What is Optic Nerve Sheath Meningioma?
Optic nerve sheath meningioma (ONSM) is a rare, usually benign tumor that develops in the meninges around the optic nerve. Because of their location and compression on the optic nerve, these tumors have the potential to cause progressive vision loss. Although slow-growing, optic nerve sheath meningiomas can have a significant impact on visual function and quality of life, necessitating careful diagnosis and management to preserve vision and avoid complications.
Detailed Insight into Optic Nerve Sheath Meningioma
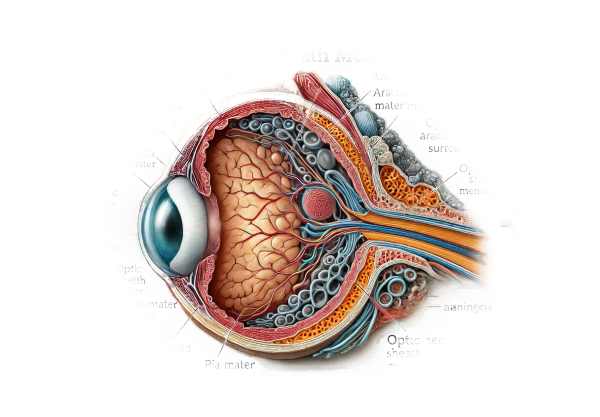
Anatomy and Pathophysiology
The optic nerve is an essential component of the visual system, transmitting visual information from the retina to the brain. The dura mater, arachnoid mater, and pia mater are the three meningeal layers that surround it. Optic nerve sheath meningiomas are those that develop from the meningeal layers surrounding the optic nerve. These tumors are typically benign and slow-growing, but they can cause significant damage to optic nerve fibers due to their compressive effect.
Epidemiology
Optic nerve sheath meningiomas are uncommon, accounting for only 1-2% of all orbital tumors and approximately 4% of all meningiomas. They are most frequently diagnosed in middle-aged adults, with women having a higher prevalence than men. Although ONSM can be sporadic, they are also linked to genetic conditions like neurofibromatosis type 2 (NF2).
Causes and Risk Factors
The exact cause of optic nerve sheath meningioma is not fully understood, but several factors are thought to contribute to its development:
- Genetic mutations:
- Mutations in the NF2 gene, which are associated with neurofibromatosis type 2, significantly increase the risk of developing meningiomas, including those affecting the optic nerve sheath.
- Radiation Exposure:
- Prior radiation exposure, particularly to the head and neck, is a known risk factor for meningiomas.
- Hormonal factors:
- The higher prevalence of ONSM in women suggests that hormonal factors, particularly estrogen, may contribute to the development of these tumors.
Clinical Presentation
Optic nerve sheath meningiomas are typically characterized by a variety of ocular and visual symptoms, including:
- Progressive vision loss:
The most common symptom is a gradual, painless loss of vision in one eye. The severity of vision loss in the affected eye can range from mild blurring to complete blindness. - Proptosis:
- Proptosis, or forward displacement of the eye, may occur as a result of tumor growth within the orbit.
- Optical Atrophy:
- Examination may reveal optic atrophy, a pale optic disc caused by chronic compression of the optic nerve fibers.
- Optical Disc Swelling:
- In some cases, optic disc swelling (papilledema) may occur, indicating increased intracranial pressure or direct tumor compression.
- Visual field defects:
- Patients may develop visual field defects, such as loss of peripheral vision or blind spots (scotomas).
- Pain:
- Although uncommon, some patients may experience pain or discomfort near the affected eye.
Pathophysiology
The pathophysiology of optic nerve sheath meningioma is characterized by the gradual compression of optic nerve fibers and surrounding structures by the tumor. The key mechanisms include:
- Mechanic Compression:
- The tumor’s growth causes direct pressure on the optic nerve fibers, resulting in ischemia, axonal damage, and eventually optic atrophy.
- Ischemia:
- Compression of the optic nerve can reduce blood flow, resulting in ischemic damage and further loss of nerve function.
- Inflammation:
- Chronic compression can cause an inflammatory response, worsening nerve damage and contributing to the progression of vision loss.
Complications
If left untreated, optic nerve sheath meningiomas can result in a number of serious complications, including:
- Permanent vision loss:
- Progressive damage to the optic nerve can lead to irreversible vision loss.
- Intercranial Extension:
- In some cases, the tumor may spread intracranially, affecting other cranial nerves and brain structures.
