What is traumatic uveitis?
Traumatic uveitis is an inflammation of the uveal tract of the eye, which includes the iris, ciliary body, and choroid, caused by ocular trauma. This condition can result from blunt force, penetrating injuries, or chemical exposure, causing inflammation that, if not treated promptly and effectively, can significantly impair vision. Pain, redness, blurred vision, photophobia (light sensitivity), and floaters are common symptoms of traumatic uveitis. Depending on the location and severity of the trauma, the inflammation can affect the anterior segment (iritis), the intermediate segment (cyclitis), or the posterior segment (choroiditis).
The pathophysiology of traumatic uveitis is complex, with immune responses triggered by the initial injury. The trauma disrupts the blood-ocular barrier, allowing inflammatory cells and mediators to enter the uveal tissues, resulting in swelling and tissue damage. This inflammation can lead to secondary complications like glaucoma, cataracts, retinal detachment, and optic neuropathy, all of which impair vision.
Traumatic uveitis is diagnosed using a detailed patient history and a thorough eye examination, which includes slit-lamp biomicroscopy to assess anterior segment inflammation and fundoscopic examination to evaluate posterior segment involvement. Ancillary tests such as optical coherence tomography (OCT), fluorescein angiography, and ultrasonography may be used to assess the severity of the inflammation and its complications. Prompt recognition and management are critical for avoiding permanent vision loss and other serious ocular consequences.
Traumatic Uveitis: Typical Management and Treatment
The goal of managing and treating traumatic uveitis is to reduce inflammation, alleviate symptoms, avoid complications, and preserve vision. Standard treatment methods include a combination of pharmacological and supportive measures based on the severity and location of the inflammation.
Corticosteroids
Corticosteroids are the cornerstone of traumatic uveitis treatment due to their potent anti-inflammatory properties. They can be administered in a variety of ways, depending on the severity and extent of the inflammation.
- Topical Corticosteroids: Eye drops containing prednisolone acetate or dexamethasone are frequently used to treat anterior uveitis. They help to reduce inflammation, pain, and redness.
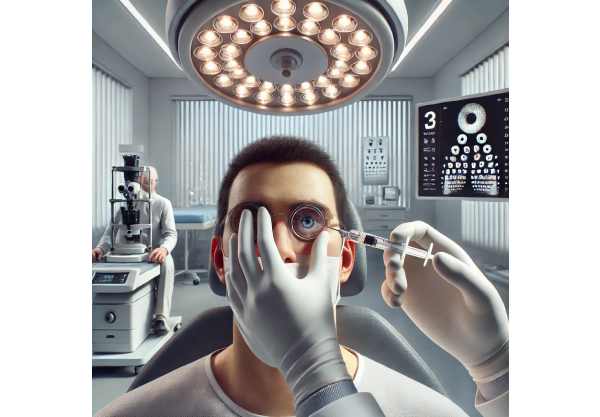
- Periocular or Intravitreal Corticosteroids: For more severe or posterior segment involvement, periocular injections (e.g., triamcinolone acetonide) or intravitreal injections may be required to deliver higher doses of the drug directly to the inflamed tissues.
- Systemic Corticosteroids: In cases of severe inflammation or when topical and local treatments fail, oral or intravenous corticosteroids may be used to achieve systemic anti-inflammatory effects.
Cycloplegic Agents
Cycloplegic agents, like atropine or cyclopentolate, are used to relax the ciliary muscle and dilate the pupil. This relieves pain by reducing muscle spasms and preventing posterior synechiae (adhesions between the iris and lens).
Nonsteroidal anti-inflammatory medications (NSAIDs)
NSAIDs, such as topical ketorolac or oral ibuprofen, can be used in addition to corticosteroids to reduce inflammation and pain. They reduce the production of prostaglandins, which are important mediators of inflammation.
Supportive Care
Supportive care measures are necessary to supplement medical treatment and improve patient comfort:
- Cold Compresses: Putting cold compresses on the affected eye can help relieve pain and swelling.
- Sunglasses: Wearing sunglasses can help relieve photophobia and protect your eyes from bright light.
- Rest and Hydration: Getting enough rest and hydration helps the body’s healing process and overall comfort.
Monitoring and Follow-up
Regular monitoring and follow-up visits are essential for assessing the response to treatment, adjusting therapy as needed, and detecting complications early. This typically entails multiple ocular examinations, such as visual acuity testing, intraocular pressure measurements, and imaging studies, to determine the extent of the inflammation and any structural damage.
Innovative Traumatic Uveitis Treatments
Recent advances in the treatment of traumatic uveitis have introduced novel approaches that improve the efficacy, safety, and convenience of managing this condition. These cutting-edge innovations include novel drug delivery systems, advanced pharmacological agents, and emerging technologies in regenerative medicine and diagnostics.
