What is Lens-induced glaucoma?
Lens-induced glaucoma is a type of glaucoma that occurs as a result of changes or abnormalities in the eye’s lens. This condition can result from a variety of lens pathologies, such as lens dislocation, cataract formation, or lens swelling, all of which cause elevated intraocular pressure (IOP). Elevated IOP can damage the optic nerve and cause vision loss if not treated promptly. This condition usually necessitates immediate medical attention to avoid permanent vision impairment.
The Science Behind Lens-Induced Glaucoma
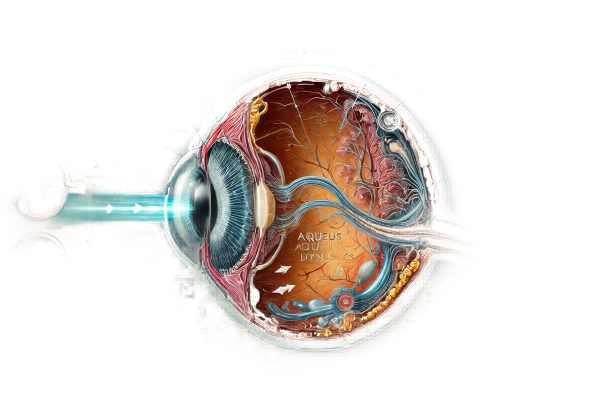
Lens-induced glaucoma is a serious clinical condition that can result in permanent vision loss if not detected and treated promptly. It refers to a group of glaucomas caused by lens abnormalities that disrupt the eye’s aqueous humor dynamics, resulting in increased intraocular pressure. Understanding the various types, mechanisms, and consequences of lens-induced glaucoma is critical for successful management.
Types of Lens-Induced Glaucoma
There are several types of lens-induced glaucoma, each with its own set of pathologies. The primary forms are:
1) Phacomorphic Glaucoma: This type occurs when an intumescent (swollen) cataract blocks the flow of aqueous humor through the pupil, resulting in secondary angle-closure glaucoma. The swollen lens pushes the iris forward, narrowing or closing the anterior chamber angle and preventing aqueous outflow.
- Phacolytic Glaucoma: This condition results from the leakage of lens proteins through an intact but hypermature cataractous lens capsule. The leaked proteins cause inflammation and block the trabecular meshwork, reducing aqueous humor outflow and raising IOP.
- Lens Particle Glaucoma: This type develops after cataract surgery or trauma, when residual lens particles in the anterior chamber cause inflammation and block the trabecular meshwork, resulting in high IOP.
- Phacoanaphylactic Glaucoma: Also known as phacoantigenic glaucoma, this uncommon condition occurs when lens proteins leak into the eye after trauma or surgery, causing an immune response. The resulting inflammation can prevent aqueous humor outflow, raising IOP.
- Ectopia Lentis: This condition occurs when the lens dislocates or subluxates, obstructing the pupil or anterior chamber angle and resulting in elevated IOP. Trauma, congenital conditions such as Marfan syndrome, or systemic diseases can all cause ectopia lentis.
Pathophysiology
The underlying mechanisms of lens-induced glaucoma differ depending on the type, but they typically involve disruption of the aqueous humor outflow pathway. The ciliary body produces aqueous humor, which flows through the pupil and into the anterior chamber before exiting the eye via the trabecular meshwork and Schlemm’s canal. Any obstruction along this pathway can cause an increase in IOP.
- Phacomorphic Glaucoma: The swollen lens physically reduces or closes the anterior chamber angle, preventing aqueous outflow.
- Phacolytic Glaucoma: High-molecular-weight lens proteins leak into the anterior chamber, causing an inflammatory response and trabecular meshwork blockage.
- Lens Particle Glaucoma: Residual lens fragments clog the trabecular meshwork, causing an increase in IOP.
- Phacoanaphylactic Glaucoma: An immune response to lens proteins causes inflammation and trabecular meshwork blockage.
- Ectopia Lentis: Dislocated lenses can obstruct the pupil or cause intermittent angle closure, which disrupts the normal outflow of aqueous humor.
Clinical Presentation
The clinical presentation of lens-induced glaucoma varies according to the type and severity of the condition. Common symptoms include:
- Acute Onset: Sudden vision loss, eye pain, redness, and headache are common symptoms of acute cases such as phacomorphic and lens particle glaucoma.
- Chronic Symptoms: In chronic conditions like phacolytic glaucoma, there may be gradual vision loss, mild eye discomfort, and halos around lights.
