What is Polychromatic Cataract?
Polychromatic cataract is a rare but intriguing type of cataract in which multiple colors appear within the lens opacity. Polychromatic cataracts, as opposed to typical cataracts, which usually appear as a cloudy or opaque area within the lens, show a spectrum of colors when examined under a slit-lamp. A number of factors can contribute to this condition, including a genetic predisposition, metabolic disorders, or exposure to specific chemicals and medications. The multicolored opacities can scatter light entering the eye, causing significant visual disturbances like glare, halos around lights, and decreased visual acuity.
Patients with polychromatic cataract frequently report distinct visual symptoms as a result of light diffraction and dispersion by colored opacities. These symptoms vary according to the size, location, and density of the cataract within the lens. Early detection and accurate diagnosis are critical for the successful management of this condition. Ophthalmologists typically use advanced diagnostic tools, such as slit-lamp biomicroscopy, to identify and assess the severity of the cataract. Understanding the underlying cause of polychromatic cataract is critical for determining the best treatment approach, which may include addressing any associated systemic conditions as well as treating the cataract itself.
Polychromatic Cataract Management and Treatment
The management and treatment of polychromatic cataracts involve a combination of non-surgical and surgical approaches aimed at improving vision and addressing the root causes. Standard treatment methods aim to alleviate symptoms and restore visual function.
Non-Surgical Management: In the early stages of polychromatic cataract, non-surgical interventions may be adequate to alleviate symptoms. These interventions include using prescription eyeglasses or contact lenses to correct refractive errors and improve visual acuity. Anti-glare coatings on lenses can help reduce glare and improve comfort, particularly in bright light conditions. Additionally, lifestyle changes such as wearing UV-protective sunglasses and avoiding exposure to bright lights can help alleviate symptoms.
Pharmacological Treatment: Although no medications can reverse cataracts, some pharmacological treatments may help slow the progression of cataract formation. Antioxidant supplements, such as vitamins C and E, lutein, and zeaxanthin, have been investigated for their ability to protect the lens from oxidative damage. Patients with early-stage cataracts may benefit from these supplements, which may delay the need for surgical intervention.
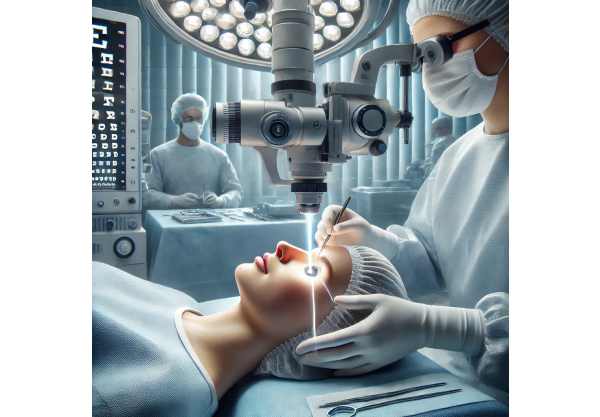
Surgical Intervention: When polychromatic cataracts severely impair vision and daily activities, surgical intervention is required. Cataract surgery is the most effective way to restore vision to patients with advanced cataracts. The standard procedure, known as phacoemulsification, involves breaking up the cloudy lens with ultrasound energy before removing it through a small incision. An artificial intraocular lens (IOL) is inserted to replace the natural lens and restore clear vision.
Types of Intraocular Lenses (IOLs): A variety of IOLs are available to meet the specific needs of patients with polychromatic cataracts. Monofocal IOLs provide clear vision from a single distance, whereas multifocal IOLs can focus at multiple distances, reducing the need for reading glasses. Toric IOLs are intended to correct astigmatism as well as cataracts, giving patients with this refractive error clearer vision. The patient’s visual requirements and the presence of any coexisting ocular conditions influence the IOL selection.
Postoperative Care: After cataract surgery, patients require careful postoperative care to ensure a full recovery and avoid complications. This includes using prescribed antibiotic and anti-inflammatory eye drops to reduce infection and inflammation. Regular follow-up visits with the ophthalmologist are required to monitor the healing process and address any issues that arise.
Innovative Polychromatic Cataract Treatment Methods
In recent years, the field of cataract treatment has made remarkable advances, with several novel technologies and techniques emerging to improve the management of polychromatic cataracts. These cutting-edge innovations aim to improve surgical precision, patient outcomes, and overall visual quality.
