Episcleritis is a common, typically benign inflammation affecting the episclera—the thin layer of tissue covering the white part of the eye. While it often causes redness, mild discomfort, or irritation, most cases resolve on their own or with minimal intervention. However, recurring or persistent episcleritis can signal underlying health issues and affect quality of life. This comprehensive guide explores episcleritis from every angle: understanding its causes, identifying symptoms, navigating evidence-based treatments, and looking at the future of care. Whether you’re managing your own symptoms or supporting someone else, this article will equip you with practical advice and the latest medical insights.
Table of Contents
- What Is Episcleritis and Who Gets It?
- Non-Surgical and Medication Approaches
- Operative and Procedural Considerations
- Breakthrough Technologies and Modern Developments
- Research Studies and the Road Ahead
- Frequently Asked Questions
- Disclaimer
What Is Episcleritis and Who Gets It?
Episcleritis is an inflammation of the episclera, a thin layer of tissue that lies between the conjunctiva (the clear outer membrane) and the sclera (the white part of the eye). It presents as sudden redness, mild soreness, or localized discomfort in one or both eyes. While the appearance can be dramatic, the condition is generally mild and does not threaten vision.
Types of Episcleritis
- Simple episcleritis: The most frequent form, characterized by diffuse redness and irritation.
- Nodular episcleritis: Marked by a raised, localized nodule surrounded by redness.
Pathophysiology
Episcleritis results from immune-mediated inflammation but is rarely linked to serious systemic illness. Blood vessels in the episclera become engorged, leading to redness and discomfort. The condition is self-limited and not infectious.
Epidemiology
- Most cases occur in adults aged 30–50 but can affect all ages.
- Women are affected slightly more often than men.
- Recurrences are not uncommon, and up to one-third of patients may experience repeated episodes.
Risk Factors
- Idiopathic: Most cases occur with no clear cause.
- Autoimmune or connective tissue diseases: A minority of cases are associated with systemic disorders, such as rheumatoid arthritis or lupus.
- Environmental triggers: Stress, minor trauma, or exposure to irritants may play a role.
Key Practical Tips
- Episcleritis is usually painless, unlike scleritis (a deeper, more severe inflammation).
- Vision changes are rare; if present, consult an ophthalmologist promptly.
- If redness persists, recurs, or is accompanied by joint pain or skin rashes, ask your doctor about possible systemic causes.
Non-Surgical and Medication Approaches
Most cases of episcleritis respond well to conservative management or simple medical therapies. Understanding when to use which treatment can help you recover quickly and reduce the risk of recurrence.
Home Remedies and Supportive Care
- Cool compresses: Placing a clean, cool washcloth over the closed eyelids can reduce discomfort and redness.
- Artificial tears: Over-the-counter lubricating drops soothe the eye and help flush out irritants.
- Avoiding triggers: Reduce eye strain, avoid smoke or dust, and take breaks from screens.
Pharmacological Treatment
For persistent or bothersome episodes, medication may be prescribed:
- Topical corticosteroids: Short-term use of low-potency steroid eye drops can quickly reduce inflammation.
Common choices include loteprednol or fluorometholone, used 2–4 times daily for 1–2 weeks. - Nonsteroidal anti-inflammatory drugs (NSAIDs):
- Topical NSAIDs (like ketorolac) are sometimes prescribed for mild inflammation.
- Oral NSAIDs may help in recurrent or nodular episcleritis, especially if pain is present.
- Oral corticosteroids: Rarely needed, but may be considered in severe, recurrent, or systemic cases.
Choosing the Right Therapy
- For most people, artificial tears and patience are enough—episcleritis often resolves in 1–2 weeks without treatment.
- If you experience frequent flare-ups, talk with your ophthalmologist about evaluating for underlying systemic diseases.
Safety and Side Effects
- Always use steroid drops as directed and attend follow-up visits, as overuse can increase eye pressure or risk of infection.
- Long-term steroid use is rarely necessary and should be carefully monitored.
Practical Self-Care Tips
- Wear sunglasses outdoors to protect your eyes from environmental irritants.
- Practice good hygiene, especially when applying or removing eye drops.
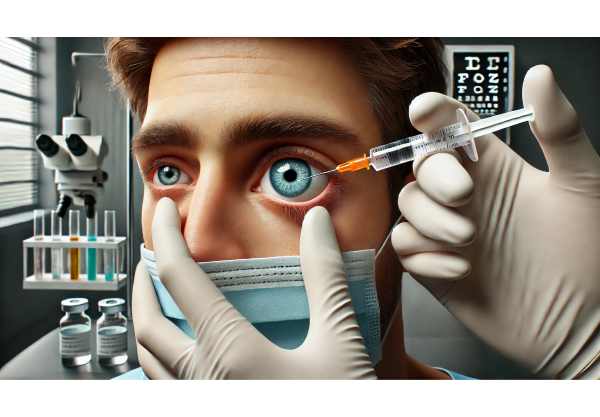
Operative and Procedural Considerations
Unlike many eye disorders, episcleritis rarely requires surgery or invasive procedures. However, understanding when further intervention may be appropriate is helpful—especially in atypical or severe cases.
When Is Surgical Treatment Considered?
- Complicated cases: If symptoms do not resolve with standard therapy, additional work-up or referral to a specialist is warranted.
