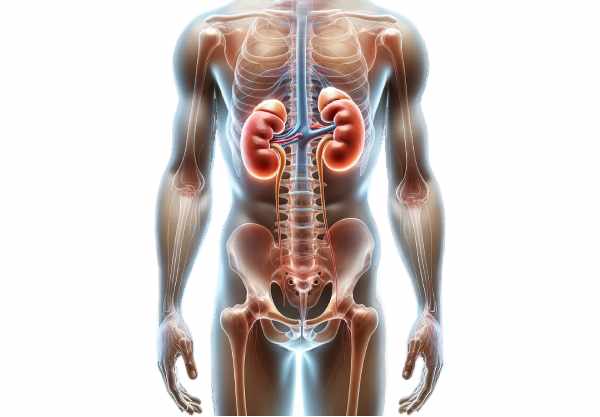
The kidneys are vital bean-shaped organs that play a crucial role in filtering blood, maintaining fluid and electrolyte balance, and regulating blood pressure. These highly efficient organs remove waste products and toxins from the body, contribute to metabolic functions, and produce essential hormones that influence overall health. Despite their small size, the kidneys perform complex tasks that are fundamental for homeostasis and longevity. In this guide, we explore the intricate anatomy of the kidneys, their multifaceted functions, common disorders affecting them, modern diagnostic methods, treatment options, and lifestyle strategies to keep your kidneys functioning optimally.
Table of Contents
- Anatomy & Structure
- Kidney Physiology & Functions
- Common Kidney Conditions
- Diagnostic Techniques
- Treatment Options & Interventions
- Nutritional Support & Supplements
- Lifestyle Practices for Kidney Health
- Trusted Resources & Further Reading
- Frequently Asked Questions
Anatomy & Structure
The kidneys are two bean-shaped organs located on either side of the spine in the retroperitoneal space. They measure approximately 11–14 cm in length, 6 cm in width, and 3 cm in thickness, with the right kidney positioned slightly lower than the left due to the liver’s presence.
External Anatomy
- Renal Capsule:
Each kidney is encased in a tough, fibrous capsule that provides structural protection and a barrier against infections and trauma. - Renal Cortex:
Just beneath the capsule lies the renal cortex, a granular, outer layer that contains the glomeruli and the majority of the nephrons. The cortex is the primary site for blood filtration and initial urine formation. - Renal Medulla and Pyramids:
The inner region, known as the renal medulla, comprises several cone-shaped structures called renal pyramids. Each pyramid ends in a renal papilla, through which urine drains into the minor calyces. - Renal Columns:
These are extensions of cortical tissue that separate the renal pyramids and provide a supportive framework for the kidney.
Internal Anatomy
- Nephrons – The Functional Units:
The kidney’s essential function of filtering blood is performed by approximately one million nephrons in each kidney. Each nephron consists of: - Glomerulus:
A tuft of capillaries where blood filtration begins. The high-pressure system forces water, electrolytes, and small molecules through the glomerular filtration barrier into Bowman’s capsule. - Bowman’s Capsule:
Surrounds the glomerulus and collects the filtrate that will be processed into urine. - Proximal Convoluted Tubule (PCT):
This segment reabsorbs the majority of water, ions, and nutrients such as glucose and amino acids from the filtrate back into the bloodstream. - Loop of Henle:
A U-shaped tube that further concentrates the urine. The descending limb is permeable to water, while the ascending limb actively transports sodium and chloride, creating an osmotic gradient. - Distal Convoluted Tubule (DCT):
In this section, additional reabsorption and secretion occur to fine-tune the filtrate composition. - Collecting Duct:
The final segment that adjusts urine concentration under the influence of hormones like antidiuretic hormone (ADH) before it is transported to the renal pelvis. - Renal Pelvis and Calyces:
The renal pelvis is a funnel-shaped cavity that collects urine from the minor calyces, which themselves collect urine from the renal papillae. Urine then passes from the renal pelvis into the ureter and ultimately to the bladder.
