Orbital cellulitis is a serious bacterial infection that affects the tissues around the eye, such as the eyelids, brows, and cheek. It is usually caused by the spread of infection from the sinuses or direct trauma to the area around the eye. Staphylococcus aureus, Streptococcus pneumoniae, and Haemophilus influenzae are among the most common pathogens that cause orbital cellulitis. If not treated promptly, this condition can result in severe complications such as vision loss, abscess formation, and infection spreading intracranially.
Orbital cellulitis symptoms include redness and swelling around the eye, pain with eye movement, decreased vision, fever, and, in some cases, proptosis (eye bulging). A clinical examination, blood tests, and imaging studies such as computed tomography (CT) or magnetic resonance imaging (MRI) are typically used to confirm the diagnosis and assess the extent of the infection and any potential complications. Prompt recognition and treatment are critical to avoiding serious consequences and preserving vision.
Standard Treatments for Orbital Cellulitis
Management and treatment of orbital cellulitis necessitate a multifaceted approach that includes antimicrobial therapy, surgical intervention when necessary, and supportive care. Here are the standard treatments for managing orbital cellulitis:
- Antibiotic Therapy: Broad-spectrum intravenous antibiotics are the cornerstone of treatment for orbital cellulitis because they cover the majority of pathogenic bacteria. Initial empirical therapy frequently consists of a combination of antibiotics such as ceftriaxone or cefotaxime and clindamycin or vancomycin. Once culture results are available, the antibiotic regimen can be tailored to the identified pathogen and its sensitivities.
- Hospitalization: Because of the severity of the condition and the need for intravenous antibiotics, most patients with orbital cellulitis must be hospitalized. Continuous monitoring of the patient’s clinical status, including visual acuity and eye movements, is critical for detecting infection progression or complications.
- Surgical Intervention: Surgical drainage may be required if there is evidence of abscess formation, significant orbital involvement, or the patient does not respond adequately to antibiotic therapy. Abscesses and infected tissues can be drained using procedures such as functional endoscopic sinus surgery (FESS) or orbitotomy.
- Imaging Studies: Regular imaging studies, such as CT or MRI, are critical for monitoring treatment response and detecting complications early on. Imaging aids in determining the need for surgical intervention and assessing the severity of the infection.
- Supportive Care: Pain management, hydration, and monitoring for potential complications are all essential components of comprehensive care. If eyelid closure is impaired, patients may require additional interventions such as fever-reducing antipyretics and cornea-protecting ophthalmic ointments.
- Follow-Up Care: After leaving the hospital, patients need close outpatient follow-up to watch for recurrence or late complications. Regular ophthalmologic evaluations and imaging studies are part of the follow-up treatment plan.
Latest Innovations in Orbital Cellulitis Care
Recent advances in medical research and technology have resulted in novel approaches that provide new hope for orbital cellulitis patients. These cutting-edge innovations include advanced diagnostic techniques, novel antimicrobial therapies, minimally invasive surgical procedures, immunotherapy, and integrative care models. Each of these innovations offers distinct advantages and has the potential to improve orbital cellulitis management.
Advanced Diagnostic Techniques
Diagnostic technology advancements have greatly improved the accuracy and efficiency with which orbital cellulitis can be diagnosed and monitored.
Rapid Molecular Diagnostics: Traditional pathogen identification methods can take days. Rapid molecular diagnostic techniques, such as polymerase chain reaction (PCR) and next-generation sequencing (NGS), allow for faster and more accurate identification of the causative bacteria. These technologies enable timely adjustments to antibiotic therapy based on the pathogen, resulting in better patient outcomes.
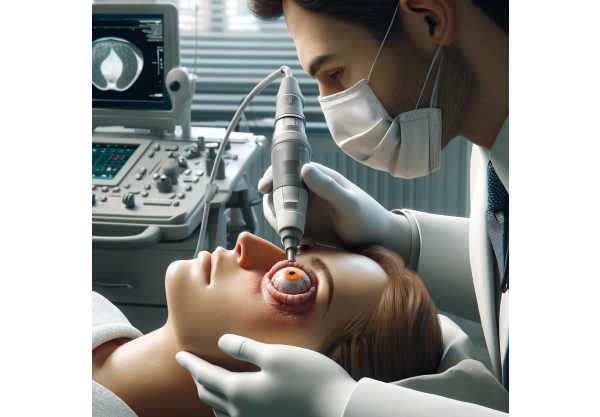
Point-Of-Care Ultrasound: Point-of-care ultrasound (POCUS) is increasingly being used as a bedside tool for diagnosing orbital cellulitis. POCUS can quickly assess the extent of soft tissue swelling, abscess formation, and involvement of adjacent structures. This non-invasive imaging modality improves the ability to make quick clinical decisions and monitor treatment outcomes.
