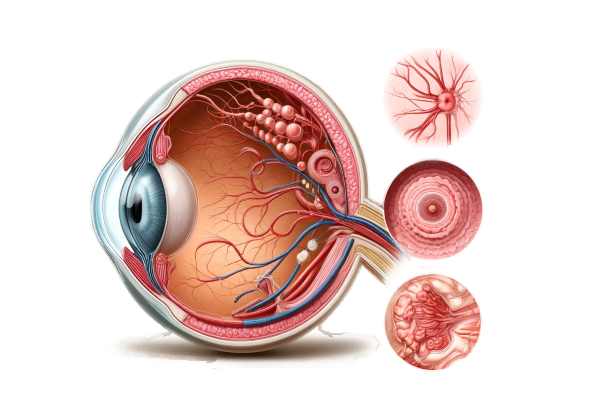
What is Optic Disc Pallor?
Optic disc pallor is a clinical sign that indicates a pale appearance of the optic disc, which is where the optic nerve enters the retina. This pallor is frequently indicative of underlying optic nerve damage or atrophy, and it can be associated with a variety of ocular and systemic conditions. The optic disc appears less pink and more white, indicating a loss of nerve fibers and blood flow. Optic disc pallor can cause visual impairment and requires a thorough investigation to determine the cause.
The Science Behind Optic Disc Pallor
Anatomy and Physiology of the Optic Disc
The optic disc, also known as the optic nerve head, is where the retinal nerve fibers come together to form the optic nerve, which transmits visual information from the retina to the brain. Normally, the optic disc appears pink due to its abundant blood supply and healthy nerve fibers. Any color changes, such as pallor, suggest an underlying pathology affecting the optic nerve.
Causes of Optical Disc Pallor
Optic disc pallor can have a variety of causes, including optic neuropathies, ischemic events, hereditary conditions, inflammatory processes, and compressive lesions.
- Optical Neuropathies:
- Optic Neuritis: Inflammation of the optic nerve, which is frequently associated with multiple sclerosis, can cause optic disc pallor after the acute phase.
- Leber’s Hereditary Optic Neuropathy (LHON): A genetic disorder that causes mitochondrial dysfunction and then optic nerve degeneration, resulting in pallor.
- Ischemic Event:
- Nonarteritic Anterior Ischemic Optic Neuropathy (NAION): Sudden vision loss caused by reduced blood flow to the optic nerve, which is common in older adults.
- Giant Cell Arteritis is an inflammatory condition that affects blood vessels and causes ischemic damage to the optic nerve.
- Hereditary Condition:
- Dominant Optic Atrophy: A genetic condition that causes progressive vision loss and optic nerve pallor, typically presenting in childhood.
- The Inflammatory Processes:
- Sarcoidosis is a systemic inflammatory disease that can affect the optic nerve, resulting in granulomatous inflammation and optic disc pallor.
- Infectious Causes: Infections such as syphilis, Lyme disease, and tuberculosis can all cause optic nerve inflammation and pallor.
- Compressive lesions:
- Tumors: Intracranial or orbital tumors can compress the optic nerve, causing atrophy and pallor.
- Hydrocephalus: Increased intracranial pressure can compress the optic nerve and cause pallor.
Clinical Presentation
Patients with optic disc pallor may experience a variety of symptoms, depending on the underlying cause and extent of optic nerve damage:
- Visual Acuity Loss is a loss of vision sharpness that can occur gradually or suddenly.
- Visual Field Defects include loss of peripheral vision or the presence of blind spots (scotomas) in the visual field.
- Color Vision Deficiency: Difficulty distinguishing colors or colors that appear washed-out.
- Reduced Contrast Sensitivity: Difficulty perceiving contrasts and subtle shades.
Pathophysiology
Optic disc pallor indicates underlying damage to the optic nerve fibers, resulting in a reduction in the optic disc’s normal pink coloration. Pathophysiology involves various mechanisms depending on the cause:
- Axonal Loss: Damage to the optic nerve fibers causes the loss of axons, resulting in a pale optic disc. This can result from direct injury, ischemia, or inflammatory processes.
- Reduced Blood Flow: Ischemic events such as NAION or giant cell arteritis reduce blood supply to the optic nerve, resulting in pallor and atrophy.
- Genetic Mutations: Hereditary conditions such as LHON and dominant optic atrophy involve genetic mutations that disrupt normal cellular function, resulting in optic nerve degeneration and pallor.