- Underlying causes: In rare situations where episcleritis is linked to a mass, tumor, or infectious granuloma, minor surgical intervention may be required for diagnosis or treatment.
- Biopsy: Occasionally, a small tissue sample is taken to rule out more serious conditions if symptoms persist despite standard care.
Procedural Adjuncts
- In-office procedures:
- Debridement or removal of a persistent nodule may be performed for nodular episcleritis not responding to medication.
- Laser or device-based treatments:
- Currently, these play no significant role in episcleritis management, though they may be considered for associated ocular surface diseases.
Practical Advice on When to Seek Advanced Care
- If your symptoms are unusually severe, persistent, or associated with vision changes, seek prompt evaluation by an eye specialist.
- Early referral and multidisciplinary collaboration are key for patients with recurrent or atypical presentations.
Breakthrough Technologies and Modern Developments
Advancements in technology are refining how episcleritis is diagnosed and monitored, making care more precise and accessible.
Enhanced Imaging for Accurate Diagnosis
- Anterior segment optical coherence tomography (AS-OCT): This high-resolution imaging tool helps distinguish episcleritis from deeper, more dangerous conditions like scleritis.
- Digital slit-lamp photography: Allows detailed documentation and tracking of inflammation over time.
AI-Driven Diagnostic Aids
- Recent developments include artificial intelligence platforms that assist in diagnosing red eye conditions. These tools improve early detection, reduce misdiagnosis, and support clinicians in complex cases.
Biologic Therapies and Immunomodulators
- Research is underway into targeted therapies for immune-mediated inflammation. Biologics are not yet standard for episcleritis, but their use in related eye conditions (such as uveitis) may open future possibilities for patients with severe, recurrent disease.
Wearable Technology and Patient Monitoring
- Smart contact lenses and wearable devices are being tested for real-time monitoring of ocular surface health. While still experimental, these innovations may one day help track inflammation and optimize treatment for chronic cases.
Practical Implications
- If you are living with recurrent episcleritis, ask your provider about imaging and monitoring tools that can help tailor your treatment plan.
- Stay informed about the evolving landscape of technology, as many innovations will soon become widely available.
Research Studies and the Road Ahead
While episcleritis is generally mild, research continues to refine our understanding and improve care for those with persistent or complicated cases.
Current and Upcoming Clinical Trials
- Ongoing studies are investigating new topical medications, safer anti-inflammatory agents, and biologic therapies for refractory inflammation.
- Some clinical trials are focused on identifying genetic or molecular markers that may predict recurrence or link episcleritis to systemic diseases.
Pipeline Treatments
- Researchers are developing next-generation steroid-sparing drugs, aiming to control inflammation without the side effects of traditional corticosteroids.
- Controlled-release eye drops and depot drug delivery systems may soon offer longer-lasting relief for chronic cases.
Personalized Medicine and Future Outlook
- Advances in genomics and immune profiling could soon allow for individualized treatment approaches, ensuring the most effective and safest therapy for each patient.
- Integration of AI-powered monitoring and telemedicine will increase access to specialist care, especially in remote or underserved areas.
Getting Involved in Research
- If you experience recurrent or severe episcleritis, ask your eye specialist about participating in clinical trials.
- Patient engagement is vital to advancing our understanding and treatment options for this condition.
Frequently Asked Questions
What is the best treatment for episcleritis?
The best treatment for episcleritis is supportive care, such as artificial tears and cool compresses. Mild cases often resolve without medication, while moderate symptoms may require short-term use of anti-inflammatory eye drops under medical supervision.
Can episcleritis go away on its own?
Yes, episcleritis often resolves on its own within 1–2 weeks. Supportive measures like lubricating drops and avoiding eye irritants can help. Medical treatment is usually only necessary if symptoms are severe or persistent.
Is episcleritis a sign of autoimmune disease?
Most episcleritis cases are idiopathic, meaning they have no known cause. However, recurrent or bilateral episcleritis may indicate an underlying autoimmune or connective tissue disease. Consultation with an ophthalmologist is advised for recurrent episodes.
How do you tell the difference between episcleritis and scleritis?
Episcleritis usually causes mild discomfort and bright red, superficial eye redness. Scleritis is deeper, more painful, and may affect vision. Persistent pain or vision changes should prompt urgent eye specialist evaluation.
Are there any complications from episcleritis?
Complications are rare, as episcleritis is generally mild and self-limiting. Rarely, severe or untreated inflammation can affect deeper eye tissues. Prompt evaluation ensures appropriate care and excludes more serious conditions.
Can I wear contact lenses with episcleritis?
It is best to avoid wearing contact lenses during episodes of episcleritis to prevent further irritation or infection. Resume lens use only after complete resolution and with your doctor’s approval.
When should I see a doctor for episcleritis?
See a doctor if redness is persistent, vision changes occur, or pain is severe. Recurring episodes or association with other health symptoms may also warrant a medical evaluation.
Disclaimer
The information provided in this article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider with questions regarding your health or symptoms. Never ignore professional advice or delay care based on information from this guide.
If this guide was helpful, please share it on Facebook, X (formerly Twitter), or your favorite platform to help others learn more. Support our mission by sharing, following us on social media, and encouraging our team to continue providing quality health information for all.