Blood Supply
- Renal Arteries and Their Branches:
Blood is supplied to the kidneys by the renal arteries, which arise directly from the abdominal aorta. These arteries branch into segmental, interlobar, arcuate, and interlobular arteries, ensuring a rich and efficient blood flow to every nephron. - Afferent and Efferent Arterioles:
Afferent arterioles deliver blood to the glomeruli, while efferent arterioles carry filtered blood away, branching into peritubular capillaries and the vasa recta, which are essential for nutrient exchange and maintaining the osmotic gradient necessary for urine concentration.
Nerve and Lymphatic Supply
- Renal Plexus:
The kidneys are innervated by both sympathetic and parasympathetic fibers. The sympathetic nervous system plays a significant role in regulating blood flow and renin secretion, which affects blood pressure. - Lymphatic Drainage:
Lymph from the kidneys drains into the lumbar lymph nodes, playing an important role in immune surveillance and fluid balance.
The sophisticated structure of the kidneys allows them to perform their functions efficiently, from blood filtration and urine production to hormone secretion and regulation of blood pressure.
Kidney Physiology & Functions
The kidneys are essential for maintaining homeostasis by filtering blood, balancing fluids and electrolytes, and eliminating waste products. Their functions extend well beyond urine formation, impacting overall health and metabolic regulation.
Filtration
- Glomerular Filtration:
The primary step in urine production occurs in the glomeruli, where blood pressure forces water, electrolytes, and small molecules through the filtration barrier into Bowman’s capsule. This filtrate forms the basis of urine and contains both useful and waste substances.
Reabsorption
- Proximal Convoluted Tubule (PCT):
Approximately 65% of the filtered substances are reabsorbed in the PCT. This includes water, glucose, amino acids, and bicarbonate, which are actively or passively transported back into the bloodstream. - Loop of Henle:
The loop of Henle plays a critical role in concentrating urine. The descending limb is permeable to water, allowing reabsorption, while the ascending limb actively transports sodium and chloride, creating an osmotic gradient. - Distal Convoluted Tubule and Collecting Duct:
These segments fine-tune urine composition by reabsorbing additional ions and water under hormonal regulation, particularly by ADH and aldosterone.
Secretion
- Tubular Secretion:
The kidneys actively secrete substances such as hydrogen ions, potassium, and certain drugs into the tubular fluid, ensuring that metabolic waste products and excess substances are removed from the body.
Acid-Base Regulation
- Maintaining pH Balance:
The kidneys contribute to the regulation of blood pH by reabsorbing bicarbonate and excreting hydrogen ions. This critical function helps maintain the acid-base balance within a narrow range.
Electrolyte and Fluid Balance
- Electrolyte Homeostasis:
The kidneys regulate the levels of sodium, potassium, calcium, and phosphate through selective reabsorption and secretion, which is essential for nerve function, muscle contraction, and overall cellular health. - Fluid Balance:
Through the controlled reabsorption of water, particularly under the influence of ADH, the kidneys maintain optimal blood volume and osmolality, which are crucial for blood pressure regulation.
Hormone Production
- Erythropoietin (EPO):
The kidneys secrete EPO in response to low oxygen levels, stimulating red blood cell production in the bone marrow. - Calcitriol:
The kidneys convert vitamin D into its active form, calcitriol, which enhances calcium absorption in the intestines and supports bone health.
Detoxification and Metabolic Functions
- Waste Elimination:
The kidneys remove metabolic waste products such as urea and creatinine from the blood, excreting them in urine. - Gluconeogenesis:
In times of fasting, the kidneys contribute to glucose production, helping to maintain blood sugar levels.
Through these processes, the kidneys are fundamental to maintaining the internal environment, ensuring that every cell receives the nutrients it needs while efficiently removing waste.
Common Kidney Conditions & Management
Kidney disorders can significantly impact overall health and lead to systemic complications. Early diagnosis and appropriate management are essential to preserve kidney function and prevent progression.
