Fungal keratitis is a serious, sight-threatening infection of the cornea that requires swift diagnosis and thoughtful management. With its global prevalence rising due to increased contact lens use, agricultural injuries, and changes in climate, the condition has gained urgency for both eye care professionals and patients. Fungal keratitis often presents subtly at first but can progress rapidly, resulting in vision loss if not addressed. This comprehensive guide provides a clear, up-to-date roadmap for understanding fungal keratitis: from risk factors and symptoms to conventional drug therapies, surgical strategies, and cutting-edge innovations shaping future care.
Table of Contents
- Condition Introduction and Global Trends
- Standard Therapeutic Approaches and Pharmacological Management
- Surgical Interventions and Procedural Care
- Emerging Technologies and Novel Treatments
- Research Pipeline and Upcoming Advancements
- Frequently Asked Questions
- Disclaimer
Condition Introduction and Global Trends
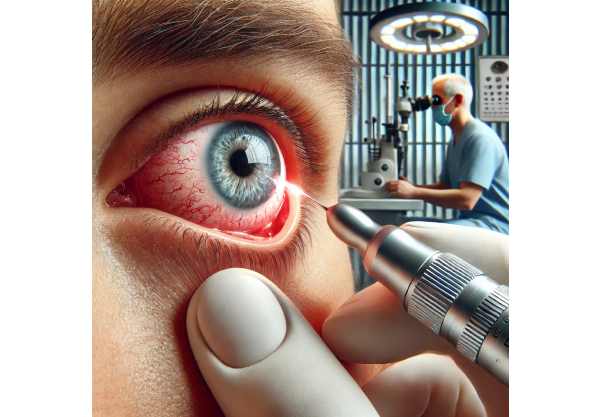
Fungal keratitis, also known as mycotic keratitis, is an infection of the cornea—the transparent front part of the eye—caused by a wide range of fungi. This condition is particularly prevalent in tropical and subtropical regions, where agricultural workers are at higher risk due to corneal injuries from plant material. However, in recent years, urban populations have seen increased incidence due to contact lens wear and topical corticosteroid use.
What Happens in Fungal Keratitis?
- The Process: Fungi invade the corneal tissue after minor trauma or due to underlying ocular surface disease. The most common culprits are Fusarium, Aspergillus, and Candida species.
- The Response: The body mounts an immune reaction that can result in inflammation, corneal melting, and, if left untreated, severe scarring or even perforation.
- Symptoms: Redness, pain, blurred vision, discharge, photophobia (light sensitivity), and a white or gray spot on the cornea.
Epidemiology and Global Burden
- Incidence: More than 1 million new cases occur worldwide each year, with higher rates in Asia, Africa, and South America.
- Demographics: Men and women of all ages are affected, but those in rural or agricultural settings are at greatest risk.
- Rising Trends: Increased use of topical steroids, climate change (altering fungal flora), and more widespread contact lens use are expanding the at-risk population.
Key Risk Factors
- Corneal trauma (especially with plant or soil exposure)
- Long-term use of contact lenses
- Prior corneal surgery or ocular surface disease
- Topical corticosteroid or antibiotic use
- Immunosuppression (systemic disease or medications)
Practical Advice for Patients
- Always protect your eyes when working outdoors or with plants.
- Never use contact lenses beyond recommended duration or care.
- If you experience sudden pain, redness, or blurred vision after eye injury or while wearing contacts, seek medical attention immediately—early intervention is crucial.
Diagnosis: Why Early and Accurate Identification Matters
- Clinical signs may mimic bacterial keratitis, delaying proper therapy.
- Microscopy and culture of corneal scrapings remain the gold standard, but newer diagnostic tools (see “Emerging Technologies”) are closing the gap for rapid diagnosis.
Standard Therapeutic Approaches and Pharmacological Management
Treating fungal keratitis is complex due to the organism’s resistance to many common antibiotics, the relative impermeability of the cornea to antifungal drugs, and the risk of rapid progression. Therapy focuses on targeted antifungal agents, supportive care, and careful monitoring.