- Secondary Glaucoma:
- Increased intraocular pressure caused by tumor growth can lead to secondary glaucoma, which further impairs vision.
- Cosmetic concerns:
- Severe proptosis can cause cosmetic deformities, reducing the patient’s self-esteem and quality of life.
Prognosis
The prognosis for people with optic nerve sheath meningioma varies depending on the size and location of the tumor, its rate of growth, and the effectiveness of treatment. Early diagnosis and treatment are critical for maintaining vision and improving outcomes. Although ONSM are usually benign and slow-growing, they can have a significant impact on visual function if not treated properly.
Diagnostic Techniques for Optic Nerve Sheath Meningioma
Clinical evaluation, advanced imaging techniques, and, in some cases, histopathological examination are all required to make an accurate diagnosis of optic nerve sheath meningioma.
Clinical Evaluation
- Patient history:
- A complete patient history is required to determine the onset and progression of symptoms. The ophthalmologist will ask about the duration of the vision loss, any associated pain or discomfort, and the presence of systemic symptoms that could indicate a larger problem.
- Ophthalmological Examination:
- Visual Acuity Testing: This simple yet important test measures vision clarity to determine the severity of visual impairment. It is typically carried out using a Snellen chart or other age-appropriate visual acuity tests.
- Fundoscopy: A direct examination of the optic disc with an ophthalmoscope or a slit-lamp biomicroscope equipped with a fundus lens can reveal signs of optic atrophy or swelling. A pale optic disc or papilledema can indicate underlying pathology.
- Pupil Reactions: Examining the pupil’s response to light can reveal an afferent pupillary defect, indicating severe optic nerve dysfunction.
Imaging Studies
- Magnetic Resonance Imaging(MRI):
- MRI is the preferred imaging modality for diagnosing optic nerve sheath meningioma. It generates high-resolution images of the optic nerve and surrounding structures, allowing for a thorough evaluation of the tumor’s size, location, and extent. Gadolinium-enhanced MRI can help with tumor delineation and vascularity assessment.
- Computerized Tomography (CT) Scan:
- CT scans are useful for assessing bony changes in the orbit and optic canal. They can also detect calcifications within the tumor that are typical of meningiomas. CT imaging is especially useful when an MRI is either contraindicated or unavailable.
- Orbital ultrasound:
- Ultrasound imaging can reveal more information about the tumor’s characteristics and relationship to surrounding structures. It is an effective adjunctive tool, especially for determining orbital involvement.
Additional Diagnostic Tests
- Visual Field Test:
- Automated perimetry or other visual field tests can assist in quantifying visual field defects, such as scotomas or peripheral vision loss, which may be associated with optic nerve sheath meningioma. These tests provide a functional evaluation of the visual impact of the condition.
- Fluorescein Angiogram:
- This imaging technique involves injecting a fluorescent dye into the bloodstream to see the retinal and choroidal circulation. It can assist in detecting any vascular abnormalities or areas of ischemia associated with the tumor.
- Electrophysiological Test:
- In some cases, electrophysiological tests such as visual evoked potentials (VEP) may be used to evaluate the functional integrity of the optic nerve pathways. These tests assess the electrical responses of the visual cortex to visual stimuli and can help determine the severity of optic nerve dysfunction.
Optic Nerve Sheath Meningioma: Available Treatment Methods
Standard Treatment Options
Treatment for optic nerve sheath meningioma (ONSM) focuses on preserving vision, relieving symptoms, and controlling tumor growth. The tumor’s size, location, growth rate, and the patient’s overall health and visual function all influence the treatment decision.
- Observation:
- If the tumor is small, asymptomatic, and slow-growing, a conservative approach with frequent monitoring may be appropriate. This includes regular MRI scans and ophthalmic evaluations to monitor the tumor’s progression and visual function. Observation is particularly important for older patients or those with few symptoms.
- Radiation Therapy:
- Fractionated Radiotherapy: This method involves administering small doses of radiation over multiple sessions in order to minimize damage to surrounding tissues while targeting the tumor. Fractionated radiotherapy can effectively stop tumor growth and stabilize vision.
- Stereotactic Radiosurgery: Techniques like Gamma Knife and CyberKnife deliver highly focused radiation to the tumor while minimizing exposure to surrounding structures. Stereotactic radiosurgery is particularly effective for small to medium-sized tumors, providing a non-invasive treatment option with promising results.
