What is ischemic optic neuropathy?
Ischemic optic neuropathy (ION) is a condition that causes sudden loss of vision due to decreased blood flow to the optic nerves. This condition can affect one or both eyes and is typically divided into two types: anterior ischemic optic neuropathy (AION) and posterior ischemic optic neuropathy (PION). AION is more common and affects the front part of the optic nerve, whereas PION affects the rear. Early diagnosis and treatment are critical for preventing permanent vision loss.
Extensive Review of Ischemic Optic Neuropathy
Ischemic optic neuropathy (ION) is a major cause of sudden vision loss, especially in older adults. Understanding ION entails investigating its various types, pathophysiology, risk factors, clinical manifestation, complications, and epidemiology.
Types of Ischemic Optic Neuropathy
- Anterior ischemic optic neuropathy (AION):
- Non-Arteritic Anterior Ischemic Optic Neuropathy (NAION): This is the most common type, which is often associated with systemic conditions like hypertension, diabetes, or sleep apnea. It occurs when there is insufficient blood flow to the anterior portion of the optic nerve.
- Arteritic Anterior Ischemic Optic Neuropathy (AAION): This type is associated with giant cell arteritis (GCA), a blood vessel inflammatory condition. AAION is an ophthalmic emergency that requires immediate treatment to avoid further vision loss.
- Posterior Ischemic Optic Neuropathy (PION):
PION is less common than AION and affects the retrobulbar portion of the optic nerve. It is divided into three types: arteritic, non-arteritic, and perioperative PION, with the latter frequently associated with surgeries involving significant blood loss or prolonged hypotension.
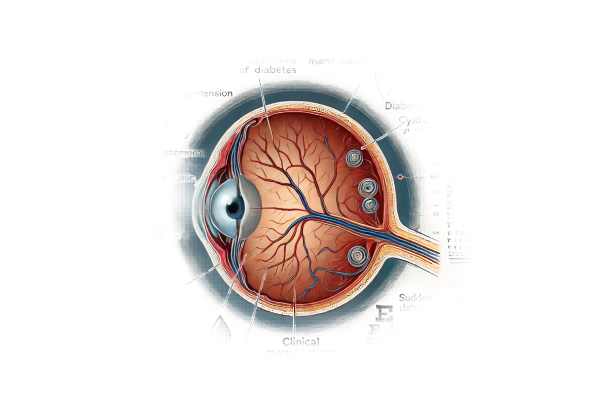
Pathophysiology
Reduced blood flow to the optic nerve causes ischemia and subsequent damage, which is the underlying mechanism of ION. The optic nerve is dependent on a delicate balance of blood supply from the posterior ciliary arteries and the small branches of the ophthalmic artery. Any disruption in this supply can cause ischemia and infarction of the optic nerve fibers.
- NAION: Although the exact cause is not always known, NAION is frequently associated with nocturnal hypotension or a small, crowded optic disc (disc at risk). The condition typically appears upon waking and is thought to be caused by a drop in blood pressure during sleep, resulting in insufficient perfusion of the optic nerve.
- AAION: AAION is caused by inflammation of the blood vessels (vasculitis) in GCA, which leads to occlusion of the arteries that supply the optical nerve. The inflammatory process causes thickening and narrowing of the vessel walls, reducing blood flow and resulting in ischemia.
Risk Factors
Several factors raise the risk of developing ION.
- Age: ION primarily affects people over the age of 50, and the incidence rises with age.
- Cardiovascular Disease: Hypertension, atherosclerosis, and diabetes mellitus are major risk factors due to their effects on blood vessels.
- Sleep Apnea: Obstructive sleep apnea is associated with NAION, possibly due to repeated episodes of hypoxia and nocturnal hypotension.
- Giant Cell Arteritis: This condition is a major risk factor for AAION, especially in people over 70 years old.
- Genetic Factors: A family history of ION or related vascular conditions may increase risk.
- Medications: Some medications, such as phosphodiesterase inhibitors used to treat erectile dysfunction, have been linked to NAION.
Clinical Presentation
The symptoms and signs of ION differ according to the type and severity of the condition:
- NAION:
- Sudden Vision Loss: Usually painless and occurs upon waking. A “curtain coming down” or a dark spot in the visual field are common descriptions of vision loss.
- Visual Field Defects: Altitudinal field defects are most common, affecting either the upper or lower half of the visual field.
- Swollen Optic Disc: Examination reveals a swollen optic disc with peripapillary hemorrhages.
- AAION:
- Severe Vision Loss: Often more severe than NAION and can happen quickly.