Differential Diagnosis
Several conditions can manifest as optic disc pallor, necessitating a thorough differential diagnosis to determine the underlying cause:
- Optic Neuritis: Acute inflammation of the optic nerve commonly causes pain and sudden vision loss, with optic disc pallor appearing later.
- Glaucoma: Chronically elevated intraocular pressure causes optic nerve damage and pallor, as well as characteristic changes in the shape of the optic disc.
- Retinal Diseases: Conditions such as retinitis pigmentosa can result in secondary optic disc pallor due to retinal degeneration.
- Nutritional Deficiencies: Vitamin B12 and folate deficiencies can cause optic neuropathy and pallor, respectively.
- Toxic Optic Neuropathy: Toxins like methanol and certain medications can damage the optic nerves and cause pallor.
Complications
Optic disc pallor can lead to several complications if the underlying cause is not identified and managed appropriately:
- Permanent Vision Loss: If the cause of optic nerve damage is not addressed, it can result in irreversible vision loss.
- Progression of Underlying Disease: Conditions such as multiple sclerosis or giant cell arteritis can have systemic consequences and necessitate immediate treatment to avoid further complications.
- Reduced Quality of Life: Visual impairment can have a significant impact on daily activities and overall well-being.
Prognosis
The prognosis for patients with optic disc pallor is dependent on the underlying cause and the timing of intervention. Early diagnosis and treatment of the underlying condition can improve outcomes and prevent future vision loss.
Methods to Diagnose Optic Disc Pallor
Diagnosing optic disc pallor requires a multifaceted approach that includes clinical evaluation, imaging studies, and laboratory tests to determine the underlying cause and the extent of optic nerve damage.
Clinical Evaluation
- Patient history:
- A thorough patient history is essential for determining potential risk factors, underlying conditions, and the onset and progression of symptoms. This includes inquiries about visual changes, pain, systemic symptoms, and a family history of ocular or systemic illnesses.
- Ophthalmoscopy:
- Direct examination of the optic disc with an ophthalmoscope is required to detect pallor. The color, shape, and margins of the optic disc are examined for any abnormalities that may indicate underlying pathology.
- Visual Acuity and Field Testing:
- These tests help determine the effect of optic nerve damage on vision. Visual acuity testing determines the clarity of vision, whereas visual field testing maps the patient’s field of vision to identify defects or blind spots.
Imaging Studies
- Optical Coherence Tomography (OCT):
- OCT can produce high-resolution cross-sectional images of the optic nerve head and retina. It is useful for evaluating the optic nerve’s structure, detecting retinal nerve fiber layer thinning, and visualizing any associated retinal abnormalities.
- Magnetic Resonance Imaging(MRI):
- An MRI of the brain and orbits is useful for detecting compressive lesions, such as tumors or structural abnormalities, which can cause optic disc pallor. Contrast-enhanced MRI can identify areas of inflammation or vascular abnormalities.
- Fundus Photography:*
- This imaging technique takes detailed photographs of the retina and optic disc, allowing for documentation of the appearance of the optic disc pallor and long-term monitoring of changes.
Lab Tests
- Blood test:
- A thorough blood examination can aid in determining systemic causes of optic disc pallor, such as infections, inflammatory conditions, and nutritional deficiencies. Tests may include a complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and specific antibody tests.
- Lumbral Puncture:
- When inflammatory or infectious causes are suspected, analyzing the cerebrospinal fluid (CSF) can provide useful diagnostic data. Elevated protein levels or the presence of specific antibodies may indicate a condition such as multiple sclerosis or neurosyphilis.
Treatment Options for Optic Disc Pallor
Addressing Underlying Causes
The treatment of optic disc pallor is primarily concerned with determining the underlying cause of optic nerve damage. Each potential cause of optic disc pallor necessitates a distinct treatment strategy:
- Optical Neuritis:
- Corticosteroids: High-dose intravenous corticosteroids are frequently used in combination with oral steroids to reduce inflammation and speed up vision recovery. This treatment is commonly used for optic neuritis associated with multiple sclerosis.
- Ischemic optic neuropathy:
- Management of Vascular Risk Factors: Controlling systemic conditions like hypertension, diabetes, and hyperlipidemia is critical. Antiplatelet therapy, such as aspirin, may be recommended to reduce the risk of future ischemic events.