Chronic Kidney Disease (CKD)
- Overview:
CKD is characterized by a gradual loss of kidney function over time. It is often a consequence of conditions such as diabetes, hypertension, and glomerulonephritis. - Symptoms:
Early symptoms may include fatigue, changes in urine output, and swelling in the legs or feet. Advanced CKD can lead to anemia, bone disease, and electrolyte imbalances. - Management:
Treatment focuses on controlling blood pressure, managing blood sugar levels, and dietary modifications. Medications, lifestyle changes, and, in severe cases, dialysis or kidney transplantation are used to manage CKD.
Acute Kidney Injury (AKI)
- Overview:
AKI is a sudden decline in kidney function, often reversible if the underlying cause is promptly addressed. - Causes:
It can result from dehydration, severe infections, medications, or obstruction. - Symptoms:
Symptoms include reduced urine output, swelling, and elevated blood levels of creatinine and urea. - Management:
Management includes correcting the underlying cause, ensuring proper hydration, and monitoring electrolyte levels. Severe cases may require temporary dialysis.
Kidney Stones
- Overview:
Kidney stones are hard deposits formed from minerals and salts that crystallize in the kidneys. They can cause severe pain and obstruct the urinary tract. - Risk Factors:
Factors include dehydration, dietary imbalances, and genetic predisposition. - Symptoms:
Patients experience sharp pain in the back or side, hematuria (blood in the urine), and nausea. - Management:
Treatment may involve increased fluid intake, pain management, and medications to facilitate stone passage. In cases of large stones, lithotripsy or surgical removal may be necessary.
Urinary Tract Infections (UTIs) and Pyelonephritis
- Overview:
UTIs can affect any part of the urinary system, with pyelonephritis referring to infections that reach the kidneys. - Symptoms:
Symptoms include fever, flank pain, frequent urination, and burning during urination. - Management:
Treatment typically involves antibiotics, adequate hydration, and pain management. In recurrent or severe cases, further investigation and long-term management strategies are required.
Polycystic Kidney Disease (PKD)
- Overview:
PKD is a genetic disorder characterized by the development of numerous cysts in the kidneys, leading to progressive kidney enlargement and loss of function. - Symptoms:
Symptoms include high blood pressure, back or side pain, and urinary issues. PKD may progress to CKD over time. - Management:
Management focuses on controlling blood pressure, reducing cyst growth, and addressing complications. In advanced stages, dialysis or transplantation may be necessary.
Glomerulonephritis
- Overview:
Glomerulonephritis is the inflammation of the glomeruli, impairing the kidney’s ability to filter blood effectively. - Causes:
It can result from infections, autoimmune diseases, or certain medications. - Symptoms:
Symptoms include blood and protein in the urine, high blood pressure, and edema. - Management:
Treatment involves addressing the underlying cause, using immunosuppressive medications, and managing blood pressure and fluid balance.
Understanding these common kidney conditions is essential for early intervention and effective management to preserve kidney function and overall health.
Diagnostic Techniques & Evaluation Methods
Accurate diagnosis of kidney disorders is crucial for implementing effective treatment strategies. A comprehensive evaluation often combines clinical assessments, laboratory tests, and imaging techniques.
Clinical Evaluation
- Medical History:
A detailed history including symptoms, past medical conditions, and family history is essential. Patients are asked about changes in urine output, swelling, fatigue, and any risk factors such as diabetes or hypertension. - Physical Examination:
A thorough physical examination may reveal signs of fluid retention, high blood pressure, or abnormalities in kidney size and tenderness, which can point to underlying kidney dysfunction.
Laboratory Tests
- Blood Tests:
- Serum Creatinine and Blood Urea Nitrogen (BUN): Elevated levels indicate impaired kidney filtration.
- Electrolyte Panel: Assesses levels of sodium, potassium, and other electrolytes to evaluate kidney function.
- Glomerular Filtration Rate (GFR): An estimate of kidney filtering capacity calculated from serum creatinine levels.
- Urine Tests:
- Urinalysis: Evaluates the appearance, protein, glucose, and presence of blood cells in the urine.
- Urine Protein-to-Creatinine Ratio: Helps quantify proteinuria, an important marker of kidney damage.
- 24-Hour Urine Collection: Measures total protein excretion and creatinine clearance to provide a comprehensive assessment of kidney function.