- Surgical Resection:*
- Surgery may be considered for larger tumors that cause significant vision loss or are rapidly growing. The goal is to remove as much of the tumor as possible while keeping the optic nerve functional. Complete resection is difficult due to the tumor’s proximity to the optic nerve and other critical structures, and the risk of surgical complications is significant.
- In Combination Therapy:
- In some cases, a combination of surgery and radiation therapy may be used to improve tumor control while preserving vision. This approach can be tailored to the needs of each patient as well as the tumor’s specific behavior.
Innovative and Emerging Therapies
- Target Molecular Therapies:
- Studies on the molecular pathways involved in meningioma growth have resulted in the development of targeted therapies. Drugs that inhibit specific proteins or receptors that promote tumor proliferation, such as those inhibiting the PDGF (platelet-derived growth factor) and VEGF (vascular endothelial growth factor) pathways, are being studied for their potential to treat ONSM.
- Immunotherapy:
- Immunotherapy uses the body’s immune system to identify and attack cancer cells. Checkpoint inhibitors, which block proteins that prevent the immune system from attacking cancer cells, are being investigated for their potential use in treating meningiomas, including ONSM.
- Genetic Therapy:
- Gene therapy is the process of altering the genetic material within tumor cells to either stop their growth or make them more susceptible to other treatments. Although still in the experimental stage, gene therapy holds promise for the future treatment of ONSM and other tumors.
- Neuroprotective Agents:*
- Neuroprotective drugs seek to preserve optic nerve function while preventing further damage. Citicoline and brimonidine are being investigated for their ability to improve neural survival and function in patients with optic nerve compression.
Supportive Care
- Visual rehabilitation:
- Patients with severe vision loss can benefit from visual rehabilitation services, such as low vision aids, orientation and mobility training, and adaptive techniques, to improve their quality of life. These services help patients make the most of their remaining vision and maintain their independence.
- Psychological support:
- Living with a chronic condition, such as ONSM, can be challenging. Psychological support and counseling can help with emotional and mental health issues, including stress management strategies and overall well-being.
Monitoring and Follow-up
Regular follow-up with a multidisciplinary team, including ophthalmologists, neurologists, and oncologists, is required to monitor the patient’s condition, assess treatment efficacy, and manage any new complications. Periodic visual acuity tests, visual field assessments, and imaging studies are essential for monitoring changes and adjusting treatment plans as necessary.
Effective Ways to Improve and Prevent Optic Nerve Sheath Meningioma
- Regular Eye Examination:
- Schedule regular eye exams to detect vision changes early on and look for signs of optic nerve sheath meningioma. Early detection enables timely intervention and improved management.
- Awareness of symptoms:
- Be aware of the signs of optic nerve sheath meningioma, which include progressive vision loss, proptosis, and visual field defects. If you experience any of these symptoms, seek medical attention right away.
- Managing Risk Factors:
- Manage risk factors such as radiation exposure, particularly in the head and neck, which is known to increase the risk of meningiomas.
- Genetic counseling:
- Genetic counseling can help people with a family history of neurofibromatosis type 2 or other genetic predispositions understand their risk of developing optic nerve sheath meningiomas and make better family planning decisions.
- A Healthy Lifestyle:
- Live a healthy lifestyle, including a balanced diet, regular exercise, and quitting smoking, to improve overall health and potentially lower the risk of tumor development.
- Protect the eyes from trauma:
- Wear protective eyewear when participating in activities that may cause eye injury. Preventing trauma can lower the risk of exacerbating an existing optic nerve sheath meningioma or causing further ocular damage.
- Stay informed:
- Learn more about optic nerve sheath meningiomas and their potential complications. Understanding the condition allows you to take proactive measures to manage your eye health effectively.
- Treatment Plans:
- Follow the treatment plans and follow-up schedules recommended by your healthcare provider. Consistent monitoring and adherence to treatment can halt the progression of complications.
- Engage in Support Networks:
- Participate in support groups or online communities for people living with optic nerve sheath meningiomas or other similar conditions. Sharing experiences and strategies can offer both emotional support and practical advice.
Trusted Resources
Books
- “Clinical Neuro-Ophthalmology: A Practical Guide” by Ambar Chakravarty
- “Meningiomas: Diagnosis, Treatment, and Outcome” by Joung H. Lee and Dharampaul S. Masson
- “Neuro-Ophthalmology Illustrated” by Valérie Biousse and Nancy J. Newman
Online Resources
- American Academy of Ophthalmology (AAO)
- National Eye Institute (NEI)
- Brain Science Foundation
- National Organization for Rare Disorders (NORD)