- Steroids and Immunosuppressants: In cases of giant cell arteritis, high-dose corticosteroids are given immediately to prevent further vision loss and systemic complications. Long-term immunosuppressants may also be required.
- Hereditary Optic Neuropathies:*
- Genetic Counseling and Support: Genetic counseling can assist families in understanding inheritance patterns and associated risks. Current treatments are primarily supportive, but research into gene therapy shows promise for future management.
- Inflammatory Condition:
- Immunosuppressive Therapy: Certain conditions, such as sarcoidosis or systemic lupus erythematosus, may necessitate the use of immunosuppressive drugs such as methotrexate or azathioprine to control inflammation and prevent optic nerve damage.
- Antibiotics or antivirals: Antimicrobial therapies are used to treat infectious conditions such as syphilis and Lyme disease.
- Compressive lesions:
- Surgery: Surgical intervention may be required to remove tumors or relieve pressure on the optic nerve due to structural abnormalities.
Symptomatic Treatment and Support
- Low-Vision Aids:
- For patients with severe vision loss, low vision aids such as magnifying glasses, electronic reading devices, and adaptive technologies can help maximize remaining vision and improve quality of life.
- Visual Rehabilitation:
- Vision rehabilitation programs offer patients training and support to help them adapt to vision loss and improve their ability to perform daily tasks independently.
Innovative and Emerging Therapies
- Neuroprotective Agents:*
- Neuroprotective drugs that can protect optic nerve cells from further damage are currently under investigation. Agents like citicoline and brimonidine are being investigated for their ability to preserve vision in optic neuropathy.
- Genetic Therapy:
- Advances in gene therapy provide hope for treating hereditary optic neuropathy. Gene therapy, which corrects genetic mutations that cause optic nerve damage, has the potential to restore some vision. Early trials in conditions such as Leber’s Hereditary Optic Neuropathy (LHON) are yielding encouraging results.
- Stem Cell Treatment:
- Stem cell therapy is being investigated as a way to regenerate damaged optic nerve cells. This approach seeks to replace lost or damaged neurons, potentially restoring visual function.
- Electric Stimulation:
- Techniques such as transorbital alternating current stimulation (tACS) are being tested for their ability to stimulate optic nerve cells and improve visual function in patients with optic neuropathies.
Monitoring and Follow-up
Regular follow-up with an ophthalmologist or neuro-ophthalmologist is required to track the progression of optic disc pallor and evaluate the efficacy of treatments. Periodic visual acuity tests, visual field assessments, and imaging studies are critical for detecting changes early and adapting treatment plans accordingly.
Effective Methods to Improve and Avoid Optical Disc Pallor
- Regular Eye Examination:
- Schedule regular eye exams to monitor your vision and detect early signs of optic nerve damage. Early detection can prevent progression and allow for timely intervention.
- Controlling Vascular Risk Factors:
- Manage systemic conditions such as hypertension, diabetes, and hyperlipidemia with medication, diet, and lifestyle changes to reduce the risk of ischemic optic neuropathy.
- A Healthy Diet:
- Eat a well-balanced diet high in vitamins, antioxidants, and essential nutrients to improve overall eye health. Foods like leafy greens, nuts, and fish are healthy.
- Avoid smoking:
- Quit smoking and avoid secondhand smoke, as smoking can worsen vascular problems and contribute to optic nerve damage.
- Protective eyewear:
- Wear protective eyewear while participating in activities that pose a risk of eye injury to avoid trauma that could cause optic nerve damage.
- Stay hydrated:
- Maintain adequate hydration to promote vascular health and eye function.
- Managing Stress:
- Use stress-reduction techniques such as meditation, yoga, and regular exercise to improve overall health and reduce the impact of stress on systemic conditions that affect vision.
- Educate Yourself.
- Learn about optic disc pallor, its potential symptoms, and the significance of regular monitoring in managing the condition effectively.
- Prompt treatment of systemic conditions:
- Seek immediate medical attention if you have symptoms of a systemic condition that could affect your eyes, such as giant cell arteritis or autoimmune diseases.
Trusted Resources
Books
- “Clinical Neuro-Ophthalmology: A Practical Guide” by Ambar Chakravarty
- “Optic Nerve Disorders: Diagnosis and Management” by Jane W. Chan
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski and Brad Bowling