Imaging Techniques
- Ultrasound:
A non-invasive imaging modality that visualizes kidney size, structure, and the presence of cysts, stones, or obstructions. It is the first-line imaging technique in kidney evaluations. - Computed Tomography (CT) Scan:
CT imaging provides detailed cross-sectional views, useful for detecting kidney stones, masses, and structural abnormalities. It can also evaluate the surrounding tissues for complications. - Magnetic Resonance Imaging (MRI):
MRI offers high-resolution images without ionizing radiation, making it valuable for assessing complex kidney conditions, vascular structures, and tumors. - Intravenous Pyelography (IVP):
Involves the injection of contrast dye to visualize the urinary tract, helping to identify obstructions and structural anomalies. - Renal Scintigraphy:
A nuclear imaging technique that evaluates kidney function and blood flow by using radiotracers, often used to assess differential renal function.
Specialized Tests
- Renal Biopsy:
A small sample of kidney tissue is obtained, usually with a needle, and examined under a microscope. Biopsy is crucial for diagnosing glomerulonephritis, interstitial nephritis, and other intrinsic kidney diseases. - Cystoscopy:
A procedure that involves inserting a scope through the urethra to view the bladder and ureteral orifices. This test can help detect abnormalities that may impact kidney function. - Urodynamic Studies:
Evaluate bladder function and urine flow, providing insights into conditions that may affect kidney health indirectly through urinary tract dysfunction.
These diagnostic approaches provide a comprehensive evaluation of kidney function and structure, guiding clinicians toward the appropriate treatment plan.
Treatment Strategies & Therapeutic Interventions
Effective management of kidney disorders is essential for preserving kidney function and overall health. Treatment strategies vary based on the specific condition and its severity and may include lifestyle modifications, medications, interventional procedures, and, in severe cases, renal replacement therapy.
Lifestyle Modifications
- Dietary Adjustments:
A kidney-friendly diet is low in sodium, protein (if kidney function is impaired), and phosphorus while being rich in fruits, vegetables, and whole grains. This helps reduce the workload on the kidneys and manage blood pressure. - Hydration:
Adequate fluid intake supports kidney filtration and prevents the formation of kidney stones, though fluid recommendations may vary depending on individual kidney function. - Weight Management:
Maintaining a healthy weight alleviates pressure on the kidneys and helps control blood pressure and diabetes, two major risk factors for kidney disease. - Exercise:
Regular, moderate exercise improves cardiovascular health and blood circulation, which benefits overall kidney function. - Smoking Cessation:
Quitting smoking improves blood flow and reduces the risk of kidney disease progression. - Limit Alcohol Consumption:
Excessive alcohol can damage the kidneys over time; moderation is key.
Pharmacologic Treatments
- Antihypertensives:
Medications such as ACE inhibitors and ARBs are used to control blood pressure while also reducing proteinuria and protecting kidney function. - Diuretics:
These medications help manage fluid retention and lower blood pressure, reducing the strain on the kidneys. - Phosphate Binders:
For patients with CKD, phosphate binders prevent high phosphate levels, which can cause bone disease and cardiovascular complications. - Erythropoiesis-Stimulating Agents (ESAs):
Used to manage anemia in CKD patients by stimulating red blood cell production. - Sodium Bicarbonate:
Administered to correct metabolic acidosis, a common complication in advanced kidney disease.
Renal Replacement Therapy
- Dialysis:
- Hemodialysis: Uses a machine to filter waste and excess fluids from the blood, typically performed several times per week at a dialysis center.
- Peritoneal Dialysis: Uses the lining of the abdomen (peritoneum) as a natural filter, offering greater flexibility and independence.
- Kidney Transplantation:
For end-stage renal disease, transplantation offers the best long-term outcomes. A donor kidney is surgically implanted, restoring kidney function and improving quality of life.
Surgical Interventions
- Kidney Stone Removal:
Procedures such as lithotripsy (shock wave therapy), ureteroscopy, or percutaneous nephrolithotomy are used to remove kidney stones that cause obstruction or severe pain. - Surgical Correction of Structural Abnormalities:
In cases of congenital or acquired structural issues, surgery may be required to correct anatomical defects that compromise kidney function.