First-Line Antifungal Medications
- Topical Natamycin 5%: First-choice for filamentous fungi (e.g., Fusarium, Aspergillus). Instilled every 1–2 hours initially, then tapered as infection resolves.
- Topical Amphotericin B 0.15–0.5%: Best for Candida and some other yeasts. Compounded in pharmacies due to limited commercial availability.
- Topical Voriconazole 1%: Broad-spectrum, often used as adjunct or for resistant infections.
- Adjunctive Therapy: Oral antifungals (e.g., itraconazole, voriconazole, fluconazole) in severe or deep infections, or if there is risk of scleral involvement.
Dosage and Duration
- Intensive, frequent dosing (hourly, even around-the-clock for the first 48 hours) is critical.
- Duration varies, but treatment generally continues for 4–8 weeks, guided by clinical improvement.
Supportive Care
- Cycloplegic drops (e.g., atropine) to relieve pain and prevent synechiae (iris sticking to lens).
- Pain control: Oral or topical non-steroidal anti-inflammatory drugs (NSAIDs), as directed.
- Steroid avoidance: Topical corticosteroids are typically avoided early on as they can worsen infection, except in rare, carefully monitored circumstances.
Monitoring and Adjusting Therapy
- Close follow-up is essential. Daily exams may be required in the initial stages.
- Therapy is adjusted based on clinical response and laboratory identification of the organism.
- Secondary bacterial infection may require added antibiotics.
Patient Guidance
- Never stop medications without your ophthalmologist’s guidance.
- Report any sudden worsening of symptoms or new pain immediately.
- Adherence is essential; missing doses can rapidly worsen prognosis.
Complications of Delayed or Inadequate Therapy
- Corneal perforation
- Irreversible scarring and vision loss
- Endophthalmitis (infection inside the eye), a medical emergency
Practical Tips
- Keep a medication diary or set reminders to avoid missed doses.
- Enlist support from family or friends for help with frequent drops.
Surgical Interventions and Procedural Care
Surgery is considered when medical management fails, or when complications threaten the structural integrity or function of the eye.
Procedures and Indications
- Debridement: Manual removal of infected corneal tissue to improve drug penetration and reduce organism load.
- Corneal Collagen Cross-Linking (CXL): An adjunctive therapy, particularly in early or recalcitrant cases, that strengthens corneal tissue and may inhibit fungal growth.
- Therapeutic Keratoplasty (Corneal Transplant): Required for deep, large, or non-responsive ulcers; urgent in cases of perforation. The infected cornea is replaced with healthy donor tissue.
- Amniotic Membrane Transplantation: Used in severe cases to promote healing and reduce inflammation.
Postoperative Management
- Intensive antifungal therapy continues after surgery to prevent recurrence.
- Careful monitoring for rejection, secondary infection, and healing is crucial.
- In some cases, multiple surgeries may be needed for full rehabilitation.
Potential Surgical Risks
- Graft rejection or failure
- Recurrence of infection in the graft
- Endophthalmitis or loss of vision
Innovations in Surgical Care
- Use of femtosecond lasers for precise corneal cuts during transplantation.
- Development of bioengineered corneal tissue to address donor shortages.
Rehabilitation and Long-Term Care
- Vision rehabilitation with corrective lenses or further surgery as needed.
- Psychological support for patients coping with vision loss or long recovery.
Advice for Patients
- Strict adherence to post-surgical instructions is essential.
- Avoid eye rubbing, protect the eye from trauma, and attend all follow-up appointments.
Emerging Technologies and Novel Treatments
The landscape of fungal keratitis management is rapidly evolving with the advent of novel diagnostics, drug delivery systems, and therapies.
Advanced Diagnostics
- Polymerase Chain Reaction (PCR): Allows rapid identification of fungal DNA from corneal samples, reducing time to targeted therapy.
- In Vivo Confocal Microscopy: High-resolution imaging detects fungal filaments in living tissue, aiding early diagnosis.
Novel Antifungal Agents
- New Azoles (e.g., Luliconazole, Efinaconazole): Under investigation for enhanced efficacy and corneal penetration.
- Drug-Eluting Contact Lenses: Deliver antifungal medications directly to the cornea for sustained, controlled release.