- Inflammation: Phacoanaphylactic glaucoma frequently presents with signs of anterior uveitis, such as eye redness, pain, and photophobia.
- Lens Changes: A slit-lamp examination may reveal visible cataract, lens dislocation, or a swollen lens.
- Elevated IOP: Elevated IOP is a feature of all types of lens-induced glaucoma and can be measured during an ophthalmic examination.
Epidemiology and Risk Factors
Lens-induced glaucoma is less common than primary glaucomas, but it is a serious condition because of the risk of rapid vision loss. Risk factors include:
- Age: Older people are more likely to develop cataracts and other lens-related conditions.
- Trauma: Eye injuries can cause lens dislocation or rupture, resulting in lens-induced glaucoma.
- Surgical History: Previous cataract surgery raises the possibility of lens particle glaucoma.
- Systemic Conditions: Diseases like Marfan syndrome, homocystinuria, and Weill-Marchesani syndrome can result in lens dislocation and glaucoma.
Complications
If left untreated, lens-induced glaucoma can cause serious complications, such as:
- Optic Nerve Damage: Prolonged high IOP can damage the optic nerve, resulting in irreversible vision loss.
- Chronic Inflammation: Persistent inflammation can lead to secondary complications like synechiae (adhesions) that further obstruct aqueous outflow.
- Blindness: Advanced cases can lead to total vision loss if not treated promptly and effectively.
Understanding the various forms of lens-induced glaucoma and their underlying mechanisms is critical for timely diagnosis and treatment, resulting in better outcomes for affected individuals.
Methods to Diagnose Lens-Induced Glaucoma
Lens-induced glaucoma diagnosis necessitates a multifaceted approach that includes clinical evaluation, imaging techniques, and specialized tests to confirm the condition and determine the cause.
Clinical Evaluation
- History and Symptoms: A thorough patient history can help identify symptoms like sudden vision loss, eye pain, and previous ocular trauma or surgery. Patients may describe halos around lights, headaches, and redness in the affected eye.
- Visual Acuity Test: Measuring visual acuity helps determine the severity of vision impairment. Significant vision loss may indicate advanced glaucoma.
- Slit-Lamp Examination: This procedure allows the ophthalmologist to examine the anterior segment of the eye, which includes the lens, cornea, and anterior chamber. Signs of lens swelling, dislocation, or particles in the anterior chamber are visible.
Intraocular Pressure Measurement
Measuring IOP is critical in diagnosing glaucoma
- Tonometry: This test determines the pressure within the eye. Elevated IOP is a strong indicator of glaucoma. Goldmann applanation tonometry, non-contact tonometry, and handheld tonometers are examples of commonly used methods.
- Pachymetry: Measuring corneal thickness is critical because it can impact IOP readings. Thicker or thinner corneas can result in inaccurate IOP measurements.
Gonioscopy
Gonioscopy is the use of a special lens to examine the anterior chamber angle, which is where the aqueous humor drains from the eye. This test can detect angle closure, which is common in phacomorphic glaucoma. It can also detect abnormalities in the angle structure, such as synechiae or debris clogging the trabecular mesh.
Optical Coherence Tomography(OCT)
OCT can generate high-resolution cross-sectional images of the retina and optic nerve. This imaging technique detects thinning of the retinal nerve fiber layer, indicating optic nerve damage. OCT can also detect lens-related changes, such as swelling or dislocation, which contribute to glaucoma.
Ultrasound Biomicroscopy (UBM)
UBM is a sophisticated imaging technique that employs high-frequency ultrasound to visualize anterior segment structures such as the lens, ciliary body, and anterior chamber angle. It’s especially useful for detecting lens dislocation and determining the degree of angle closure or blockage.
Anterior Segment Photography
Photographs of the anterior segment can reveal changes in the lens and anterior chamber. This technique aids in monitoring the progression of lens-induced glaucoma and assessing treatment efficacy.
Lab Tests
In cases of suspected phacolytic or phacoanaphylactic glaucoma, testing the aqueous humor for inflammatory cells or lens proteins can provide diagnostic confirmation. These tests aid in distinguishing between different types of lens-induced glaucoma and determining appropriate treatment strategies.
Lens-Induced Glaucoma Treatment
Treating lens-induced glaucoma entails addressing both the elevated intraocular pressure (IOP) and the underlying lens pathology. The treatment approach varies depending on the type of lens-induced glaucoma, its severity, and the patient’s overall health.
