Post-surgical glaucoma, also known as secondary glaucoma after ocular surgery, is a condition characterized by elevated intraocular pressure (IOP) that develops as a result of eye surgeries such as cataract extraction, corneal transplantation, or vitreoretinal procedures. If not treated properly, this increase in IOP can cause optic nerve damage and vision loss. Post-surgical glaucoma can develop due to a variety of factors, including inflammation, mechanical obstruction, or changes in the eye’s fluid dynamics after surgery.
Post-surgical glaucoma symptoms are similar to primary glaucoma and may include eye pain, redness, blurred vision, halos around lights, and, in severe cases, nausea and vomiting. Patients who have had eye surgery must be closely monitored for any signs of elevated IOP to ensure early detection and timely intervention.
A thorough eye examination is required to diagnose post-surgical glaucoma. This includes measuring intraocular pressure with tonometry, evaluating the optic nerve head with ophthalmoscopy, and assessing the anterior chamber angle with gonioscopy. Advanced imaging techniques, such as optical coherence tomography (OCT), can also be used to assess the severity of optic nerve damage.
Understanding postoperative glaucoma and its potential complications is critical for both patients and healthcare providers. Early detection and appropriate management can prevent significant vision loss and improve long-term outcomes for people with this condition.
Standard Treatments for Post-Surgical Glaucoma
Managing post-surgical glaucoma necessitates a multifaceted approach that includes medical therapy, laser treatment, and surgical intervention tailored to each patient’s specific needs. The primary goal is to lower intraocular pressure in order to prevent optic nerve damage and preserve vision.
Medical Therapy
Topical medications to lower intraocular pressure are frequently used as the first line of treatment for post-surgical glaucoma. These medications can be divided into several categories:
- Prostaglandin Analogs: Drugs like latanoprost, bimatoprost, and travoprost increase the outflow of aqueous humor, which lowers IOP.
- Beta-Blockers: Timolol and betaxolol reduce aqueous humor production, which effectively lowers IOP.
- Alpha Agonists: Medications such as brimonidine decrease aqueous humor production while increasing uveoscleral outflow.
- Carbonic Anhydrase Inhibitors: Topical agents like dorzolamide and brinzolamide, as well as oral acetazolamide, inhibit aqueous humor production.
- Rho Kinase Inhibitors: Netarsudil works by increasing trabecular outflow while decreasing episcleral venous pressure.
Combination eye drops containing two different classes of medications are also frequently prescribed to improve IOP control.
Laser Treatment
If medical therapy is insufficient to control IOP, laser treatments may be used. There are two main types of laser procedures for post-surgical glaucoma:
- Selective Laser Trabeculoplasty (SLT): This procedure focuses on the trabecular meshwork to improve aqueous humor outflow. SLT is noninvasive and can be repeated as needed.
- Laser Peripheral Iridotomy (LPI): Typically performed in angle-closure glaucoma, LPI creates a small opening in the iris to allow fluid to flow more freely within the eye.
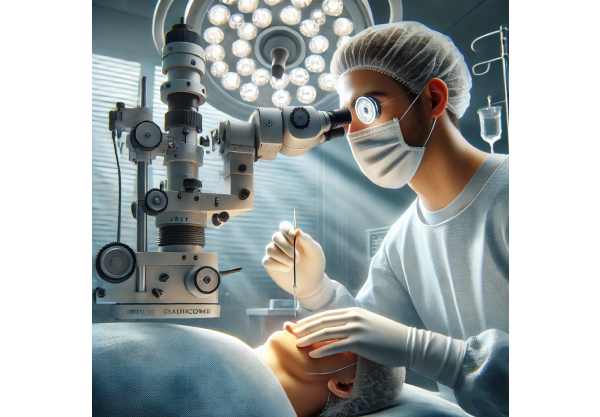
Surgical Intervention
Patients who do not achieve adequate IOP control with medical or laser therapies may require surgical intervention. Surgery options include:
- Trabeculectomy: This procedure creates a new drainage pathway for aqueous humor to exit the eye, thereby lowering IOP. A flap is formed in the sclera, and a small portion of the trabecular meshwork is removed to allow fluid outflow.
- Glaucoma Drainage Devices: Implants such as the Ahmed, Baerveldt, or Molteno devices redirect aqueous humor to an external reservoir, lowering IOP. These devices are especially useful in complex or refractory cases.
- Minimally Invasive Glaucoma Surgery (MIGS): MIGS procedures, such as the implantation of micro-stents (e.g., iStent, Hydrus) or trabecular meshwork bypass procedures (e.g., Trabectome), are less invasive and require less recovery time than traditional surgeries.
