Primary intraocular lymphoma (PIOL) is a rare and aggressive cancer that develops within the eye. It is a subtype of primary central nervous system lymphoma (PCNSL) that mostly affects the retina, vitreous, or optic nerve head. PIOL is most commonly a non-Hodgkin’s lymphoma, specifically a diffuse large B-cell type. This condition is most commonly seen in immunocompromised people, such as those with HIV/AIDS or those on long-term immunosuppressive therapy, but it can also affect immunocompetent people.
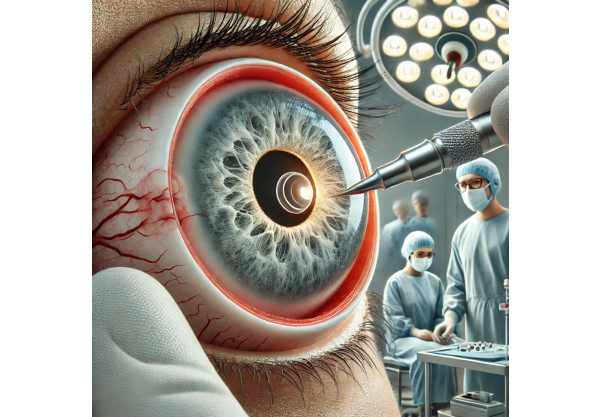
Symptoms of PIOL are frequently nonspecific and can mimic other ocular conditions, making diagnosis difficult. Common symptoms include blurred vision, floaters, eye pain, and photophobia. In some cases, patients may experience redness and inflammation that resemble uveitis, a common misdiagnosis in PIOL cases. The diagnostic process combines clinical examination, imaging studies such as optical coherence tomography (OCT) and magnetic resonance imaging (MRI), and definitive pathological diagnosis via vitreous biopsy or cerebrospinal fluid analysis.
Understanding the pathophysiology of PIOL is critical to effective treatment. Lymphoma cells typically spread from the eye to the brain, making early diagnosis and treatment critical. Given its aggressive nature, PIOL necessitates a collaborative approach involving ophthalmologists, oncologists, and neurologists to provide comprehensive care.
Standard Treatments for Primary Intraocular Lymphoma
Managing primary intraocular lymphoma entails a combination of therapeutic strategies aimed at controlling the local ocular disease while preventing systemic spread, particularly to the nervous system. The most common treatments for PIOL are chemotherapy, radiation therapy, and, in some cases, targeted therapies. Each treatment modality has unique indications, benefits, and potential side effects.
Chemotherapy
Chemotherapy is still the cornerstone of PIOL treatment, with different administration routes designed to maximize therapeutic efficacy while minimizing systemic toxicity. The commonly used chemotherapy approaches include:
- Intravitreal Chemotherapy: This involves injecting chemotherapeutic agents, such as methotrexate or rituximab, directly into the eye’s vitreous cavity. Intravitreal chemotherapy is especially effective at delivering high drug concentrations directly to the tumor site, improving local control while minimizing systemic side effects. However, it necessitates repeated injections and close monitoring for possible complications such as retinal detachment or cataract formation.
- Systemic Chemotherapy: Due to the close relationship between PIOL and central nervous system lymphoma, systemic chemotherapy is frequently used to treat both intraocular and potential CNS involvement. Methotrexate-based regimens with high doses are common, sometimes in combination with other agents such as cytarabine. Systemic chemotherapy can effectively control the disease, but it has a higher risk of systemic toxicity, necessitating ongoing monitoring and supportive care.
- Intrathecal Chemotherapy: In cases with concurrent CNS involvement or a high risk of CNS spread, intrathecal chemotherapy may be used. This involves injecting chemotherapy directly into the cerebrospinal fluid through a lumbar puncture or an Ommaya reservoir. Typical intrathecal agents include methotrexate, cytarabine, and thiotepa.
Radiation Therapy
Radiation therapy is another important aspect of PIOL management, particularly for ocular disease localization. External beam radiation therapy (EBRT) is an effective treatment for intraocular lymphoma cells, reducing tumor burden and alleviating symptoms. However, radiation therapy has the potential to cause radiation retinopathy, optic neuropathy, and cataract formation. To reduce these risks, precise dosing and advanced techniques such as intensity modulated radiation therapy (IMRT) are used.
Targeted Therapy
Targeted therapy is a significant step forward in the treatment of PIOL, focusing on specific molecular targets involved in lymphoma pathogenesis. Rituximab, a monoclonal antibody against CD20, is a popular treatment for PIOL, either alone or in combination with chemotherapy. Rituximab can be given intravitreally or systemically, depending on the severity of the disease.
Other emerging targeted therapies include ibrutinib, a Bruton tyrosine kinase inhibitor, and bortezomib, a proteasome inhibitor. These agents target specific signaling pathways that are essential for lymphoma cell survival and proliferation, providing a more tailored and potentially less toxic treatment approach.
Immunotherapy
Immunotherapy has transformed cancer treatment, and its use in PIOL is a topic of active research. Immune checkpoint inhibitors, like pembrolizumab and nivolumab, have shown promise in treating a variety of cancers, including lymphomas. These agents boost the immune system’s response to cancer cells by blocking inhibitory signals on immune cells. Early clinical trials show that immunotherapy has potential benefits in PIOL, particularly in refractory cases.
Another novel approach to treating PIOL is chimeric antigen receptor (CAR) T-cell therapy. Genetically engineering a patient’s T-cells to express receptors specific to lymphoma antigens improves their ability to recognize and destroy cancer cells. Although still experimental, CAR T-cell therapy holds great promise for the future treatment of PIOL.
Advancements in Diagnostic Techniques
Accurate and timely diagnosis of PIOL is critical for successful treatment. Recent advances in diagnostic techniques have enhanced the ability to detect and monitor this condition:
- Enhanced Imaging Modalities: Advanced imaging technologies, such as enhanced depth imaging optical coherence tomography (EDI-OCT) and ultra-widefield fundus photography, provide detailed visualization of the retinal and vitreous structures, allowing for the detection of subtle lymphoma infiltrates.
- Molecular Diagnostics: Techniques such as polymerase chain reaction (PCR) and next-generation sequencing (NGS) enable the identification of specific genetic mutations and clonal populations associated with lymphoma, allowing for more accurate diagnosis and personalized treatment planning.
Novel Drug Delivery Systems
Drug delivery system innovations have improved the efficacy and safety of chemotherapy in PIOL. This includes:
- Sustained-Release Implants: Intravitreal implants, such as those that release methotrexate or corticosteroids, provide continuous drug delivery over long periods of time, reducing the need for frequent injections and increasing patient compliance.
- Nanoparticle-Based Delivery: Nanotechnology-based drug delivery systems allow for targeted delivery of chemotherapeutic agents to the tumor site, increasing drug concentration while reducing systemic exposure and toxicity.
Future Directions and Research
Ongoing research and clinical trials are exploring new treatment options for PIOL. Areas under active investigation include:
- Combination Therapies: Researchers are looking into the synergistic effects of combining different treatment modalities, such as chemotherapy, targeted therapy, and immunotherapy, to improve therapeutic outcomes and overcome resistance mechanisms.
- Gene Therapy: Gene-editing technologies such as CRISPR/Cas9 are being studied for their ability to correct genetic abnormalities associated with PIOL, providing a potential curative approach.
- Precision Medicine: Personalized treatment strategies based on individual genetic and molecular profiles are being developed to improve treatment efficacy while reducing side effects.






