Optic nerve meningioma is a benign tumor that develops from the meninges, the protective membranes that surround the brain and spinal cord. It specifically targets the optic nerve, which is responsible for transmitting visual information from the eyes to the brain. Meningiomas are typically slow-growing and non-cancerous, but their location in the optic nerve can result in significant visual impairment. Optic nerve meningiomas are most commonly diagnosed in middle-aged adults, and women are more likely than men to have them.
Optic nerve meningioma symptoms include progressive vision loss, visual field defects, and, in some cases, proptosis (eye bulging). As the tumor grows, it compresses the optic nerve fibers, causing a gradual decline in visual function. The diagnosis is typically confirmed through a combination of clinical examination and imaging studies, such as magnetic resonance imaging (MRI) and computed tomography (CT) scans, which provide detailed images of the optic nerve and surrounding structures. Understanding the nature and progression of optic nerve meningioma is critical for developing effective treatment plans that preserve vision and improve patient outcomes.
Optic Nerve Meningioma Management and Treatment
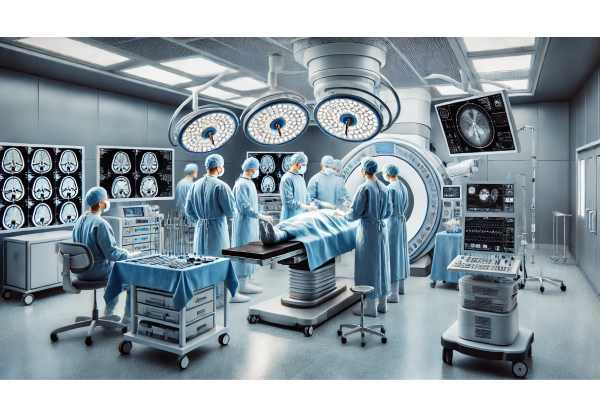
Management and treatment of optic nerve meningioma necessitate a collaborative effort among neuro-ophthalmologists, neurosurgeons, radiation oncologists, and other specialists. The primary goals are to slow tumor growth, preserve or restore vision, and reduce treatment-related side effects. The following are the standard treatment methods for optic nerve meningioma:
- Observation: In cases where the tumor is small and asymptomatic, a watchful waiting approach may be used. Regular monitoring with clinical examinations and imaging studies enables healthcare providers to track tumor progression and intervene if significant growth or worsening of symptoms occurs.
- Surgical Resection: When the meningioma has grown significantly or causes significant visual impairment, surgical removal is considered. The goal of surgery is to remove as much tumor as possible while protecting the optic nerve and surrounding structures. However, complete resection can be difficult due to the delicate nature of the optic nerve and its proximity to critical brain areas. Minimally invasive surgical techniques and advanced microsurgical tools have increased the safety and efficacy of these operations.
- Radiation Therapy: Radiation therapy, which includes stereotactic radiosurgery (SRS) and fractionated stereotactic radiotherapy (FSRT), is frequently used as a substitute or supplement to surgery. These techniques deliver precise radiation doses to the tumor while minimizing damage to surrounding healthy tissues. SRS, such as Gamma Knife or CyberKnife, is especially useful for small tumors or residual tumor tissue after surgery. FSRT is useful for larger or more complex tumors that necessitate a fractional approach.
- Chemotherapy: Because optic nerve meningiomas are typically slow-growing tumors, chemotherapy is rarely used as the primary treatment. However, in some cases where the tumor is aggressive or in patients with recurrent disease, chemotherapy may be considered as part of a comprehensive treatment plan.
- Visual Rehabilitation: Patients who have significant vision loss require visual rehabilitation services. These services include the use of low-vision aids, adaptive devices, and training in techniques to make the best use of residual vision. Vision therapy and rehabilitation can significantly improve a patient’s ability to perform daily activities and overall quality of life.
- Regular Follow-Up and Monitoring: Patients with optic nerve meningioma require continuous follow-up. Regular clinical examinations and imaging studies help to monitor the tumor’s status, evaluate treatment efficacy, and detect any signs of recurrence early.
Breakthrough Treatments for Optic Nerve Meningioma
Recent advances in medical research and technology have resulted in novel approaches that provide new hope for patients with optic nerve meningioma. These cutting-edge innovations include advanced imaging techniques, targeted therapies, immunotherapy, genetic research, and integrated care models. Each of these innovations has distinct advantages and the potential to improve the management of optic nerve meningioma.
Advanced Imaging Techniques
Imaging technology advancements have greatly improved the diagnosis and monitoring of optic nerve meningiomas. High-resolution imaging modalities provide detailed visualization of the optic nerve and surrounding structures, enabling early detection and precise assessment of tumor characteristics.
Magnetic Resonance Imaging (MRI): MRI is still the gold standard for detecting and monitoring optic nerve meningiomas. Advanced MRI techniques, such as diffusion tensor imaging (DTI) and functional MRI (fMRI), provide information about the tumor’s effects on adjacent brain structures and neural pathways. These imaging modalities allow clinicians to better plan treatment strategies and monitor treatment response.
