Blowout fractures are among the most common facial injuries, typically resulting from trauma to the eye socket. These fractures often involve the thin bones of the orbital floor or medial wall, leading to symptoms such as swelling, double vision, eye movement restriction, and facial numbness. Prompt recognition and targeted treatment are essential to restore function, prevent long-term complications, and achieve the best possible cosmetic and visual outcomes. This comprehensive guide explores the condition’s underlying causes, evidence-based therapies, surgical approaches, breakthrough technologies, and future directions, empowering patients and clinicians with actionable, up-to-date information for effective blowout fracture management.
Table of Contents
- Condition Insights and Prevalence: Anatomy, Causes & Risk Patterns
- Initial Medical Care and Standard Therapies
- Operative Techniques and Reconstructive Options
- Recent Technological Advancements in Diagnosis and Repair
- Ongoing Research and Clinical Trials
- Frequently Asked Questions
Condition Insights and Prevalence: Anatomy, Causes & Risk Patterns
A blowout fracture occurs when blunt trauma—often from sports injuries, assaults, or accidents—impacts the orbital rim, transferring force to the thin bones forming the eye socket’s floor or medial wall. This causes these delicate bones to break, potentially allowing orbital contents to herniate into adjacent sinuses.
Key Points:
- Orbital Floor: The most frequently involved site due to its thin structure and proximity to the maxillary sinus.
- Medial Wall: The next most common, adjacent to the ethmoid sinus.
- Common Causes: Punches, falls, ball injuries, car accidents.
Epidemiology:
- Blowout fractures account for up to 50% of all orbital injuries.
- Males aged 10–30 are most commonly affected, particularly in urban and sports environments.
- Children’s “trapdoor” fractures may present differently, with less visible displacement but a higher risk of muscle entrapment.
Clinical Features:
- Swelling, bruising, and tenderness around the eye.
- Double vision (diplopia), often worse with upward or downward gaze.
- Restricted eye movement, especially upward (inferior rectus muscle involvement).
- Numbness of the cheek and upper lip (infraorbital nerve injury).
- Enophthalmos (sunken eye) or visible asymmetry if not treated.
Practical Advice:
After any facial trauma, prompt assessment by a healthcare professional is vital. Do not ignore double vision, severe swelling, or difficulty moving the eye—these require urgent evaluation.
Initial Medical Care and Standard Therapies
Immediate, appropriate care is the cornerstone of successful blowout fracture management, especially to prevent complications such as persistent double vision or disfigurement.
Key Initial Steps:
- Assessment and Imaging:
- Perform a careful eye exam for vision, pupil response, and eye movement.
- Order a CT scan of the orbits and facial bones to define fracture extent and muscle involvement.
- Acute Symptom Management:
- Apply cold packs to reduce swelling.
- Instruct the patient to avoid nose blowing, which can force air into the orbit and worsen swelling.
- Elevate the head and rest.
- Prescribe oral antibiotics (such as amoxicillin-clavulanate) if there is communication with the sinuses to prevent infection.
- Consider a short course of oral corticosteroids for severe swelling.
- Pain Control:
- Use acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) for pain.
- Avoid aspirin (which can increase bleeding risk).
Conservative vs. Surgical Management:
- Conservative management is possible for minor, non-displaced fractures without muscle entrapment or significant enophthalmos.
- Urgent surgery is recommended if:
- There is muscle entrapment with persistent diplopia.
- The eye cannot move fully, or symptoms do not resolve with time.
- There is significant cosmetic deformity or risk of long-term dysfunction.
Home Care and Monitoring:
- Advise patients to watch for signs of worsening vision, severe pain, or new symptoms, and return promptly if they occur.
Practical Advice:
Follow all post-injury instructions closely. Even after mild trauma, new or persistent double vision or numbness should always be reassessed.
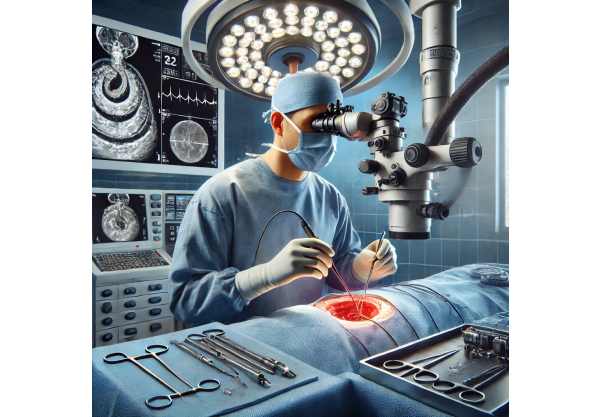
Operative Techniques and Reconstructive Options
Surgical intervention is indicated for selected cases where functional or cosmetic outcomes are threatened. Advances in surgical techniques continue to improve results and reduce recovery times.
Main Surgical Approaches:
- Transconjunctival Approach:
- Accesses the fracture through the inner eyelid, minimizing visible scarring.
- Used for orbital floor or medial wall repairs.
- Subciliary Approach:
- Involves an incision just below the lower eyelashes, providing excellent exposure but with a small risk of visible scar or lid malposition.
