Mark J. Mannis, and Edward J. Holland
- “Glaucoma: Medical Diagnosis and Therapy” by Tarek M. Shaarawy, Mark B. Sherwood, Roger A. Hitchings, and Jonathan G. Crowston
- “Clinical Atlas of Ophthalmology” by David J. Spalton, Roger A. Hitchings, and Paul Hunter
Online Resources
- American Academy of Ophthalmology (AAO): www.aao.org
- National Eye Institute (NEI): www.nei.nih.gov
- Glaucoma Research Foundation: www.glaucoma.org
- EyeWiki: eyewiki.aao.org
- PubMed: pubmed.ncbi.nlm.nih.gov