Emerging and Innovative Therapies
- Stem Cell Therapy:
Investigational treatments using stem cells aim to regenerate damaged kidney tissue, offering hope for reversing chronic kidney disease. - Artificial Kidney Devices:
Research is underway to develop wearable or implantable artificial kidneys that could provide an alternative to traditional dialysis. - Precision Medicine:
Tailoring treatment based on genetic and biomarker information to optimize outcomes and minimize side effects.
By combining lifestyle modifications, pharmacologic interventions, and advanced treatment options, healthcare providers can tailor therapies to individual needs, thereby preserving kidney function and enhancing quality of life.
Nutritional Strategies & Supplements for Kidney Health
Nutrition plays a pivotal role in maintaining kidney health. A balanced diet combined with targeted supplements can support kidney function, reduce inflammation, and help prevent complications associated with kidney disease.
Essential Nutrients
- Omega-3 Fatty Acids:
Found in fish oil, flaxseed, and walnuts, omega-3s help reduce inflammation, improve blood pressure, and support overall cardiovascular health, which is crucial for kidney function. - Coenzyme Q10 (CoQ10):
An antioxidant that supports cellular energy production, CoQ10 can help protect kidney cells from oxidative damage and improve overall kidney function. - Vitamin D:
Adequate vitamin D levels are vital for calcium absorption and bone health. In kidney disease, vitamin D deficiency is common, so supplementation may help regulate calcium and phosphate balance. - Magnesium:
Magnesium supports proper nerve and muscle function and helps maintain electrolyte balance, which is essential for kidney health. - Vitamin C:
This antioxidant helps protect cells from oxidative stress and supports immune function, which is beneficial in reducing the risk of infections in kidney disease patients.
Herbal and Natural Supplements
- Milk Thistle:
Known for its liver-protective properties, milk thistle also benefits kidney function by promoting detoxification and reducing oxidative stress. - Astragalus:
An herb traditionally used in Chinese medicine, astragalus may help improve kidney function and reduce proteinuria in patients with chronic kidney disease. - Curcumin:
The active ingredient in turmeric, curcumin has potent anti-inflammatory and antioxidant properties that may help mitigate kidney inflammation and support overall function.
Antioxidant Support
- N-Acetylcysteine (NAC):
NAC boosts glutathione production, a critical antioxidant that helps reduce oxidative stress and inflammation in the kidneys. - Alpha-Lipoic Acid:
This antioxidant aids in energy metabolism and protects kidney cells from damage caused by free radicals.
Incorporating these nutrients and supplements, along with a balanced diet rich in fruits, vegetables, and lean proteins, can help maintain optimal kidney function and reduce the risk of kidney-related complications.
Lifestyle Practices for Kidney Wellness
A healthy lifestyle is crucial for maintaining kidney function and preventing disease. By adopting positive habits and avoiding harmful practices, you can protect your kidneys and support their vital functions.
Hydration and Diet
- Stay Hydrated:
Drinking adequate water helps flush toxins from the kidneys, reduces the risk of kidney stone formation, and supports overall kidney function. Aim for at least 8–10 glasses of water per day, but adjust based on your health and activity level. - Balanced Diet:
A diet low in sodium, processed foods, and unhealthy fats, while rich in fruits, vegetables, whole grains, and lean proteins, can reduce kidney workload. Limiting protein intake may be necessary for those with chronic kidney disease to prevent further damage. - Monitor Mineral Intake:
Managing levels of potassium, phosphorus, and calcium is essential, particularly for individuals with compromised kidney function.
Exercise and Weight Management
- Regular Physical Activity:
Engaging in moderate exercise such as walking, cycling, or swimming improves circulation, helps manage weight, and reduces blood pressure—all of which are beneficial for kidney health. - Maintain a Healthy Weight:
Excess body weight puts extra stress on the kidneys and increases the risk of conditions such as diabetes and hypertension. Achieving and maintaining a healthy weight is vital for long-term kidney health.