- Systemic Symptoms: GCA can cause headaches, scalp tenderness, jaw claudication, and fatigue.
- Swollen and Pale Optic Disc: The optic disc is usually swollen and pale, indicating severe ischemia.
- PION:
- Vision Loss: Sudden and painless vision loss, usually bilateral in perioperative cases.
- Normal Optic Disc: The optic disc appears normal at first, but atrophy gradually develops over weeks.
Complications
ION can cause a number of complications, most notably persistent vision loss and its impact on quality of life:
- Chronic Visual Impairment: Permanent vision loss is common, especially in severe cases or when treatment is delayed.
- Second Eye Involvement: There is a risk that the condition will affect the other eye, particularly in NAION and AAION.
- Psychosocial Impact: Significant vision loss can lead to depression, anxiety, and a lower quality of life.
Epidemiology
ION is a significant cause of vision loss, especially in older adults.
- Incidence: The most common form is NAION, which has an estimated annual incidence of 2-10 per 100,000 people over the age of 50. AAION is less common, but more severe.
- Demographics: ION primarily affects people over 50, with AAION being more common in women due to the higher prevalence of GCA in women.
- Geographic Variation: The incidence of ION can vary depending on geography and ethnicity, indicating the prevalence of underlying risk factors such as GCA and cardiovascular disease.
Methods to Diagnose Ischemic Optic Neuropathy
A comprehensive clinical evaluation, imaging studies, and laboratory tests are required to confirm the diagnosis and identify underlying causes of ischemic optic neuropathy.
Clinical Evaluation
- Patient History: A thorough history is required to determine symptoms, onset, and risk factors. Patients with AAION frequently report systemic symptoms such as headaches and jaw pain, whereas those with NAION may have a history of heart disease or sleep apnea.
- Visual Acuity and Field Testing: Key diagnostic steps include determining the extent of vision loss and identifying specific visual field defects, such as altitudinal defects in NAION.
- Ophthalmoscopy: A direct examination of the optic disc reveals distinctive changes:
- NAION: A swollen optic disc with peripapillary hemorrhages.
- AAION: The optic disc is pale and swollen, indicating severe ischemia.
Imaging Studies
Imaging is critical for confirming the diagnosis and ruling out other causes of optic neuropathy.
- Optical Coherence Tomography (OCT): This non-invasive imaging technique produces detailed cross-sectional images of the optic nerve head and retinal nerve fiber layer, assisting in determining the extent of damage and monitoring progression.
- Fluorescein Angiography: This imaging technique involves injecting a fluorescent dye into the bloodstream to see how blood flows in the retina and optic nerve head. It can detect areas of reduced perfusion, which are indicative of ischemia.
- Magnetic Resonance Imaging (MRI): An MRI of the brain and orbits can rule out other causes of optic neuropathy, such as compressive lesions, and examine the optic nerves for signs of ischemia or inflammation.
Lab Tests
Laboratory tests are especially important for diagnosing AAION and determining underlying systemic conditions:
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): Elevated levels of these inflammatory markers strongly suggest GCA in patients with AAION.
- Temporal Artery Biopsy: This definitive test for GCA entails taking a small sample of the temporal artery and looking for characteristic inflammatory changes. It is critical for diagnosing AAION and determining treatment.
- Blood Glucose and Lipid Profile: These tests aid in identifying underlying cardiovascular risk factors, such as diabetes and hyperlipidemia, that are associated with NAION.
Treating Ischemic Optic Neuropathy Effectively
The treatment of ischemic optic neuropathy (ION) aims to address the underlying causes, reduce the risk of further vision loss, and alleviate associated symptoms. Treatment strategies vary depending on whether the condition is anterior (AION) or posterior (PION), arteritic (associated with giant cell arteritis, GCA), or non-arteritic. Here, we look at the available treatment options, emphasizing innovative and emerging therapies.
Medical Management
- Non-arteritic anterior ischemic optic neuropathy (NAION):
- Observation and Supportive Care: Because there is no definitive treatment to reverse vision loss, NAION is frequently managed through observation and supportive care. Patients should maintain overall cardiovascular health to reduce the risk of recurrence.
- Control of Risk Factors: Managing underlying conditions such as hypertension, diabetes, and hyperlipidemia is critical. Patients are encouraged to manage their blood pressure, blood sugar, and cholesterol levels with medication and lifestyle changes.
- Aspirin: Some patients may be prescribed low-dose aspirin to reduce the risk of future episodes by improving blood flow and preventing clot formation.