**1. **Femtosecond Laser-Assisted Cataract Surgery (FLACS).
Femtosecond laser-assisted cataract surgery (FLACS) is a significant advancement in cataract surgery, providing higher precision and control than traditional methods. This technology employs a femtosecond laser to perform critical steps in cataract surgery, such as corneal incisions, capsulotomy, and lens fragmentation.
- Technology: The femtosecond laser produces highly precise and reproducible corneal incisions and capsulotomies, which are required for proper intraocular lens (IOL) placement. The laser also softens the lens, allowing for easier removal with ultrasound energy during phacoemulsification.
- Benefits: FLACS improves surgical outcomes by lowering the risk of complications like capsular rupture and postsurgical astigmatism. The laser’s precision also enables better customization of the surgical procedure to the patient’s specific ocular anatomy, resulting in better visual outcomes and shorter recovery times.
**2. Intraocular lenses with extended depth of focus (EDOF).
Extended depth of focus (EDOF) intraocular lenses are a novel type of IOL that offers a continuous range of vision from distance to intermediate, with minimal visual disturbances. EDOF IOLs are especially beneficial for patients with polychromatic cataracts, as they can improve overall vision and reduce the need for additional corrective lenses.
- Technology: EDOF IOLs use advanced optics to increase the depth of focus, resulting in clear vision at a variety of distances. Unlike multifocal IOLs, which have distinct focal points, EDOF IOLs allow for a smooth transition of focus, reducing glare and halos.
- Benefits: Patients with EDOF IOLs have improved visual acuity over a wide range of distances, allowing them to perform daily activities without the need for reading glasses. This technology provides a more natural visual experience and increases patient satisfaction with postoperative outcomes.
3. Trifocal intraocular lenses
Trifocal intraocular lenses are the next generation of multifocal IOLs, with clear vision at near, intermediate, and distance ranges. These lenses are especially useful for patients with polychromatic cataracts because they address a broader range of visual needs while improving overall visual function.
- Technology: Trifocal IOLs have three distinct focal points in their design, allowing for the correction of both presbyopia and cataracts. This technology ensures that patients have clear vision for tasks like reading, computer work, and driving.
- Benefits: The use of trifocal IOLs reduces the need for glasses and improves visual performance across a variety of tasks. Patients express high levels of satisfaction with their visual quality and ability to seamlessly transition between distances.
**4. **Intraoperative Wavefront Aberrometry
Intraoperative wavefront aberrometry is a cutting-edge diagnostic tool for optimizing intraocular lens selection and placement during cataract surgery. This technology measures the eye’s refractive power in real time, providing precise data to help the surgeon achieve the best possible visual results.
- Technology: Wavefront aberrometry devices take precise measurements of the eye’s refractive errors and aberrations during surgery. This information is used to fine-tune the power of the IOL and ensure accurate alignment, particularly in patients with astigmatism.
- Benefits: Intraoperative wavefront aberrometry improves the accuracy of IOL placement and postoperative visual acuity. This technology is especially useful for patients with complex refractive profiles or those receiving premium IOL implantation.
5. Light-adjustable intraocular lenses (LALs)
Light-adjustable intraocular lenses (LALs) are a novel solution that enables postoperative adjustments to lens power via UV light. This technology provides unprecedented flexibility in achieving the best visual outcomes following cataract surgery.
- Technology: LALs are made of a special photosensitive material that can be reshaped when exposed to UV light. Following the initial surgery, patients receive a series of light treatments to fine-tune the lens power based on their visual requirements and preferences.
- Benefits: LALs have the distinct advantage of customizable vision correction, which allows for precise adjustments to achieve the desired refractive outcome. This technology minimizes the need for additional corrective procedures while increasing patient satisfaction with their visual results.
6. Robot-Assisted Cataract Surgery
Robotic-assisted cataract surgery is a cutting-edge approach that combines advanced robotic technology and the surgeon’s expertise. This method improves the precision and control of the surgical procedure, resulting in better outcomes for polychromatic cataracts patients.
- Technology: Robotic systems assist the surgeon in performing critical steps in cataract surgery, such as incision creation, capsulotomy, and lens fragmentation. The robotic platform provides real-time feedback and precise movements, reducing the possibility of human error.