Post-operative Care
Postoperative management is critical to ensuring successful outcomes in patients undergoing surgery for post-surgical glaucoma. This includes:
- Anti-inflammatory and Antibiotic Therapy: After surgery, patients are usually given topical steroids and antibiotics to reduce inflammation and prevent infection.
- Regular Monitoring: Frequent follow-up visits are required to monitor IOP, assess healing progress, and detect complications early.
- Patient Education: Educating patients on the importance of following medication regimens, recognizing symptoms of elevated IOP, and attending scheduled follow-up appointments is critical for long-term success.
Innovative Post-Surgical Glaucoma Treatment Options
Recent medical research and technology advances have significantly improved the treatment landscape for post-surgical glaucoma. These cutting-edge developments provide more effective, safer, and minimally invasive treatments for this complex condition.
Microinvasive Glaucoma Surgery(MIGS)
Microinvasive glaucoma surgery (MIGS) has transformed the treatment of glaucoma, including post-surgical glaucoma, by providing less invasive options with shorter recovery times and fewer complications than traditional procedures. MIGS procedures seek to improve aqueous humor outflow through a variety of mechanisms:
- iStent and iStent inject: These small stents are placed in the trabecular meshwork to improve fluid outflow and lower IOP. The iStent inject is a second-generation device that enables the implantation of two stents in a single procedure, providing more complete IOP control.
- Hydrus Microstent: This flexible microstent is inserted into Schlemm’s canal to open it up and improve fluid flow. It has been demonstrated to provide significant and sustained IOP reduction.
- XEN Gel Stent: Constructed from a soft, gelatin-like material, the XEN Gel Stent forms a permanent channel through the sclera, allowing aqueous humor to bypass the trabecular meshwork and lower IOP. Its minimally invasive design lowers the risk of complications associated with traditional filtering surgeries.
Sustained-release drug delivery systems.
Drug delivery system innovations have resulted in the development of sustained-release devices that provide long-term IOP control while posing fewer risks. These systems ensure consistent delivery of medication directly to the target site, thereby improving efficacy and patient compliance:
- Durysta: This biodegradable implant provides a steady dose of bimatoprost, a prostaglandin analog, for several months. Durysta is implanted in the anterior chamber and gradually releases medication, reducing the need for daily eye drops.
- iDose TR is an investigational sustained-release implant that delivers travoprost, another prostaglandin analog, directly to the eye for up to a year. Clinical trials have yielded promising results in terms of long-term IOP control.
Advanced Imaging Techniques
Advanced imaging techniques have greatly improved the diagnosis and management of post-surgical glaucoma. These technologies offer detailed insights into the anatomical and functional aspects of the eye, enabling more precise treatment planning:
- Optical Coherence Tomography (OCT): Enhanced-depth imaging OCT (EDI-OCT) provides high-resolution cross-sectional views of the optic nerve head, retina, and anterior segment. This enables the detection of subtle changes in the optic nerve and retina, allowing for early intervention.
- Anterior Segment OCT: This imaging modality provides detailed views of the anterior chamber angle and structures, which aids in determining angle anatomy and the effectiveness of MIGS devices.
- Confocal Scanning Laser Ophthalmoscopy (CSLO): CSLO generates three-dimensional images of the optic nerve head and retina, allowing for accurate measurement of optic nerve damage and disease progression monitoring.
Genetic and biomarker research
Advances in genetic and biomarker research are paving the way for personalized treatment of post-surgical glaucoma. Identifying genetic markers and specific biomarkers associated with the condition can help predict disease progression and treatment response, resulting in more tailored and effective therapeutic strategies.
- Genetic Testing: Researchers have identified several genes linked to glaucoma, including MYOC, OPTN, and CYP1B1. Genetic testing can help identify individuals who are more likely to develop post-surgical glaucoma, allowing for earlier intervention and personalized treatment plans.
- Biomarker Analysis: Biomarkers such as optic nerve head morphology, retinal nerve fiber layer thickness, and aqueous humor composition are being investigated in order to predict disease progression and treatment response. Analyzing these biomarkers can aid in treatment decisions and improve patient outcomes.
Artificial Intelligence, Machine Learning
Artificial intelligence (AI) and machine learning are transforming ophthalmology, including the treatment of post-surgical glaucoma. AI algorithms can identify patterns and predict disease progression by analyzing large datasets containing imaging studies, clinical records, and genetic information. This capability enables early diagnosis, personalized treatment plans, and optimized monitoring strategies.
- AI-Based Diagnostic Tools: AI algorithms can analyze OCT images to identify early signs of optic nerve damage and track disease progression. These tools provide ophthalmologists with valuable insights, allowing for more accurate diagnoses and timely interventions.
- Predictive Modeling: Using individual patient data, machine learning models can predict IOP fluctuations and treatment responses. This aids in tailoring treatment plans to achieve optimal IOP control while preventing vision loss.