Positron Emission Tomography (PET): PET imaging, often in conjunction with MRI, can reveal metabolic information about the tumor. PET scans with tracers like fluorodeoxyglucose (FDG) can help distinguish between benign and malignant lesions and assess tumor activity, thereby guiding treatment decisions.
Targeted Therapies
Targeted therapies represent a significant step forward in the treatment of optic nerve meningiomas. These therapies target specific molecular pathways involved in tumor growth and progression, providing a more personalized and effective treatment approach.
VEGF Inhibitors: Vascular endothelial growth factor (VEGF) inhibitors, such as bevacizumab, block the VEGF pathway, which is frequently overexpressed in meningiomas. By inhibiting this pathway, VEGF inhibitors can reduce tumor vascularity and proliferation. Clinical trials have shown that VEGF inhibitors can help stabilize tumor growth and alleviate symptoms in patients with optic nerve meningioma.
mTOR Inhibitors: The mammalian target of rapamycin (mTOR) pathway is another potential target for treatment in optic nerve meningioma. Everolimus, a mTOR inhibitor, has shown promise in reducing tumor growth by inhibiting cell proliferation and angiogenesis. Ongoing research is looking into the efficacy of mTOR inhibitors in combination with other therapies to improve treatment outcomes.
Immunotherapy
Immunotherapy uses the body’s immune system to combat cancer cells and has emerged as a promising treatment for a variety of tumors, including optic nerve meningiomas.
Checkpoint Inhibitors: Checkpoint inhibitors, such as pembrolizumab and nivolumab, inhibit proteins that prevent the immune system from attacking cancer cells. These drugs have shown efficacy in treating other types of brain tumors and are being studied for their potential use in optic nerve meningiomas. Checkpoint inhibitors may aid in tumor growth control and patient outcomes by boosting the immune response.
CAR-T Cell Therapy: Chimeric antigen receptor (CAR) T-cell therapy involves genetically modifying a patient’s T cells so that they target specific tumor antigens. This personalized immunotherapy has demonstrated remarkable success in treating certain blood cancers and is being investigated for solid tumors, including meningiomas. CAR-T cell therapy for optic nerve meningiomas is still in the early stages of development, but it shows great promise for the future.
Genetic Research and Therapy
Genetic research has revealed important details about the molecular underpinnings of optic nerve meningiomas, paving the way for targeted genetic therapies.
Genetic Testing: Identifying specific genetic mutations linked to optic nerve meningiomas can aid in predicting the risk of developing the condition and guiding personalized treatment strategies. Genetic testing enables early detection and personalized therapies that address the underlying genetic defects.
Gene Therapy: Gene therapy seeks to correct or modify the genetic mutations that cause tumor growth. While still experimental, gene therapy has the potential to treat optic nerve meningiomas by directly targeting the underlying genetic abnormalities. CRISPR-Cas9 gene editing techniques are being investigated as a means of selectively altering tumor cells, which may lead to a future cure.
Integrative and Complementary Approaches
Integrative approaches combine conventional medical treatments with complementary therapies to provide comprehensive care to patients with optic nerve meningioma.
Acupuncture: Acupuncture is being investigated for its ability to relieve symptoms and improve quality of life in patients receiving treatment for optic nerve meningiomas. According to some studies, acupuncture may help reduce pain, nausea, and fatigue, making it a useful addition to traditional therapies.
Herbal Medicine: Certain herbal remedies, such as ginkgo biloba and turmeric, have been studied for their potential benefits in improving overall health and lowering inflammation. While more research is needed, herbal medicine may provide a complementary approach to managing symptoms and improving well-being in patients with optic nerve meningioma.
Personalized Medicine
Personalized medicine tailors treatment plans to each patient’s unique characteristics, including genetics, lifestyle, and disease manifestations.
Precision Medicine: Advances in genetic testing and molecular diagnostics have enabled the development of precision medicine approaches to optic nerve meningiomas. Understanding the genetic and molecular underpinnings of the condition allows clinicians to create personalized treatment plans that target the specific pathways involved in tumor growth and progression.
Lifestyle and Nutritional Interventions: Personalized medicine emphasizes the importance of lifestyle and nutrition in treating optic nerve meningiomas. Patients can benefit from personalized dietary recommendations, exercise plans, and stress management techniques that are tailored to their specific needs and health profiles.
Artificial Intelligence, Machine Learning
The application of artificial intelligence (AI) and machine learning (ML) in oncology has the potential to revolutionize the treatment of optic nerve meningiomas.
AI-Powered Diagnostics: Artificial intelligence algorithms can analyze large datasets of imaging and clinical data to identify patterns and predict disease progression. AI-powered diagnostics can improve the accuracy and efficiency of diagnosing optic nerve meningiomas, allowing for earlier intervention and personalized treatment strategies.
Predictive Modeling: Machine learning models can forecast the likelihood of complications and guide treatment decisions based on individual patient data. Predictive modeling enables clinicians to create proactive management plans for patients with optic nerve meningioma, thereby improving long-term outcomes.