Novel Antimicrobial Therapies
Innovative antimicrobial therapies are being developed to address antibiotic resistance and improve treatment efficacy for orbital cellulitis.
Phage Therapy: Bacteriophage therapy employs viruses that selectively target and kill bacteria. Phage therapy is being investigated as an alternative or adjunct to traditional antibiotics, particularly for multidrug-resistant infections. This method provides a targeted way to eliminate pathogenic bacteria while preserving the beneficial microbiota.
Antimicrobial peptides Antimicrobial peptides are small proteins with broad-spectrum antimicrobial activity. These peptides can disrupt bacterial membranes, making them effective against a variety of pathogens, including antibiotic-resistant strains. Antimicrobial peptides are being studied as a potential new class of therapeutic agents for bacterial infections such as orbital cellulitis.
Nanotechnology-Based Drug Delivery: Nanotechnology is being used to improve antibiotic delivery directly to the source of infection. Nanoparticles can be engineered to transport antibiotics and release them in a controlled manner, increasing the drug concentration at the infection site while reducing systemic side effects. This targeted approach has the potential to improve treatment efficacy for orbital cellulitis.
Minimally Invasive Surgical Procedures
Minimally invasive surgical techniques are transforming the treatment of orbital cellulitis by shortening recovery times and reducing complications.
Endoscopic Sinus Surgery: Functional endoscopic sinus surgery (FESS) is a minimally invasive procedure for draining sinus infections that lead to orbital cellulitis. Using an endoscope, surgeons can access and clear infected sinuses while causing minimal disruption to surrounding tissues. FESS is associated with shorter hospital stays, faster recovery, and less postoperative discomfort than traditional open surgery.
Image-Guided Surgery: Image-guided surgical systems use real-time imaging to help surgeons navigate and perform precise procedures. These systems improve the accuracy of procedures such as abscess drainage and debridement for orbital cellulitis. Image-guided surgery reduces the risk of complications and improves surgical outcomes by allowing for detailed visualization of the affected area.
Immunotherapy and Host-Directed Therapeutics
Immunotherapy and host-directed therapies are being developed to strengthen the body’s natural defenses against infections such as orbital cellulitis.
Immunomodulatory Agents: Immunomodulatory agents can alter the immune response to infection, increasing the body’s ability to combat pathogens. Monoclonal antibodies and cytokine inhibitors are being studied for their ability to improve immune function and reduce inflammation during bacterial infections.
Vaccines: Preventative vaccines against common pathogens that cause orbital cellulitis, such as Haemophilus influenzae and Streptococcus pneumoniae, can reduce the risk of infection. Vaccination programs for at-risk populations, such as children and those with chronic sinusitis, can significantly reduce the prevalence of orbital cellulitis.
Integrative and complementary therapies
Integrative approaches combine conventional medical treatments with complementary therapies to provide comprehensive care for patients suffering from orbital cellulitis.
Nutritional Support: Proper nutrition is essential for immune system support and infection recovery. Nutritional interventions, such as the administration of specific vitamins and minerals that boost immune function, can supplement antibiotic therapy and improve patient outcomes.
Herbal Medicine: Certain herbs, such as echinacea and garlic, have antimicrobial and immune-boosting effects. While more research is needed, these herbs may be used in conjunction with conventional antibiotics to help manage bacterial infections.
Probiotics: Probiotics, or beneficial bacteria, can aid in the maintenance of a healthy microbiota in the body. Probiotic supplementation may reduce the risk of secondary infections and improve overall immune health, which could benefit patients receiving antibiotic treatment for orbital cellulitis.
Personalized Medicine
Personalized medicine tailors treatment plans to each patient’s unique characteristics, including genetics, lifestyle, and disease manifestations.
Genomic Testing: Advances in genomic testing enable the identification of genetic factors that may affect a patient’s susceptibility to infections and response to treatment. Understanding these genetic factors can help guide personalized treatment strategies, ensuring that patients receive the most effective therapies based on their individual genetic makeup.
Lifestyle and Environmental Modifications: Personalized medicine emphasizes the importance of lifestyle and environmental factors in treating orbital cellulitis. Patients can benefit from personalized recommendations for hygiene practices, environmental modifications to reduce pathogen exposure, and lifestyle changes that promote immune health.
Artificial Intelligence, Machine Learning
The application of artificial intelligence (AI) and machine learning (ML) in healthcare has the potential to transform the treatment of orbital cellulitis.
AI-Powered Diagnostics: AI algorithms can analyze large datasets of clinical and imaging data to identify patterns and forecast disease progression. AI-powered diagnostics can improve the accuracy and efficiency of detecting orbital cellulitis, allowing for earlier intervention and personalized treatment strategies.
Predictive Modeling: Machine learning models can forecast the likelihood of complications and guide treatment decisions based on individual patient data. Predictive modeling assists clinicians in developing proactive management plans, which improves long-term outcomes for patients with orbital cellulitis.






