Choroidal neovascularization (CNV) is a vision-threatening complication that arises when abnormal blood vessels grow beneath the retina, often linked to age-related macular degeneration, high myopia, or ocular injury. These new vessels are fragile and prone to leaking, causing swelling, bleeding, and scarring that can severely impair central vision. Early identification and comprehensive management are essential for preserving sight and quality of life. In this guide, we explore the full landscape of CNV—from foundational knowledge and gold-standard therapies to breakthrough innovations and future directions, providing practical, actionable information for patients, caregivers, and eye care professionals.
Table of Contents
- Choroidal Neovascularization Basics and Epidemiology
- Medical Management and Non-Surgical Therapies
- Surgical Procedures and Localized Interventions
- Advancements in Diagnosis and Cutting-Edge Treatments
- Ongoing Clinical Trials and Future Perspectives
- Frequently Asked Questions
Choroidal Neovascularization Basics and Epidemiology
Choroidal neovascularization refers to the abnormal growth of blood vessels from the choroid—the vascular layer beneath the retina—into the space under the retinal pigment epithelium or even the neurosensory retina. This process disrupts normal retinal architecture, posing a risk for vision loss if not managed promptly.
Common Causes of CNV
- Age-related macular degeneration (AMD): Most common cause, especially the “wet” form of AMD.
- Pathologic myopia: High degrees of nearsightedness may predispose to CNV.
- Ocular trauma or inflammation: Chorioretinitis, histoplasmosis, or angioid streaks.
- Genetic or hereditary retinal disorders: Such as Best disease or pattern dystrophies.
Epidemiological Facts
- CNV is most prevalent in adults over 50, especially those with AMD.
- “Wet” AMD, caused by CNV, accounts for 10–15% of AMD cases but leads to 90% of AMD-related vision loss.
- Myopic CNV tends to affect younger adults but is less common overall.
Symptoms and Early Signs
- Blurred or distorted central vision (metamorphopsia).
- A dark or gray spot in the center of vision (scotoma).
- Rapid decline in visual acuity, sometimes over days or weeks.
Risk Factors
- Advancing age, especially over 60.
- Family history of macular degeneration.
- Smoking, hypertension, and high cholesterol.
- Previous ocular injury or inflammation.
Practical Advice:
If you notice sudden vision changes, wavy lines, or blind spots, seek immediate evaluation by an eye care professional. Early detection allows for timely intervention and can preserve much of your vision.
Medical Management and Non-Surgical Therapies
Most cases of CNV are managed initially and primarily through non-surgical means, aiming to halt or reverse the growth of abnormal blood vessels.
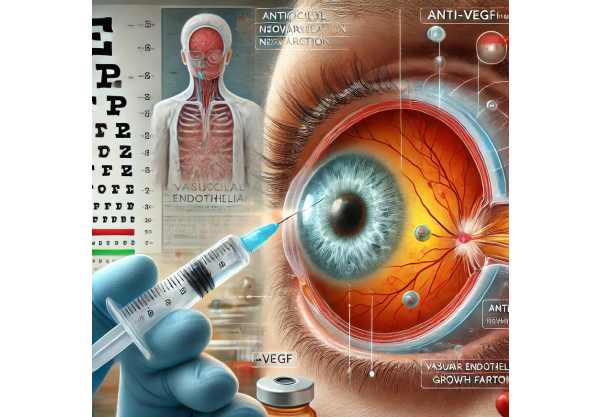
Anti-VEGF Injections (Mainstay of Therapy)
- Mechanism: Anti-VEGF agents (e.g., ranibizumab, aflibercept, bevacizumab, brolucizumab) block vascular endothelial growth factor, preventing the growth and leakage of new blood vessels.
- Administration: Intravitreal (in-the-eye) injections, often monthly for the first few months, then tailored to disease activity.
- Benefits: Proven to improve or stabilize vision in most patients; has revolutionized CNV treatment.
Other Pharmacologic Options
- Photodynamic Therapy (PDT): Involves injecting a light-sensitive drug (verteporfin) and activating it with a laser. Best for certain types of CNV, particularly where anti-VEGF is less effective or not tolerated.
- Corticosteroids: Sometimes used as adjunctive therapy, especially in inflammatory CNV or where fluid persists despite anti-VEGF treatment.
Supplemental and Supportive Measures
- Oral antioxidants/vitamins (AREDS formula): Recommended for AMD-related CNV to slow disease progression, though not directly treating CNV itself.
- Blood pressure and cholesterol control: Helps minimize risk of recurrence or progression.
Self-Care and Monitoring
- Amsler grid at home: A simple tool to detect early changes in vision.
- Healthy lifestyle: Diet rich in leafy greens, omega-3s, and regular exercise.
Practical Advice:
Stick closely to your injection schedule—even if your vision improves. Missing appointments can lead to disease recurrence and further vision loss. Notify your eye doctor immediately if you notice new symptoms between visits.
Surgical Procedures and Localized Interventions
While medical therapy remains the foundation, some patients with CNV benefit from surgical or advanced localized treatments, especially in complex or refractory cases.
Laser Photocoagulation
- Indications: Select CNV cases (well-defined, outside the foveal center).