Innovative Delivery Methods
- Nanoparticle-based therapies: Improve drug stability, penetration, and targeted delivery.
- Sustained-release inserts: Placed under the eyelid, these gradually release antifungal agents, reducing dosing frequency.
Adjunctive Therapies
- Immunomodulators: Investigational therapies aim to modulate the immune response to reduce tissue damage.
- Biologic Dressings: Engineered to promote healing and reduce secondary infection.
AI and Digital Health
- AI-powered image analysis: Supports early diagnosis and tracking of ulcer progression.
- Tele-ophthalmology: Expands access to expert care in underserved areas, allowing remote triage and follow-up.
Personalized Medicine
- Genomic profiling: Identifying host and pathogen markers to tailor therapy for optimal outcomes.
Tips for Patients
- Ask your eye care provider about eligibility for clinical trials or access to innovative therapies.
- Stay updated through reputable ophthalmology resources and patient advocacy groups.
Research Pipeline and Upcoming Advancements
Ongoing research in fungal keratitis aims to improve diagnostic speed, drug efficacy, surgical success, and ultimately, patient quality of life.
Active and Upcoming Clinical Trials
- Comparative Studies of Antifungals: Head-to-head trials assessing new topical, oral, and injectable antifungals.
- Adjunctive Cross-Linking: Large-scale studies evaluating efficacy and safety as a standard adjunct to drug therapy.
- Nanotechnology Platforms: Trials of nanoparticles and new drug delivery systems to maximize corneal penetration and minimize toxicity.
Future Innovations in Surgery
- Bioengineered Corneas: Progress toward lab-grown corneal tissue suitable for transplantation.
- 3D-Printed Corneal Scaffolds: Promise customizable solutions for severe or recurrent disease.
Diagnostic Advancements
- Point-of-Care Testing Devices: Under development for rapid, on-site identification of fungal pathogens, enabling faster initiation of therapy.
- Wearable Eye Sensors: Being trialed for continuous monitoring of ocular surface health in high-risk patients.
Preventive Strategies
- Prophylactic therapies: Exploring preventive antifungal drops for high-risk populations.
- Vaccine development: Though still in early phases, research seeks to reduce incidence among agricultural workers and other vulnerable groups.
Patient Participation and Advocacy
- Joining patient registries and research studies not only supports science but may provide early access to breakthrough care.
- Advocacy and public health initiatives are raising awareness to reduce preventable blindness from fungal keratitis globally.
Advice for Clinicians and Patients
- Remain informed about emerging research and evolving guidelines.
- Early participation in clinical trials can benefit both individual patients and the wider community.
Frequently Asked Questions
What is the best treatment for fungal keratitis?
The best treatment is prompt use of topical antifungal eye drops, such as natamycin or amphotericin B, based on the suspected fungus. Severe or non-responsive cases may require oral medications or surgery. Early diagnosis and specialist care are crucial.
How is fungal keratitis diagnosed?
Diagnosis involves clinical examination, corneal scraping for microscopy and culture, and sometimes advanced imaging or PCR to rapidly detect fungal organisms.
Can fungal keratitis cause blindness?
Yes, if not treated early and aggressively, fungal keratitis can cause permanent vision loss due to corneal scarring or perforation. Immediate medical attention greatly improves outcomes.
How long does it take to recover from fungal keratitis?
Recovery varies widely, from several weeks to months. Early, appropriate treatment speeds healing and reduces complications, but some patients may need surgery or ongoing care for optimal vision.
Who is at risk for fungal keratitis?
Anyone can develop fungal keratitis, but risk is higher for agricultural workers, contact lens users, people with eye trauma, or those using topical steroids or with immune suppression.
Are there any new treatments for fungal keratitis?
Yes, new treatments include advanced antifungal agents, drug-eluting contact lenses, nanotechnology-based delivery, and improved surgical techniques. Participation in clinical trials can offer access to these innovations.
Disclaimer
This article is provided for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified eye care provider for any questions about your vision or eye health.
If you found this guide useful, please share it on Facebook, X (formerly Twitter), or your favorite platform, and follow us on social media. Your support helps us continue creating trusted, expert health content for all.