- Benefits: Robotic-assisted surgery improves the accuracy and consistency of the procedure, resulting in better visual outcomes and fewer complications. Patients benefit from shorter recovery times and a lower risk of requiring additional surgical interventions.
**7. *Customized Cataract Surgery*
Customized cataract surgery involves tailoring the surgical procedure to each patient’s specific anatomical and visual needs. This method uses advanced diagnostic tools and surgical planning software to generate a personalized treatment plan.
- Technology: Preoperative imaging and diagnostic tests, such as corneal topography and optical coherence tomography (OCT), reveal important information about the patient’s eye. This information is used to tailor the surgical procedure, including the type and location of the IOL.
- Benefits: Customized cataract surgery ensures that each patient receives the best possible treatment for their specific condition, resulting in better visual outcomes and higher patient satisfaction. By addressing individual anatomical variations and refractive errors, this personalized approach improves the precision and effectiveness of cataract surgery.
**8. *Nanodroplet Cataract Treatment*
Nano-droplet cataract treatment is a new non-surgical approach that aims to dissolve cataracts with specially formulated eye drops. This novel approach to cataract treatment has the potential to revolutionize the field, especially for patients who are not ideal surgical candidates.
- Technology: Nano-droplet eye drops contain nanoparticles designed to penetrate the lens and break down the protein aggregates that cause cataract formation. These drops work by dissolving the cataract gradually, potentially restoring lens clarity without the need for invasive procedures.
- Benefits: If proven effective, nano-droplet treatment may provide a non-invasive, painless alternative to cataract surgery. This method would be especially beneficial for patients with early-stage cataracts or who are unable to undergo surgery due to medical reasons.
9. Gene Therapy
Genetic therapy is a ground-breaking approach to treating cataracts at the molecular level. By targeting the genetic factors that contribute to cataract formation, this therapy has the potential to prevent or reverse the condition.
- Technology: Genetic therapy uses viral vectors or other delivery systems to insert corrective genes into the eye’s lens cells. These genes can modify or repair the genetic mutations that cause cataract formation, promoting the restoration of normal lens transparency.
- Benefits: Genetic therapy may provide a long-term solution for cataract prevention, particularly in people who have a genetic predisposition to the condition. This method has the potential to reduce the prevalence of cataracts while eliminating the need for surgical intervention.
10. Corneal Inlays.
Corneal inlays are small devices implanted in the cornea to improve vision by changing how light enters the eye. Although corneal inlays are most commonly used to treat presbyopia, they may also benefit patients with polychromatic cataracts by improving overall vision.
- Technology: The inlay is inserted into the corneal stroma via a small incision, similar to LASIK. The device can improve depth of focus and reduce the need for reading glasses, making it a viable option for patients undergoing cataract surgery.
- Benefits: Corneal inlays provide another option for improving vision in cataract patients, particularly those seeking better near vision. This technology can supplement cataract surgery by offering a more comprehensive solution for visual rehabilitation.
11. Artificial Intelligence (AI) and Cataract Surgery
Artificial intelligence (AI) is becoming more widely used in cataract surgery to improve decision-making, surgical planning, and outcome assessment. AI-powered tools and algorithms can provide surgeons with valuable insights and support throughout the surgical procedure.
- Technology: AI systems use massive amounts of data from preoperative imaging, patient history, and surgical outcomes to create predictive models and recommendations. These tools can help with selecting the best IOL, predicting surgical challenges, and tracking postoperative outcomes.
- Benefits: The use of AI in cataract surgery can improve the procedure’s accuracy and consistency, resulting in better visual outcomes and fewer complications. AI-powered insights can also improve patient counseling and informed consent by providing precise, data-backed information about expected outcomes.
12. Teleophthalmology
Teleophthalmology uses telecommunication technology to provide remote consultations, diagnostics, and follow-up care for cataract patients. This approach increases access to specialized care while also allowing for more efficient disease management.
- Technology: Teleophthalmology platforms enable patients to communicate with ophthalmologists via video conferencing for virtual consultations. Remote diagnostic tools, such as digital imaging and portable devices, allow for comprehensive eye exams and monitoring from a distance.
- Benefits: Teleophthalmology improves patient access to care in remote or underserved areas by reducing the need for travel and increasing convenience. This approach also promotes continuous monitoring and timely interventions, resulting in better management of cataracts and other ocular conditions.