- Procedure: A thermal laser is used to destroy abnormal vessels. Less commonly used now due to potential for scarring and central vision loss.
- Drawbacks: Can cause permanent blind spots, so reserved for peripheral lesions.
Submacular Surgery
- Purpose: Physical removal of CNV membranes beneath the retina.
- Applications: Mainly for nonresponsive cases or where vision is already severely compromised.
- Risks: Retinal detachment, bleeding, and variable visual outcomes.
Vitrectomy
- Occasionally used if there’s significant hemorrhage or scar tissue formation. May help restore or preserve vision in carefully selected cases.
Surgical Innovations
- Retinal prosthesis and tissue engineering: Being explored for cases with extensive damage, though still largely experimental.
Practical Advice:
If surgery is proposed, make sure you understand the potential benefits, risks, and the likelihood of visual improvement versus stabilization. It’s important to weigh surgical options carefully with your retina specialist.
Advancements in Diagnosis and Cutting-Edge Treatments
The landscape of CNV care is evolving rapidly, with new diagnostic and therapeutic advances continually emerging.
Modern Diagnostic Technologies
- Optical Coherence Tomography Angiography (OCTA): Noninvasive, dye-free visualization of retinal and choroidal blood flow, allowing early CNV detection.
- Enhanced Depth Imaging OCT: Provides detailed cross-sectional images of the retina and choroid.
New Anti-VEGF Agents and Delivery Methods
- Longer-acting anti-VEGF drugs: Agents like faricimab and port delivery systems offer less frequent dosing while maintaining efficacy.
- Biosimilars: Cost-effective alternatives to existing anti-VEGF agents are expanding access worldwide.
Emerging Therapeutics
- Gene therapy: Trials are underway using viral vectors to induce sustained anti-VEGF production from the retina, aiming to reduce or eliminate injection frequency.
- Cell-based therapy: Experimental stem cell and RPE transplantation for patients with advanced scarring.
- AI-assisted care: Machine learning algorithms for automated OCT analysis and earlier intervention.
Adjunct and Combination Therapies
- Dual-targeting drugs: Medications acting on both VEGF and other angiogenic pathways, showing promise in resistant CNV.
- Photobiomodulation and novel laser modalities: Non-damaging lasers may improve outcomes or reduce injection burden in select patients.
Practical Advice:
Ask your provider about new treatment options, clinical trials, or long-acting medications that could fit your lifestyle and minimize office visits. Consider regular advanced imaging for the earliest detection of recurrence.
Ongoing Clinical Trials and Future Perspectives
The future for patients with CNV is increasingly hopeful, thanks to ongoing research and innovative clinical studies.
Current and Upcoming Clinical Trials
- Gene and cell therapy trials: Promising early results for therapies that may provide long-term control with fewer interventions.
- New drug classes: Research into medications blocking multiple angiogenic signals or targeting inflammation at the root of CNV.
- Novel delivery systems: Port devices, micro-dosing implants, and sustained-release eye drops are all being evaluated.
Research Priorities
- Reducing the need for frequent injections while maintaining or improving vision.
- Earlier diagnosis through AI and tele-ophthalmology.
- Understanding individual risk factors for personalizing therapy.
Participating in a Clinical Trial
- Offers access to the latest treatments, enhanced monitoring, and may advance care for future patients.
- Check for active trials through clinical trial registries or by consulting your retina specialist.
Practical Advice:
If you’re struggling with the frequency or side effects of your current CNV therapy, discuss clinical trial options with your eye doctor. Participation may be a pathway to tomorrow’s breakthroughs today.
Frequently Asked Questions
What is choroidal neovascularization and what causes it?
Choroidal neovascularization (CNV) is the abnormal growth of blood vessels beneath the retina, commonly due to age-related macular degeneration, high myopia, or retinal injury.
How is CNV detected and diagnosed?
CNV is diagnosed using eye exams and imaging, such as OCT, fluorescein angiography, and sometimes OCTA, which reveal abnormal blood vessel growth beneath the retina.
What is the best treatment for CNV?
Anti-VEGF injections are the gold standard for most CNV cases. Other options include photodynamic therapy, laser treatment, or surgery for select patients.
How often do I need anti-VEGF injections for CNV?
Injections are often monthly for the first 3–6 months, then tailored based on disease activity. Some newer drugs allow for less frequent dosing.
Can CNV be cured?
CNV cannot usually be “cured,” but treatments can stop or slow progression, preserve vision, and sometimes improve it, especially with early intervention.
What symptoms of CNV should prompt urgent eye care?
Sudden blurred or distorted vision, new blind spots, or visual changes should prompt immediate evaluation to prevent lasting vision loss.
Are there any new or experimental CNV treatments?
Yes, gene therapies, longer-acting drugs, AI-guided care, and new delivery systems are in advanced development or early clinical use.
Disclaimer:
This article is for educational purposes only and should not substitute for professional medical advice. Please consult your eye care provider for personal recommendations and individualized care.
If you found this guide useful, please share it on Facebook, X (formerly Twitter), or any platform you like—and follow us on social media. Your support helps us keep producing reliable, patient-focused content for all!