- Arterial Anterior Ischemic Optic Neuropathy (AAION):
- Corticosteroids: Immediate high-dose corticosteroids, such as prednisone, are the primary treatment for AAION to reduce GCA-related inflammation and prevent further vision loss. Intravenous steroids are frequently used as the first line of treatment, followed by an extended course of oral steroids.
- Immunosuppressive Therapy: To treat steroid-resistant GCA or to reduce long-term steroid use, immunosuppressive agents such as methotrexate or tocilizumab may be considered.
- Posterior Ischemic Optic Neuropathy (PION):
- Addressing Underlying Causes: PION treatment focuses on addressing underlying causes, such as hypotension or anemia, particularly in perioperative settings. Maintaining adequate blood pressure and oxygenation during and after surgery is critical.
- Steroids and Anti-Inflammatories: In cases of inflammation or autoimmune conditions, steroids and other anti-inflammatory medications may be used.
Innovative and Emerging Therapies
- Neuroprotective Agents: Researchers are working to create neuroprotective drugs that can shield optic nerve cells from ischemic damage. These agents attempt to preserve vision by preventing cell death during an ischemic event.
- Stem Cell Therapy: New research suggests that stem cell therapy could provide a treatment by promoting the regeneration of damaged optic nerve cells. Although still experimental, this method shows promise for future applications.
- Gene Therapy: Gene therapy is under investigation as a treatment for hereditary and acquired optic neuropathies. This therapy, which delivers specific genes to affected cells, has the potential to correct underlying genetic defects or improve cellular resilience to ischemia.
- Advanced Imaging-Guided Interventions: The use of advanced imaging techniques, such as optical coherence tomography (OCT) and enhanced MRI, enables accurate diagnosis and monitoring of ION. These technologies allow for more effective treatment tailoring and monitoring of the condition’s progression or resolution.
Surgical Interventions
Surgical interventions are generally not first-line treatments for ION, but may be considered in certain cases:
- Decompression Surgery: Optic nerve sheath decompression has been used in some cases of NAION to reduce swelling and improve blood flow, but its effectiveness is still debated and not widely recommended.
Integrating these treatment options allows healthcare providers to effectively manage ischemic optic neuropathy, reduce the risk of complications, and improve the quality of life for affected individuals.
Effective Ways to Improve and Prevent Ischemic Optic Neuropathy
- Regular Eye Examinations: Have routine eye exams to monitor your eye health, especially if you have risk factors for ION. Early detection can help to manage underlying conditions and prevent vision loss.
- Control Blood Pressure: Maintaining a healthy blood pressure is critical. Hypertension poses a significant risk for ION. To maintain healthy blood pressure, follow your doctor’s medication and lifestyle recommendations.
- Manage Diabetes: Proper diabetes management, including diet, exercise, and medication, can reduce the risk of NAION. Keeping blood sugar levels stable is critical for cardiovascular health.
- Check Cholesterol Levels: High cholesterol can contribute to atherosclerosis, which raises the risk of ION. Regular check-ups and medications prescribed by your doctor can help control cholesterol levels.
- Use of Low-Dose Aspirin: For people who are at high risk for vascular events, low-dose aspirin therapy can help prevent clot formation and improve blood flow, lowering the risk of ION.
- Lifestyle Modifications: Leading a healthy lifestyle that includes regular exercise, a balanced diet, quitting smoking, and moderate alcohol consumption can significantly reduce the cardiovascular risk factors associated with ION.
- Treat Sleep Apnea: If you have obstructive sleep apnea, using a CPAP machine or other treatments to ensure adequate oxygenation while sleeping can lower your risk of NAION.
- Prompt Treatment of Giant Cell Arteritis: Early detection and corticosteroid treatment of GCA can prevent AAION and other serious complications. Report symptoms such as headaches, scalp tenderness, and jaw pain to your doctor right away.
- Avoid Hypotension: For patients undergoing surgery, particularly lengthy procedures, adequate blood pressure management both intraoperatively and postoperatively is critical to preventing PION.
- Stay Informed: Learn more about the risk factors and symptoms of ION. Being proactive about your health can help you and your doctor make informed decisions to protect your vision.
Trusted Resources
Books
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski
- “Neuro-Ophthalmology: Diagnosis and Management” by Grant T. Liu, Nicholas J. Volpe, and Steven L. Galetta
- “Ischemic Optic Neuropathies” by Sohan Singh Hayreh
Online Resources
- American Academy of Ophthalmology (AAO): www.aao.org
- National Eye Institute (NEI): www.nei.nih.gov
- Mayo Clinic: www.mayoclinic.org
- MedlinePlus: medlineplus.gov
- PubMed: pubmed.ncbi.nlm.nih.gov