Medical Management
- Topical Medications: The first line of treatment is frequently topical eye drops to reduce IOP. This may include:
- Beta-blockers: Lower aqueous humor production (e.g., timolol).
- Prostaglandin analogs: Promote aqueous outflow (e.g., latanoprost).
- Alpha agonists: Reduce aqueous production and increase outflow (for example, brimonidine).
- Carbonic anhydrase inhibitors: Lower aqueous humor production (for example, dorzolamide).
- Miotics: Increase trabecular outflow (such as pilocarpine).
- Systemic Medications: In severe cases, oral or intravenous medications like acetazolamide or mannitol can be used to quickly reduce IOP.
Surgical Interventions
Surgery is frequently required to address the underlying lens pathology and restore normal aqueous humor dynamics.
- Lens Extraction: Removal of the cataractous or swollen lens is the primary treatment for phacomorphic glaucoma. This can be accomplished via:
- Phacoemulsification is the process of ultrasonically fragmenting the lens and aspirating it.
- Extracapsular Cataract Extraction (ECCE): Manual removal of the lens via a larger incision.
- Anterior Chamber Washout: In phacolytic or lens particle glaucoma, this procedure involves irrigating the anterior chamber to remove inflammatory cells and lenses.
- Laser Iridotomy or Iridoplasty: In cases of angle-closure glaucoma, laser procedures can open up the iris to improve aqueous humor outflow or reshape it to widen the anterior chamber angle.
- Trabeculectomy or Glaucoma Drainage Devices: If IOP remains uncontrolled after lens extraction, additional glaucoma surgeries, such as trabeculectomy or the implantation of drainage devices, may be required to facilitate aqueous outflow.
Innovative and Emerging Therapies
- Minimally Invasive Glaucoma Surgery (MIGS): These procedures aim to reduce IOP while causing less trauma than traditional surgeries. Microstents and trabecular meshwork bypass devices are among the techniques used.
- Anti-inflammatory Treatments: Researchers are looking into newer pharmacological agents that target specific inflammatory pathways to reduce the immune response in phacoanaphylactic glaucoma.
- Gene Therapy: Though still in the experimental stage, gene therapy has the potential to address genetic predispositions to lens dislocation or other lens pathologies that cause glaucoma.
- Nanotechnology: Researchers are investigating the use of nanoparticles to deliver medications to the eye more effectively, which could improve outcomes in lens-induced glaucoma.
Post-operative Care
Postoperative care is critical for monitoring IOP, reducing inflammation, and ensuring proper healing. Patients usually use anti-inflammatory and antibiotic eye drops after surgery to prevent infection and inflammation. Regular follow-up visits are required to monitor recovery and detect complications early.
Effective Ways to Improve and Avoid Lens-Induced Glaucoma
- Regular Eye Examinations: Have routine eye exams to detect early changes in the lens and IOP, allowing for timely intervention.
- Control Systemic Conditions: Treat systemic diseases like diabetes, which can hasten cataract formation and complicate glaucoma.
- Avoid Eye Trauma: Keep the eyes safe from injury, which can cause lens dislocation or damage, increasing the risk of lens-induced glaucoma.
- Early Cataract Surgery: Treat cataracts before they grow hypermature and cause complications such as phacolytic or phacomorphic glaucoma.
- Monitor Postoperative Changes: After cataract surgery, look for signs of lens particle glaucoma and seek immediate treatment if symptoms appear.
- Manage Inflammation: Take prescribed anti-inflammatory medications as directed to control any ocular inflammation that may contribute to glaucoma.
- Lead a Healthy Lifestyle: Eat a well-balanced diet high in antioxidants and avoid smoking to improve overall eye health and potentially delay cataract formation.
- Educate on Symptoms: Understand the signs of an acute glaucoma attack, such as sudden vision loss, eye pain, and redness, and seek immediate medical attention.
- Use Eye Protection: Wear protective eyewear when engaging in activities that pose a risk of eye injury to avoid trauma-induced lens dislocation.
Trusted Resources
Books
- “Ophthalmology” by Yanoff and Duker
- “Lens and Cataract” by David F. Chang
- “Glaucoma: Science and Practice” by John C. Morrison and Irvin P. Pollack
Online Resources
- American Academy of Ophthalmology (AAO) – aao.org
- National Eye Institute (NEI) – nei.nih.gov
- Glaucoma Research Foundation – glaucoma.org
- MedlinePlus – Glaucoma – medlineplus.gov