- Endoscopic Endonasal Approach:
- For medial wall fractures, endoscopic techniques through the nasal passages can repair the wall with less external trauma.
Implants and Grafts:
- Materials:
- Porous polyethylene (Medpor), titanium mesh, autologous bone grafts, and resorbable plates.
- Choice depends on defect size, surgeon preference, and patient-specific needs.
- Goals:
- Restore normal orbital volume and position.
- Release entrapped tissues and ensure eye movement is fully restored.
Intraoperative Navigation:
- Image-guided systems increase precision, especially for complex fractures.
Postoperative Care:
- Elevate the head to reduce swelling.
- Ice packs for comfort.
- Topical antibiotics and lubricants.
- Avoid trauma or nose blowing for several weeks.
Potential Complications:
- Persistent diplopia, infraorbital numbness, implant infection, or displacement.
- Most patients experience improved eye position and function after timely, expert repair.
Practical Advice:
Choose a surgeon with experience in orbital trauma. Early repair (within 2 weeks) usually provides the best chance for full recovery.
Recent Technological Advancements in Diagnosis and Repair
Modern imaging, surgical planning, and new biomaterials have revolutionized the management of blowout fractures, leading to improved outcomes and fewer complications.
Diagnostic Innovations:
- High-Resolution CT & 3D Reconstruction:
- Allow precise mapping of fractures, aiding in surgical planning and preoperative simulation.
- 3D Printing:
- Patient-specific orbital implants are now created from CT data, ensuring optimal fit and function.
- Intraoperative Navigation:
- Computer-assisted navigation guides the surgeon, minimizing errors and enhancing safety.
New Surgical Materials:
- Biodegradable Implants:
- These provide temporary support as natural bone heals, eliminating long-term foreign body risks.
- Titanium Mesh with Preformed Contours:
- Combines strength with flexibility for tailored reconstruction.
Regenerative Medicine and Tissue Engineering:
- Stem Cell and Growth Factor Applications:
- Early research explores promoting natural bone regeneration and improving healing rates.
Postoperative Monitoring:
- AI-Assisted Imaging Analysis:
- Artificial intelligence tools help monitor healing and detect subtle complications early.
Practical Advice:
Ask about the use of custom implants, minimally invasive techniques, and advanced imaging at your surgical center. These technologies often translate into quicker recovery and better function.
Ongoing Research and Clinical Trials
Research continues to expand treatment options and optimize outcomes for blowout fracture patients, focusing on both functional and cosmetic recovery.
Key Research Topics:
- Timing of Surgery:
- Studies examine the optimal window for intervention to maximize success while minimizing risks.
- Comparative Outcomes:
- Trials compare different materials (e.g., titanium vs. biodegradable plates) and techniques.
- Regenerative Therapies:
- Testing bone growth factors, scaffolds, and stem cell therapies to enhance healing.
Patient Outcomes:
- Quality of life, return to normal activity, and patient satisfaction are increasingly prioritized in research studies.
How to Participate:
- Discuss ongoing clinical trials with your specialist or visit national clinical trial registries for opportunities to join.
Future Directions:
- Integration of virtual reality for surgical planning and training.
- Advanced imaging combined with AI to personalize treatment.
Practical Advice:
Stay engaged in your care—ask your provider about the latest studies, and consider participating in research that may help shape the future of blowout fracture management.
Frequently Asked Questions
What is the best treatment for a blowout fracture?
Treatment depends on severity. Minor cases may heal without surgery; severe or symptomatic fractures often require surgical repair to restore function and appearance.
How long does it take to recover from a blowout fracture?
Recovery ranges from a few weeks for mild cases to several months for severe or surgically treated fractures. Regular follow-up ensures optimal healing.
Is surgery always necessary for a blowout fracture?
Not always. If eye movement is normal and there’s no significant deformity or muscle entrapment, conservative management is appropriate. Surgery is needed if symptoms persist or worsen.
What are the signs I need urgent treatment for a blowout fracture?
Signs include persistent double vision, restricted eye movement, visible eye sinking, severe pain, or numbness. These warrant prompt specialist evaluation.
Can a blowout fracture affect my vision permanently?
Most patients recover well, but untreated muscle entrapment or severe fractures can lead to lasting double vision or cosmetic issues. Early care is crucial for the best outcome.
Are new materials or technologies improving blowout fracture repair?
Yes, advances like custom 3D-printed implants, AI-guided surgery, and new biomaterials have improved precision, reduced complications, and accelerated recovery.
What should I avoid after a blowout fracture?
Avoid nose blowing, heavy lifting, or trauma to the area until cleared by your doctor. Follow all post-op instructions and attend follow-up visits as advised.
Disclaimer:
This article is for educational purposes only and should not be used as a substitute for professional medical advice. Always consult a qualified healthcare provider for guidance specific to your situation.
If you found this article valuable, please share it on Facebook, X (formerly Twitter), or your preferred platform, and follow us for more expert content. Your support helps us continue to produce trusted, up-to-date health information.