Avoiding Harmful Substances
- Quit Smoking:
Smoking impairs blood flow and can accelerate kidney damage. Quitting smoking is one of the best steps you can take to protect your kidneys. - Limit Alcohol Consumption:
Excessive alcohol can cause dehydration and increase the burden on the kidneys. Drinking in moderation supports overall kidney function. - Avoid Overuse of Medications:
Frequent use of over-the-counter pain relievers like NSAIDs can lead to kidney damage over time. Always follow dosing guidelines and consult your healthcare provider if you have concerns about medication use.
Regular Health Monitoring
- Routine Check-Ups:
Regular visits to your healthcare provider for blood pressure monitoring, blood tests (including kidney function tests), and overall health evaluations can detect early signs of kidney issues. - Manage Chronic Conditions:
Controlling conditions such as diabetes and hypertension is crucial for preventing kidney damage and preserving renal function.
By incorporating these lifestyle practices, you can create a supportive environment for your kidneys, promoting longevity and reducing the risk of kidney disease.
Trusted Resources & Further Reading
Staying informed about kidney health is essential for managing and preventing kidney-related disorders. Below are some trusted resources that provide up-to-date research, practical advice, and comprehensive information on maintaining kidney function.
Recommended Books
- “The Kidney Disease Solution” by Duncan Capicchiano:
This book provides insights into managing kidney disease naturally through diet and lifestyle changes, offering practical strategies to support kidney health. - “Coping with Kidney Disease: A 12-Step Treatment Program to Help You Avoid Dialysis” by Mackenzie Walser and Betsy Thorpe:
Offers a holistic approach to managing kidney disease, focusing on nutrition, lifestyle, and medical interventions to delay or prevent the need for dialysis. - “Dr. Sebi’s Alkaline and Anti-Inflammatory Diet for Beginners” by Samantha Plant:
Although focused on a broader dietary approach, this book provides useful strategies for maintaining overall health, including kidney function, through dietary modifications.
Academic Journals
- Journal of the American Society of Nephrology (JASN):
A leading source of research on kidney function, disease mechanisms, and innovative treatment options in nephrology. - Clinical Journal of the American Society of Nephrology (CJASN):
Publishes clinical research on kidney disease, offering insights into new therapies and management strategies for kidney conditions.
Mobile Apps
- MyKidneyCare:
A mobile app that helps track kidney health metrics, medications, and appointments, promoting proactive management of kidney disease. - WaterMinder:
An app designed to help users stay properly hydrated by tracking daily water intake, crucial for maintaining kidney function. - MyFitnessPal:
A comprehensive nutrition and exercise tracking app that supports weight management and overall health, which is vital for kidney wellness.
These resources offer valuable insights, scientific research, and practical tools to help you manage kidney health effectively and improve overall well-being.
Frequently Asked Questions About the Kidneys
What is the primary function of the kidneys?
The kidneys filter blood to remove waste products, regulate fluid and electrolyte balance, control blood pressure, and produce hormones essential for red blood cell production and bone health.
How do the kidneys maintain fluid and electrolyte balance?
The kidneys reabsorb water, electrolytes, and nutrients in the renal tubules while excreting waste and excess substances, a process regulated by hormones such as ADH, aldosterone, and natriuretic peptides.
What are common symptoms of kidney dysfunction?
Symptoms may include changes in urine output, swelling (edema), fatigue, high blood pressure, and, in advanced stages, nausea and confusion due to toxin buildup.
How is kidney disease diagnosed?
Diagnosis involves blood tests (e.g., serum creatinine, BUN, GFR), urine tests (urinalysis, protein-to-creatinine ratio), and imaging techniques such as ultrasound, CT scans, or MRI to evaluate kidney structure and function.
What lifestyle changes can improve kidney health?
Maintaining proper hydration, following a balanced diet low in sodium and processed foods, exercising regularly, managing blood pressure and blood sugar, and avoiding smoking and excessive alcohol all support kidney health.
Disclaimer:
The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a healthcare provider for personalized guidance.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about kidney health and overall wellness.