Sustained-release drug delivery systems.
Intravitreal Implants
Sustained-release intravitreal implants deliver corticosteroids or other anti-inflammatory agents directly into the vitreous cavity over time. Examples are the dexamethasone implant (Ozurdex) and the fluocinolone acetonide implant (Retisert). These implants provide numerous advantages:
- Prolonged Drug Delivery: They maintain a consistent concentration of the drug, reducing the need for frequent administration and increasing patient compliance.
- Targeted Treatment: Direct delivery to the vitreous cavity maximizes therapeutic efficacy while reducing systemic side effects.
- Efficacy in Refractory Cases: These implants are especially useful when other treatments have failed to control inflammation.
Biological Agents
Biologic agents, such as TNF inhibitors and IL blockers, are being investigated for their ability to modulate the immune response in traumatic uveitis. These agents specifically target inflammatory cytokines, offering a more targeted approach to reducing inflammation. Adalimumab and infliximab are two examples of treatments that have shown promise for refractory uveitis.
JAK inhibitors
Janus kinase (JAK) inhibitors, such as tofacitinib, are a new class of drugs that inhibit the JAK-STAT signaling pathway, which is involved in the inflammatory response. These inhibitors have shown promise in reducing inflammation in autoimmune and inflammatory conditions, and they are being tested for use in traumatic uveitis.
Stem Cell Therapy
Stem cell therapy is a new field that shows great promise for regenerating damaged ocular tissues and restoring vision in traumatic uveitis patients. Stem cells can differentiate into different cell types and secrete neurotrophic factors, which aid in tissue repair and inflammation reduction. Experimental studies have shown that transplanting stem cells into the eye can promote healing and improve vision.
Genetic Therapy
Gene therapy, which involves delivering genetic material into cells to correct or modify gene expression, is a novel approach to treating uveitis. CRISPR-Cas9 and viral vector-mediated gene delivery are being investigated to improve immune modulation and tissue repair. For example, gene therapy can be used to increase anti-inflammatory cytokines or inhibit pro-inflammatory pathways, reducing inflammation and preserving vision.
Optical Coherence Tomography (OCT
Optical coherence tomography (OCT) is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina and choroid. OCT enables detailed visualization of structural changes and inflammation, which aids in the diagnosis and management of traumatic uveitis. Recent advances in OCT technology, such as swept-source OCT and OCT angiography, improve imaging capabilities and provide important insights into disease pathophysiology.
Fluorescein Angiography
Fluorescein angiography involves injecting a fluorescent dye into the bloodstream and taking images of the retinal vasculature. This technique evaluates blood flow and vascular integrity, which is critical in detecting inflammatory changes and complications like retinal vasculitis and macular edema.
Genetic Testing
Advances in genetic testing and personalized medicine open up new possibilities for tailoring treatment strategies to individual patients. Genetic testing can detect specific genetic mutations or polymorphisms linked to an increased risk of uveitis or poor treatment response. This data can help guide the selection of targeted therapies and improve treatment protocols.
Biomarker Discovery
Biomarkers are measurable indicators of biological processes or therapeutic responses that can help diagnose, monitor, and treat uveitis. Novel biomarkers of uveitis are being investigated, including inflammatory cytokines, neurotrophic factors, and microRNAs. These biomarkers can help researchers understand disease mechanisms, predict treatment outcomes, and guide personalized therapeutic approaches.
AI-Driven Diagnostics
AI and machine learning algorithms are revolutionizing the diagnosis and treatment of traumatic uveitis. AI can analyze massive amounts of imaging and clinical data to identify patterns and detect early signs of uveitis. These tools can help clinicians make accurate diagnoses, predict disease progression, and create personalized treatment plans.
Predictive Analytics
Machine learning models can predict the risk of complications and treatment outcomes based on patient-specific information. Predictive analytics can help guide clinical decisions, optimize treatment plans, and improve patient care. Healthcare providers can provide more precise and effective interventions for patients suffering from traumatic uveitis by combining AI-powered diagnostics and predictive analytics.
Telemedicine & Remote Monitoring
Remote Consultations
Telemedicine platforms enable remote consultations with ophthalmology specialists, ensuring timely access to expert care, particularly for patients in underserved areas. This approach allows for early diagnosis and ongoing management without the need for frequent in-person visits.
Wearable Devices
Wearable devices with sensors can track ocular parameters like intraocular pressure and inflammation in real time. These devices can send data to healthcare providers, enabling continuous monitoring and timely interventions.






